1. A 58-year-old man is evaluated because of insidious onset of slowly progressive dyspnea over the last 3 years. At this point, he must stop to rest when walking 1 block. Previously, he walked 1 to 2 miles daily without difficulty. He has no cough, chest pain, or orthopnea. He has no other medical problems.
On physical examination, vital signs are normal. Body mass index is 3 5 . 0xygen saturation is 93% breathing ambient air. Dry crackles are noted on auscultation. Cardiac examination shows a parasternal heave and persistent splitting of S2•
Chest radiograph shows diffuse reticular infiltrates that are most prominent in the upper lung zones.
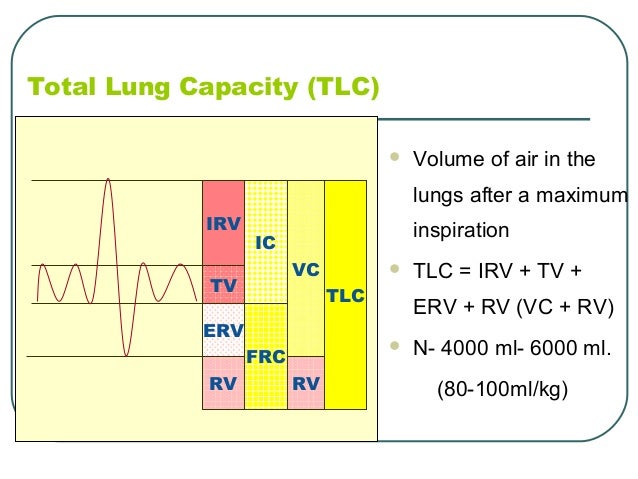
Spirometry shows forced expiratory volume in 1 second (FEV1) that is 60% ofpredicted and an FEV1/forced vital capacity ratio of 80%. Total lung capacity is 70% of expected. Diffusing capacity of carbon monox - ide is 45% ofexpected.
Which of the following is the most likely diagnosis?
(A) Diffuse parenchymal lung disease
(B) Heart failure
(C) Obesity hypoventilation syndrome
(D) Obstructive airways disease
(E) Respiratory muscle weakness
A
2. A 30-year-old man is evaluated for chronic cough that has lasted nearly 1 year. He recalls that the cough began after a "bad cold. " He was treated with a course of a macrolide antibiotic without signifi cant improvement. The cough is nonproductive, is most noticeable at night and on cold days, and sometimes occurs after exercise. He has no postnasal drip, nasal congestion, or heartburn. He does not smoke. He has no history ofoccupational or other exposures. Medical history is otherwise unremarkable except for gastroesophageal reflux for which he takes a daily proton pump inhibitor.
On physical examination, vital signs are normal. The oropharynx is normal, without postnasal drip. Findings on pulmonary examina tion are normal. Spirometry shows forced expiratory volume in 1 sec ond (FEV1) of90% ofpredicted and an FEV1/forced vital capacity ratio of 80%. Chest radiograph is normal.
Which of the following is the most appropriate diagnostic test to perform next?
(A) Bronchial challenge test
(B) Bronchoscopy
(C) Chest computed tomography (D) Pertussis culture
A
Item 6
A 50-year-old man is evaluated in the emergency department for a 3-day history of dyspnea, fever, productive cough, and left-sided pleuritic chest pain. He has been in good health previously and takes no medications.
On examination, temperature is 39°C (102.2°F), blood pressure is 140/80 mm Hg, pulse rate is 105/min, respiration rate is 22/min, and oxygen saturation is 94% on ambient air. Pulmonary examination shows crackles on the left side.
Chest radiograph shows a patchy left lower lobe infiltrate with blunt ing of the costophrenic angle. Left lateral decubitus film shows free flowing fluid that layers out to 8 mm.
Treatment with empiric oral antibiotics is initiated for community acquired pneumonia.
Which of the following is the most appropriate next step in man agement ofthe pleural effusion?
(A) Chest computed tomography
(B) Furosemide
(C) Thoracentesis
(D) Observation
D
Please draw the correct pulmonary lung volumes and capacities
:)
Item 21
A 43 -year-old man is evaluated because of a 3 -year history of exces sive sleepiness. He sleeps 8 hours nightly but never seems to wake refreshed. He reports that his wife complains about his snoring. She also notes that he appears to stop breathing suddenly for several sec onds many times during the night. He resumes breathing with a loud gasp and snort. He falls asleep easily during the day, particularly in meetings or while reading. He has a history of hypertension and pre diabetes. He has a 15-pack-year history ofsmoking but has not used tobacco for the past 8 years. He does not use alcohol. Medications are chlorthalidone and lisinopril. He works as an accountant and is gen erally sedentary.
