Name a BCR-ABL Kinase inhibitor
1st generation and second generation tyrosine kinase inhibitors (BCR-ABL kinase inhibitors)
Used for Ph+ ALL and for CML
What is the mechanism of action for Bortezomib?
Proteosome inhibitor
You have a patient with Anaplastic Large Cell Lymphoma name a possible targeted therapy to treat their disease?
Crizotinib if ALK+
What is the MOA of Bendamustine?
Alkylator and anti-metabolite
Can be used in combination with Brentuximab for HL
Your patient has a diagnosis of AML with a high allelic ratio of FLT3-ITD, what should you consider adding to your therapy?
Sorafenib VEGFR, PDGFR, FLT-3, c-KIT, RAF, RET
Sunitinib C-KIT, FLT-3, VEGFR, PDGFR-B, CSF-1R, RET
AAML1031
Sorafenib can be safely combined the standard pediatric AML chemotherapy. The available efficacy data (CR rate, EFS, RR, OS) are encouraging. The available PIA indicate that adequate inhibition of sorafenib is achieved in a majority of patients with data on Arm C. Additional PIA and PK data analyses will be required to complete the proposed study aims. Ongoing analyses are evaluating the comparative efficacy of the addition of sorafenib to standard chemotherapy for pediatric patient with HAR FLT3 ITD
What is the target of Gemtuzumab?
CD33, used for AML
What is the mechanism of action of Brentuximab?
Anti-CD30 antibody conjugated via a protease-cleavable linker to the potent anti-microtubule agent monomethyl auristatin E (MMAE). Following binding to CD30, brentuximab vedotin is rapidly internalized and transported to lysosomes where MMAE is released and binds to tubulin, leading to cell cycle arrest and apoptosis.
Alemtuzumab is a monoclonal antibody against....
CD52
Your patient has bone marrow blasts that are positive for Express cytoplasmic CD3 (cCD3+); most sCD3+ and TdT+, What agent should you consider adding to the standard BFM therapy?
Nelarabine
Does Dasatanib Cross the blood brain barrier?
Yes!
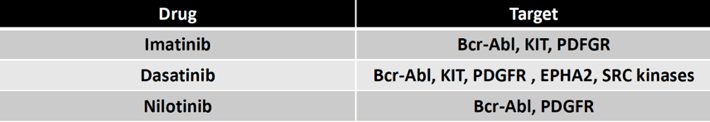
AALL1122 discusses the important differences between Imatinib and Dasatanib. Dasatanib has dual targeting of ABL and SRC family kinases, more potent suppression of the BCR-ABL signaling, broad spectrumactivity against most imatinib-resistant BCR-ABL mutants.
Another potential advantage of dasatinib is that, unlike imatinib, it is capable of crossing the blood brain barrier and long-lasting results in patients with CNS disease have been reported.
While long-term toxicity data are not yet available from either of these COG Ph+ ALL trials incorporating imatinib or dasatinib, the use of large amounts of alkylators and multiple cycles of high dose methotrexate in the backbone may result in increased rates of infertility and CNS toxicity.
AALL1122 closed in 2015, no results available yet.
What diseases has Brentuximab demonstrated efficacy?
Hodgkins Lymphoma
ALCL
What are the results of AALL1131?
Blinatumomab (Blincyto) as post-reinduction consolidation therapy before hematopoietic stem cell transplantation (HSCT) improved disease-free survival (DFS) and overall survival (OS) by approximately 20% compared with intensive chemotherapy in pediatric and adolescent and young adult (AYA) patients with high- or intermediate-risk of first relapse of B-cell acute lymphoblastic leukemia (B-ALL), according to results presented at the 2019 ASH Annual Meeting.1
Your adolescent patient was recently diagnosed with Pre-B ALL, further testing confirms CRLF2 mutation, what agent should you consider
Ruxolitinib on study AALL1521
What is the efficacy of Bortezomib in leukemia?
AALL07P1: Relapsed ALL
Bortezomib appears to show efficacy in pre-B patients < 18 months from diagnosis and in T-cell ALL patients (60% response rate). Bortezomib also appears to show efficacy in T-ALL with a 68% response rate. This is in contrast to AALL01P2, in which only 1 of 7 (17%) T-ALL patients attained CR2 at the end of the first block of re-induction therapy
AALL1231:Newly diagnosed T-ALL
Patients will be randomized to receive backbone therapy with or without bortezomib during Induction and Delayed Intensification. Results not yet available
AAML1031
NOT HELPFUL
You have a patient with Group B DLBCL, in addition to standard chemotherapy, what targeted agent should be incorporated into therapy?
Rituximab
Per ANHL1131
The analysis showed 1-year EFS rate of 81.5% (95%CI=73.0%-87.8%) in the control arm and of 94.2% (95%CI=88.5%-97.2%) in the Rituximab arm.
How do you handle immunizations after CAR-T therapy?
In general only the influenza shot is given during B-Cell aplasia as patients are not expected to mount a response to vaccines
Your patient has received CAR-T cell therapy and has developed Grade 2 CRS. You decided to intervene with Tocilizumab, what is the MOA?
humanized, anti-human interleukin 6 (IL-6) receptor monoclonal antibody
What is the prevelance and outcome of Ph+ ALL in pediatric patients?