On physical examination, vital signs are normal. Body mass index is 39. Other than obesity, the remainder of the findings on physical examination are normal.
Which ofthe following is most directly responsible for the patient's symptoms?
(A) History of smoking (B) Hypertension
(C) Sedentary life style (D) Weight
D
Item 1 7 [Basic]
A 72-year-old man is evaluated for follow-up after his first exacer bation ofmoderate chronic obstructive pulmonary disease. The dose of prednisone was tapered, and treatment was stopped 1 week ago. He is afebrile and his cough has decreased. He still has dyspnea despite adherence to the treatment regimen. Medical history is oth erwise unremarkable. He has a 45-pack-year smoking history but stopped 6 months ago. Medications are tiotropium, a salmeterol dry powder inhaler, and an albuterol metered-dose inhaler as needed. He uses albuterol up to six times daily.
On physical examination, vital signs are normal. Pulmonary exam ination shows occasional expiratory wheezes. Oxygen saturation is 94% on ambient air.
Which of the following is the most appropriate next step in man agement?
(A) Add a fluticasone inhaler
(B) Add oxygen therapy
(C) Check the patient's inhaler technique
(D) Resume treatment with prednisone
C
Item 28
A 63-year-old woman is evaluated in the emergency department because of sudden onset of anterior chest pain and shortness of breath. The pain is sharp, is worse with inspiration, and does not r a d i a t e . S h e c a n n o t w a l k m o r e t h a n a few s t e p s w i t h o u t d y s p n e a . T h e medical history is significant for lung cancer that was diagnosed 2 weeks ago. She is undergoing radiation therapy. She has not been hospitalized recently. She has no cough, fever, chills, or hemoptysis. She has a 35-pack-year history of smoking and stopped smoking 3 months ago.
On physical examination, she is afebrile, blood pressure is 110/70 mm Hg, pulse rate is 115/min, respiration rate is 22/min, and oxygen saturation is 84% on ambient air. Findings on cardiopulmonary examination are normal. The extremities are normal, without pain or edema.
The electrocardiogram shows sinus tachycardia with ST-segment depression in leads V3 to V6, unchanged from 2 months ago. The ini tial troponin I level is 0.1 ng/mL (0.1 μg/L) . Chest radiograph shows a right hilar mass that is unchanged from 2 weeks ago.
Which of the following diagnostic tests should be performed next?
(A) Cardiac catheterization
(B) Chest computed tomographic angiography
(C) D-Dimer assay
(D) Dobutamine echocardiographic stress test
(E) Transthoracic echocardiogram
B
Item 4
A 36-year-old woman is evaluated because of shortness of breath. She describes her symptoms as "difficulty getting air" both at rest and with exertion. Onset of symptoms has been gradually progres sive over the last 6 months. She has no cough or wheezing. Medical history is significant for severe injuries sustained in a motor vehicle accident 2 years ago. She had multiple head and chest injuries requir ing prolonged mechanical ventilation and multiple corrective surg eries. She has recovered completely and now feels well. She takes no medications.
On physical examination, vital signs are normal. Oxygen saturation is 99% on ambient air. The oropharynx is patent, and she has no stri dor. The chest shows multiple well-healed surgical incisions; respi ratory effort and chest excursion are normal. The lungs are clear to auscultation. The remainder of the examination is unremarkable.
Which ofthe following is the most appropriate next diagnostic step?
(A) Chest computed tomography
(B) Flow-volume pulmonary function testing
(C) Plain chest radiograph
(D) Ventilation-perfusion scan
B
Item 1 0
A 26-year-old man is evaluated because ofa 6-month history ofchest tightness, cough, and shortness of breath that occur after running. He has no symptoms while running. His symptoms usually start a few minutes after he finishes running and continue for the next 30 minutes. Symptoms are worse when he runs in cold weather. He has no other medical problems and takes no medications.
On physical examination, temperature is 36.5°C (97.7°F), blood pres sure is 120/70 mm Hg, pulse rate is 65/min, respiration rate is 14/min, and oxygen saturation is 98% on ambient air. Body mass index is 21. Pulmonary examination shows good air movement without wheezing.
Office spirometry is normal. After an exercise challenge test, Forced expiratory volume in 1 second decreased by 15% from the baseline measurement obtained before exercise.
Which ofthe following is the most appropriate treatment for this patient?
(A) Inhaled glucocorticoid before exercise
(B) Inhaled long-acting -2-agonist daily
(C) Inhaled short-acting -2-agonist before exercise
(D) Oral Ieukotriene receptor agonist daily
C
Item 9
A 54-year-old woman is evaluated in the emergency department because of a 7-day history of cough and dyspnea. She had fatigue at the onset of symptoms. She reports feeling feverish, with nonpro ductive cough and progressive shortness of breath. Medical history is otherwise unremarkable. She takes no medications.
On physical examination, temperature is 37.9°C (100.3°F), blood pressure is 105/70 mm Hg, pulse rate is 106/min, and respiration rate is 32/min. Oxygen saturation is 92% on ambient air. Lung examination shows dullness to percussion, decreased tactile fremitus, and decreased breath sounds at the right base. The remainder ofthe find ings on physical examination are unremarkable.
Which of the following is the most likely diagnosis?
(A) Heart failure
(B) Lobar consolidation
(C) Pleural effusion
(D) Pneumothorax
C
Draw a flow volume loop that includes normal, restrictive and obstructive. Please explain your drawing
:)
Item 8
A 78-year-old man was admitted to the hospital 4 days ago because
ofdyspnea. He has a history of heart failure.
On physical examination at admission, he was afebrile, blood pressure was 150/88 mm Hg, pulse rate was 108/min, and respiration rate was 22/min. Jugular venous distention was present, there were bibasilar crackles and dullness to percussion at both lung bases, and there was 2 + lower extremity edema. Chest radiograph showed cardiomegaly, vascu lar congestion, and moderate bilateral pleural effusions. He was treated with furosemide but continued to have shortness ofbreath. Thoracentesiswas performed on hospital day 3 for further relief of dyspnea.
Pleural fluid analysis shows a pleural fluid-serum lactate dehydroge nase(LDH)ratioof.52,apleuralfluidLDHlevelof46%oftheupper limit of the normal level, and a pleural fluid-serum total protein ratio of 0 . 4 5 . Results of pleural fluid cultures and cytology are pending.
Which of the following is the most likely cause of this patient's pleural effusions?
(A) Heart failure
(B) Malignancy
(C) Pneumonia
(D) Pulmonary embolism
A
Item 1 6
A 66-year-old man is evaluated because ofslowly progressive short ness of breath and productive cough. He has a 5-year history of chronic obstructive pulmonary disease. He has a 55-pack-year smoking history, but stopped tobacco use 4 years ago. Medications are inhaled salbutamol and inhaled ipratropium. He uses inhaled albuterol as rescue medication. The patient continues to experience limiting dyspnea with activities of daily living. He demonstrates excellent inhaler technique. He reports no change in the color or vol ume of his sputum and does not have fever or chills.
On physical examination, temperature is 37.5°C (99.5°F) , blood pres sure is 128/76 mm Hg, pulse rate is 94/min, respiration rate is 20/min, and oxygen saturation is 82% on ambient air. Body mass index is 20. Heart sounds are distant, and breath sounds are diminished bilater ally and associated with a prolonged expiratory phase.
Spirometry shows Forced expiratory volume in 1 second (FEV1) of 40% of predicted and an FEV1/forced vital capacity ratio of 45%. Chest radiograph shows hyperinflation.
Which ofthe following interventions is most likely to prolong the patient's survival?
(A) Continuous oxygen therapy
(B) Inhaled glucocorticoid therapy
(C) Long-term antibiotic therapy
(D) Pulmonary rehabilitation
A
Item 29
A 54-year-old man is evaluated in the emergency department for a 1-hour history of chest pain and shortness of breath. He had been hospitalized 1 week ago for a colectomy for colon cancer. His med ical history is otherwise significant for hypertension complicated by hypertensive nephropathy. His medications include amlodipine, ramipril, and as-needed acetaminophen for postoperative pain.
On physical examination, temperature is 37.5°C (100°F) , blood pres sure is 110/60 mm Hg, heart rate is 115/min, and respiration rate is 24/min. Oxygen saturation is 89% with the patient breathing ambi ent air and 97% on oxygen, 4 Umin by nasal cannula. The lungs are clear. Cardiac examination shows tachycardia but is otherwise nor mal. There is a surgical incision in the left lower quadrant that is healing well. The remainder of the examination is unremarkable.
Chest radiograph is negative for infiltrates, widened mediastinum, and pneumothorax. Serum creatinine concentration is 2.1 mg/dL (185 . 6 μmol/L) .
Empiric intravenous unfractionated heparin therapy is begun.
Which ofthe following is the most appropriate study to confirm the diagnosis in this patient?
(A) CT angiography
(B) D-dimer assay
(C) Lower extremity Doppler ultrasonography
(D) Ventilation-perfusion scanning
D
Item 24
A 32-year-old woman is evaluated because of slowly progressive dyspnea. For the last 6 months she has experienced progressive exer tional dyspnea, exertional chest pressure, and dry cough. She is now short of breath when climbing one flight of stairs. She has no fever or weight loss. She reports one episode of a painful raised erythe matous lesion on the anterior right shin accompanied by fever and ankle pain 6 months ago that resolved spontaneously after 3 weeks. She does not smoke.
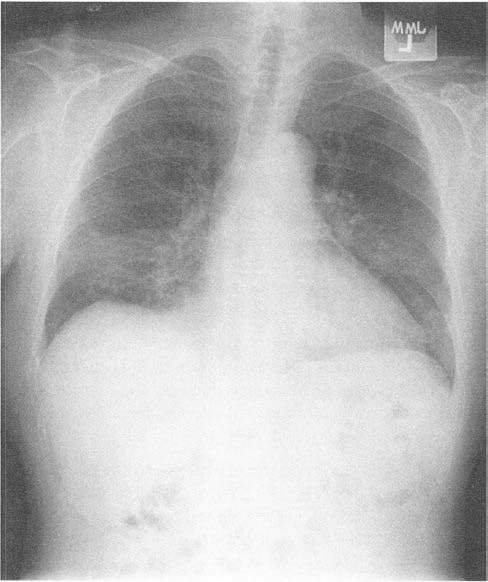
See the Chest radiograph on your paper
On physical examination, she is afebrile, blood pressure is 120/70 mm Hg, pulse rate is 90/min, and respiration rate is 20/min. Body mass index is 23. Skin appears normal. Results of cardiopulmonary examination are normal.
Pulmonary function tests show Forced expiratory volume in 1 sec ond (FEV1) of 75% of predicted, forced vital capacity (FVC) of 88%, total lung capacity of78% ofpredicted, and residual volume of70% of predicted. The FEV/FVC ratio is 68%.
Which of the following is the most likely diagnosis?
(A) Chronic hypersensitivity pneumonitis
(B) Lymphangioleiomyomatosis
(C) Respiratory bronchiolitis-associated interstitial lung disease
(D) Sarcoidosis
D
Item 1 1
A 55-year-old woman is evaluated because of a recent increase in symptoms of asthma characterized by daily cough and dyspnea. She reports waking up two to three nights per week with her typical asthma symptoms. She has no postnasal drip, nasal discharge, fever, or heartburn. Her medications are medium-dose inhaled cortico steroids and albuterol as needed. She demonstrates proper use of her metered-dose inhalers.
On physical examination, she appears comfortable and is in no res piratory distress. Pulse rate is 76/min, and respiration rate is 18/min. Pulmonary examination shows bilateral wheezing. The remainder of the findings on examination are normal.
Which of the following is the most appropriate treatment?
(A) Add a long-acting -2-agonist inhaler
(B) Add an ipratropium metered-dose inhaler
(C) Double the dose of inhaled corticosteroids
(D) Start a 10-day course of a macrolide antibiotic
A
Item 7
A 74-year-old man is evaluated because of progressive dyspnea, productive cough, and left-sided chest pain of lO days' duration. He also reports fever and chills. The medical history includes heart failure. Medications are aspirin, carvedilol, enalapril, and furosemide.
On physical examination, temperature is 39°C (102.2°F),blood pressure is 144/88 mm Hg, pulse rate is 102/min, respiration rate is 28/min, and oxygen saturation is 90% on ambient air. Pulmonary examination shows dullness to percussion and decreased breath sounds over the left posterior thorax. Cardiac examination shows a grade 2/6 holosystolic murmur and a fourth heart sound.
Serumglucose level is 110 mg/dL (6.11 mmol/L) , serum lactate dehy drogenase level is 250 units/L, and serum protein level is 5.8 g/dL (58 g/L).
Chest radiograph shows a moderate left-sided effusion. Thoracentesis yields 500 mL of cloudy-appearing pleural fluid.
Pleural fluid analysis: Blood cell count
Total protein
Lactate dehydrogenase Glucose
pH
Erythrocyte count, 1/μL; leukocyte count, 8900/μL (8.90 x 109/L) with 10% lymphocytes and 85% neutrophils
3.5 g/dL (35 g/L)
160 units/L
25 mg/dL (1.39 mmol/L)
7.10
Which of the following is the most likely cause of the effusion?
(A) Bacterial pneumonia
(B) Heart failure
(C) Malignancy
(D) Tuberculosis
A
Item 5
A 66-year-old man is admitted to the hospital with a 2-month his tory of progressive dyspnea and worsening pedal edema. Medical history is significant for coronary artery bypass surgery 3 years ago. He has a 10-year history of hypertension. Medications are metopro lol, atorvastatin, and aspirin.
On physical examination, temperature is normal, blood pressure is 118/64 mm Hg, pulse rate is 120/min, and respiration rate is 26/min. Jugular venous distention that increases with inspiration is noted. Cardiac examination shows no murmur, rub, or gallop. Pulsus para doxus of 5 mm Hg is present. Lungs are clear to auscultation. Hepatojugular reflux is present. Pedal edema of 2 + is noted.
Electrocardiogram shows sinus rhythm with increased voltage in the precordial leads. Echocardiogram shows a normal left ventricular ejection fraction, restrictive left ventricular filling, increased ven tricular wall thickness, biatrial enlargement, a small pericardia! effu sion, and abnormal diastolic to-and-fro ventricular septa! motion. Chest radiograph shows no infiltrates.
Which ofthe following is the most likely cause ofthis patient's dys pnea?
(A) Cardiac tamponade
(B) Constrictive pericarditis
(C) Restrictive cardiomyopathy
(D) Severe tricuspid regurgitation
B
Item 15
A 36-year-old man is evaluated because ofprogressive shortness of breath over the last 3 years. He has episodic wheezing and decreased exercise capacity when he climbs stairs or walks quickly. He has a 10-pack-year history of smoking, but has not used tobacco for the past 5 years.
His father is 60 years old and has severe emphysema.
On physical examination, vital signs are normal. Oxygen saturation is 95% on ambient air. Body mass index is 22. There is wheezing in the posterior and lower lung fields. The remainder of the findings on physical examination are normal.
Chest radiograph is shown.(see your paper)
Spirometry shows Forced expiratory volume in 1 second (FEV1) of 53% of predicted and an FEV1/forced vital capacity ratio of 64%. Diffusing capacity of carbon monoxide is 67% of predicted. A six minute walking test shows no significant oxygen desaturation while breathing ambient air.
In addition to smoking cessation, which ofthe following is the most appropriate next step in management?
(A) a1-Antitrypsin level measurement
(B) Chest computed tomography
(C) Inhaled glucocorticoid treatment
(D) Oxygen therapy
A
Item 30
A 42-year-old man is evaluated in the hospital for dyspnea and pleu ritic chest pain. The patient was involved in a motor vehicle accident 3 weeks ago in which he sustained multiple lacerations and a frac ture of his right femur. Medical history is otherwise unremarkable and he takes no medications.
Physicalexaminationshowsatemperatureof38.1°C (100.6°F),blood pressureofl30/78 mm Hg, pulserateofHO/min, andrespirationrate of 22/min. Oxygen saturation is 87% breathing ambient air and 92% on 2 L/min of oxygen by nasal cannula. The lungs are clear and the cardiac examination is significant only for tachycardia. There is a cast in place on the right lower extremity, and there are scattered healing lacerations present. The remainder of the examination is unre markable.
Chest radiograph shows no abnormalities. A complete metabolic profile, including measures of kidney function, is normal. Contrast enhanced CT scan shows pulmonary emboli in the arteries perfus ing the lingula and the posterior basal segment ofthe left lower lobe.
Which of the following is the most appropriate treatment for this patient?
(A) Inferior vena cava filter
(B) Intravenous unfractionated heparin
(C) Intravenous tissue plasminogen activator
(D) Surgical embolectomy
B
Item 25
A 65-year-old man is evaluated because of a 4-month history of gradually progressive shortness of breath. Initially, symptoms were present only with exertion but now are present at rest. He also has an occasionally productive cough. He has a 30-pack-year history of smoking and quit 10 years ago. His occupation history includes extensive and unprotected exposure to asbestos 20 years ago.
On physical examination, he is afebrile, blood pressure is 136/88 mm Hg, pulse rate is 100/min, respiration rate is 24/min, and oxygen sat uration on ambient air is 89% and drops to 86% with exercise. There is clubbing ofthe fingers. Pulmonary examination shows fine inspi ratory crackles bilaterally in the posterior lung zones.
Chest radiograph shows linear opacities in the lung bases bilaterally and linear calcifications along the diaphragm. There is no lym phadenopathy. High-resolution chest computed tomographic scan shows basilar interstitial fibrosis, fine and course honeycombing, traction bronchiectasis, increased interlobular septa! thickening in the subpleural regions, and diaphragmatic plaques with calcification.
Pulmonary function testing shows a predominantly restrictive dis ease pattern.
Which of the following diagnostic tests should be done next?
(A) Antinuclear antibody, rheumatoid factor, and erythrocyte sedimentation rate
(B) Open lung biopsy
(C) Transbronchial lung biopsy
(D) No further testing
D
Item 1 2
A 24-year-old woman is evaluated because of worsening symptoms of asthma. She uses an as-needed albuterol inhaler two to three times per week and has been waking at night at least once a week with
asthma symptoms that require use ofthe inhaler. She is still able to perform most of her daily activities, including regular exercise, if she uses albuterol for prevention. She is allergic to house dust mites, rag weed, grass, trees, and cats.
On physical examination, vital signs are normal. Pulmonary exam ination is normal with no wheezing. Spirometry shows forced expi ratory volume in 1 second (FEV1) of 85% of predicted and an FEV1/forced vital capacity ratio of 80% of predicted.
Which of the following is the most appropriate treatment?
(A) Add a long-acting -2 -agonist
(B) Add a long-acting -2-agonist and a low-dose inhaled gluco- corticoid
(C) Add a low-dose inhaled glucocorticoid
(D) Advise scheduled use of albuterol
(E) Refer for allergen immunotherapy
C
Item 26 [Advanced]
A 32-year-old man is evaluated because of severe dyspnea and dry cough. He has an 8-week history of increasing shortness of breath without fever or chills. He was treated for presumed pneumonia with
azithromycin when his symptoms began. However, the symptoms have continued to worsen. His medical history is otherwise unre markable. He has never smoked, and he takes no medications.
On physical examination, temperature is normal, blood pressure is 135/85 mm Hg, pulse rate is 105/min, and respiration rate is 28/min. Oxygen saturation is 88% on ambient air. There is no jugular venous distention. Pulmonary examination shows bilateral crackles in the midlung zones. Findings on cardiac examination are normal. There is no peripheral edema and no rash or joint swelling.
Chest radiograph is shown.
Which of the following is the most likely diagnosis?
(A) Chronic pulmonary embolism
(B) Community-acquired pneumonia
(C) Cryptogenic organizing pneumonia
(D) Idiopathic pulmonary fibrosis
C
Name the steps in the severity of asthma, FEV1 and treatment
1. Intermittent- >/= 80%- rescue inhaler
2. Mild Persistent- >/= 80%- Low dose ICS
3. Moderate Persistent- 60-80%- low dose ICS & LABA
4. Sever Persistent- <60%- High Dose ICS & LABA
5. Refractory- Sever persistent- PO steroids
Item 1 4
A 28-year-old woman is evaluated because of symptoms of asthma that have worsened since she became pregnant 2 months ago. She has frequent daytime symptoms and increased nighttime awakening because of the symptoms. She has used her albuterol inhaler sever al times per week to achieve symptomatic relief. History includes mild persistent asthma that was well controlled before her pregnancy with an as-needed short-acting -2-agonist and medium-dose inhaled glucocorticoids.
On physical examination, vital signs are normal. The lungs are clear. Cardiac examination shows normal S1 and S2 with no gallops or mur murs. No leg edema is noted.
Spirometry shows forced expiratory volume in 1 second (FEV1) of 85% of predicted and an FEV1/forced vital capacity ratio of 78%. Laboratory studies show a hemoglobin level ofll.5 g/dL (115 g/L).
Which of the following is the most appropriate next step in man agement?
(A) Add a long-acting -2-agonist
(B) Add theophylline
(C) Double the dose of inhaled glucocorticoid
(D) Obtain a bronchial challenge test
A
Item 1 8
A 48-year-old man is evaluated because ofa 1-year history ofcough. He has no shortness of breath, heartburn, or change in appetite or weight. He has a 35-pack-year history of smoking. He has no sea sonal allergies. The medical history is significant for hypertension. His only medication is losartan.
On physical examination, vital signs are normal. Pulmonary exam ination shows normal breath sounds that are equal bilaterally with-out wheezing. No nasal polyps are noted. Findings on abdominal examination are unremarkable. There is no cyanosis, clubbing, or edema. Pulmonary function tests show forced expiratory volume in 1 second (FEV1) of 75% of predicted and an FEV1 /forced vital capaci ty (FVC) ratio of63%. Afteradministration ofabronchodilator, there is no significant change in the FEV/FVC ratio and FEV1 is 83% of pre dicted. Chest radiograph shows no masses, and normal lung mark ings are seen.
Which of the following is the most likely cause of this patient's cough?
(A) Asthma
(B) Chronic obstructive pulmonary disease
(C) Gastroesophageal reflux disease
(D) Losartan use
B
Item 31
A 33 -year-old woman is evaluated for a 2-year history of progressive dyspnea on exertion accompanied by weakness and fatigue. There is no seasonal variation to her symptoms. She reports no history of noc turnal awakening, snoring, or daytime somnolence. She does not have dizziness or syncope. Her medical history is otherwise normal, and she takes no medications.
On physical examination, the patient is afebrile. Blood pressure 115/75mmHg,pulserateis108/minandregular,andrespirationrate is 18/min. BMI is 21. The neck veins are distended. The lungs are clear. Cardiac examination shows regular tachycardia and a prominent pulmonic component of S2• There is edema of the legs bilaterally to the level of the knees.
Laboratory studies, including a complete blood count, serum chemistries, and thyroid and coagulation studies, are normal. Antinuclear antibody, rheumatoid factor, and ANCA studies are neg ative. Chest radiograph reveals prominent central pulmonary arter ies, clear lungs, and normal heart size. Pulmonary function tests reveal a mildly decreased DLCO without evidence of airway obstruc tion or decreased lung volumes. Electrocardiogram shows right axis deviation. Transthoracic echocardiogram shows normal left ventric ular size and function, a dilated right ventricle, and an estimated right ventricular systolic pressure of 40 mm Hg. Ventilation-perfu sion scan is normal.
Which of the following is the most appropriate diagnostic test to perform next?
(A) High-resolution CT scan
(B) Pulmonary angiography
(C) Right heart catheterization
(D) Sleep study
(E) Transesophageal echocardiography
C
Item 27
A 75-year-old man is evaluated because of a 12-month history of cough and dyspnea. He reports no other symptoms or medical prob lems and takes no medications. He has a 40-pack-year history of smoking and does not currently smoke. He is a retired carpenter. He has no pets and no known environmental exposures other than wood dust.
On physical examination, blood pressure is 135/75 mm Hg, pulse rate is 88/min, and respiration rate is 24/min. Oxygen saturation is 88% on ambient air. There is no jugular venous distention. Findings on cardiac examination are normal. Pulmonary examination shows inspiratory crackles at the lung bases bilaterally. Digital clubbing is present.
Pulmonary function testing shows decreased forced expiratory vol umein1second(FEV1), decreasedforcedvitalcapacity(FVC),anor mal FEV/FVC ratio, and decreased Diffusing capacity of carbon monoxide.
Chest computed tomographic scan is shown in your paper
Which of the following is the most likely diagnosis?
(A) Chronic obstructive pulmonary disease
(B) Heart failure
(C) Hypersensitivity pneumonitis
(D) Idiopathic pulmonary fibrosis
D
Item 1 3
A 24-year-old woman is evaluated because of chronic cough that began after a respiratory tract infection 7 months ago. She notices that exposure to cold air and exercise, such as running, are likely to induce cough and wheezing. On rare occasions she is awakened at night with cough. She does not smoke, has no travel history, works as an accountant, and is not exposed to animals. She has no person al or family history ofallergy or asthma. She otherwise feelswell and takes no medications.
On physical examination, vital signs are normal. Upper airway exam ination is normal, and lungs are clear to auscultation. The remainder of the examination is normal.
Chest radiography is normal. On office spirometry, forced expirato ry volume in 1 second (FEV1) is 85% of predicted and FVC is 85% of predicted. The FEY/forced vital capacity (FVC) ratio is 76%. The flow volume loop is normal. Pulmonary function testing shows total lung capacity of 105% of predicted. After the patient inhaled metha choline, there was a 20% drop in FEV1 and FVC.
Which ofthe following is the most likely diagnosis?
(A) Asthma
(B) Cystic fibrosis
(C) Idiopathic pulmonary fibrosis
(D) Vocal cord dysfunction
A
Using RIP for quality of Cxray & ABCDE for reading systematically, Read this Cxray- and diagnose
Item 22
A 61-year-old woman is evaluated because of excessive daytime sleepiness of 7 months' duration. She falls asleep while watching television or reading and recently fell asleep during church and dur ing a conversation. She has no respiratory symptoms. Her only other medical problem is hypertension. Her only medication is amlodip ine. Her husband states that she snores loudly during the night. She does not drink alcohol, smoke cigarettes, or use sedating drugs.
On physical examination, vital signs are normal. Body mass index is 37. Oxygen saturation is 96% on ambient air. The patient has a low hanging soft palate and tongue and tonsils. Other than obesity, the remainder of the findings on physical examination are normal.
Results of complete blood count, electrocardiography, and chest radiograph are normal. The thyroid-stimulating hormone level and resting arterial blood gas results are normal.
Which of the following is most likely to establish the diagnosis?
(A) Chest computed tomography
(B) Overnight pulse oximetry
(C) Polysomnography
(D) Pulmonary function testing
C
Item 1 9
A 72-year-old woman is evaluated for follow-up because of exacer bation of COPD. She has severe COPD without resting hypoxemia. The patient presented 1 week ago with fever, productive cough, and mild dyspnea over her baseline. Use of an albuterol inhaler was increased to six times daily, and a P-lactam/P-lactamase inhibitor and glucocorticoid taper were started. On follow-up today, she is fatigued and dyspneic relative to baseline. The medical history is oth erwise unremarkable. Medications are tiotropium, fluticasone-sal meterol, and albuterol.
On physical examination, temperature is 37.8°C (100.0°F), blood pressure is 130/85 mm Hg, pulse rate is 95/min and regular, and res piration rate is 28/min. She is dyspneic at rest. Pulmonary examina tion shows bilateral expiratory wheezing. Oxygen saturation is 86% on ambient air and 92% on 2 L oxygen via nasal cannula.
Chest radiograph shows no infiltrate and no cardiomegaly.
Which of the following is the most appropriate next step in man agement?
(A) Add home oxygen treatment
(B) Admit to the hospital
(C) Expand the antibiotic spectrum
(D) Prolong the glucocorticoid taper
B
3. A 63-year-old man is evaluated for progressive dyspnea on exertion for the last several months. He can walk two to three blocks on a flat surface but becomes short of breath when going upstairs or uphill. He has a 10-pack-year history of smoking but quit 20 years ago. He takes no medications.
On physical examination, vital signs are normal except for a respi ration rate of 22/min. No jugular venous distention is noted. Pulmonary examination shows reduced breath sounds at the lung bases. Findings on cardiac examination are normal. There is no leg edema.
Pulmonary function tests show forced expiratory volume in 1 sec ond (FEV1) of 75% of predicted, forced vital capacity (FVC) of 68% of predicted with no change after administration of a bronchodilator, total lung capacity of 68% ofpredicted, and residual volume of125% ofpredicted.TheFEV1/FVCratiois82%. Chestradiographshowslow lung volumes with suggested bibasilar atelectasis.
Which ofthe following is the most likely diagnosis?
(A) Chronic obstructive pulmonary disease
(B) Heart failure
(C) Interstitial lung disease
(D) Respiratory muscle weakness
D
Item 23
A 58-year-old man is evaluated because ofa 3-month history ofloud snoring and "gasping" during sleep. He also frequently falls asleep in a chair while reading in the evening. His medical history is other wise unremarkable.
On physical examination, temperature is 37.4°C (99.3°F), blood pres sure is 130/82 mm Hg, pulse rate is 80/min, and respiration rate is 14/min. Body mass index is 34. Neck circumference is 45.7 cm (18.0 in) , and a low-lying soft palate i s noted. Polysomnography shows severe obstructive sleep apnea, with an apnea-hypopnea index of42/h.
Which ofthe following is the most appropriate next step in treat ment?
(A) Continuous positive airway pressure
(B) Nocturnal oxygen therapy
(C) Oral appliance
(D) Upper airway surgery
A
Item 20 [Advanced]
A 56-year-old man is evaluated in the emergency department because of a 3-day history of increasing dyspnea, fever, and cough with purulent sputum. He has severe chronic obstructive pulmonary disease with a history of exacerbations requiring hospitalization. Medicati�ns are ipratropium, salmeterol-fluticasone, and albuterol.
On physical examination, temperature is 38.0°C (100.4°F), blood pressure is 134/84 mm Hg, pulse rate is 88/min, and respiration rate is 30/min. He is awake and alert but is dyspneic and uses the acces sory muscles to breathe. Pulmonary examination shows bilateral expiratory wheezes but no crackles.
An arterial blood gas study performed while breathing 2 L of oxygen via nasal cannula shows pH of7.31, Pco2 of53 mm Hg (7.0 kPa), and Po2 of 55 mm Hg (7.3 kPa) . Oxygen saturation is 89%. Chest radio graph shows hyperinflation but no infiltrates.
In addition to antibiotics, glucocorticoids, and bronchodilators,
which of the following is the most appropriate management?
(A) Continuous positive airway pressure
(B) Increase in nasal oxygen
(C) Intubation and mechanical ventilation (D) Noninvasive positive pressure ventilation
D