This translocation (9,22) is found in 3% to 5% of pediatric ALL and in 20% to 40% of adult patients with ALL.
The presence of the Philadelphia chromosome is considered a poor prognostic factor in both pediatric In a recent large series of 610 children and adolescents with Ph+ ALL treated with conventionalmultiagent chemotherapy, the overall complete remission rate was 89%; however, the 7-yearevent-free survival (EFS) and 7-year overall survival (OS) rates were only 32% and 45%
Children’s Oncology Group (COG) AALL00311 established the safety and efficacy of an intensive chemotherapy backbone plus imatinib in treating children with Ph+ ALL lead to EFS of 71% 3 year EFS and transplant did not impact outcome. However MRD was a significant predictor of relapse. Future trial 1122 uses Dasatinib and only transplants for MRD
1) MRD at end of IB/start of consolidation block 1 (HR1) ≥ 0.05% (5 x 10-4) OR
2) MRD at end of IB/start of consolidation block 1 (HR1) 0.005-0.05% (5 x 10-5 to 5 x
10-4)* as measured by Ig/TCR PCR and MRD at end of consolidation block 3
(HR3)/start of reinduction block 1 remains positive at any detectable level (providing the assay limit is at least 0.1%)
Name a PD-1 inhibitor (check-point inhibitors) that is used in in Hodgkins Lymphoma?
Pembrolizumab, Nivolumab

The Role of Immune Checkpoint Inhibitors in Classical Hodgkin Lymphoma
Nicholas Meti, Khashayar Esfahani, and Nathalie A. Johnson
Additional article information
Abstract
Hodgkin Lymphoma (HL) is a unique disease entity both in its pathology and the young patient population that it primarily affects. Although cure rates are high, survivorship can be linked with significant long-term morbidity associated with both chemotherapy and radiotherapy. The most significant recent advances have been with the use of the anti-CD30-drug conjugated antibody brentuximab vedotin (BV) and inhibitors of program death 1 (PD-1). HL is genetically wired to up-regulate program death ligand 1 (PD-L1) in >95% of cases, creating a state of so-called “T cell exhaustion”, which can be reversed with immune checkpoint-inhibitor blockade. The overall and complete response rates to PD-1 inhibitors in patients with relapsed or refractory HL are 70% and 20%, respectively, with a long median duration of response of ~16 months. In fact, PD-1 inhibitors can benefit a wide spectrum of relapsed HL patients, including some who have “progressive disease” by strict response criteria. We review the biology of HL, with a focus on the immune micro-environment and mechanisms of immune evasion. We also provide the rationale supporting the use of PD-1 inhibitors in HL and highlight some of the challenges of monitoring disease response in patients treated with this immunotherapy.
Keywords: Hodgkin Lymphoma, immune checkpoint inhibitors, immunotherapy
1. Overview of Hodgkin Lymphoma
Hodgkin Lymphoma (HL) has an annual incidence of 2–3 cases per 100,000 in Europe and the USA, and epidemiological data has revealed that one in eight patients will die from the disease [1,2,3]. It has a bimodal peak, with young adults aged between 15–34 being the most affected, followed by those aged 60 and older [4]. Although the cause of HL is unknown, several risk factors have been studied. These include genetic predisposition [5], immunosuppression in the context of human immunodeficiency virus infection [6], and other viral infections such as Epstein Barr Virus [7]. Based on cellular morphology and immunohistochemistry, HL can be classified into either classical HL (cHL) or nodular lymphocyte-predominant HL (NLPHL) [8,9,10]. cHL represents approximately 90% of all HL and can be further classified into four histological subtypes known as nodular sclerosis HL, mixed cellularity HL, lymphocyte-rich HL, and lymphocyte depleted HL. Given the predominance of cHL, this review will focus on cHL and advancements in the treatment of cHL.
2. Biology and Diagnosis of Classical Hodgkin Lymphoma
The histological presence of mononuclear Hodgkin (H) and bi- to multi-nuclear, diagnostic Reed–Sternberg (RS) cells is pathognomonic of cHL. Given that both cell types are malignant, they are also referred to as HRS cells. They are derived from clonal germinal center B (GCB) cells, having rearranged and mutated immunoglobulin variable genes [11], However, with the exception of PAX5, typical GCB surface markers (CD19, CD79) and transcription factors (OCT-2, BOB.1 and PU.1) are down-regulated or completely absent in HRS cells and CD20 is expressed in only 20% of cases [10,12,13]. In contrast, HRS cells universally express CD30 and 75–85% of cases express CD15 [14,15,16,17,18,19,20,21]. The reprogramming and loss of the B cell phenotype in HRS cells likely occurs due to genomic alterations that alter important signaling pathways, including NOTCH-1, Janus kinase and Signal Transducer and Activator of Transcription (JAK/STAT), and nuclear factor kappa B (NF-κB) [22,23,24]. Genomic amplification of REL, MAP3K14, and BCL3 and mutations in NFKBIE, NFKBIA, and TNFAIP3 contribute to constitutive activation of the NF-κB pathway, promoting the survival of HRS cells [23,25,26,27,28,29]. Constitutive JAK/STAT signaling is also a hallmark of cHL and most commonly occurs as a consequence of amplification of JAK2 and mutations in STAT6 [30,31,32]. More recently, whole exome sequencing of HRS cells has revealed that ~90% of cHLs harbor mutations affecting the JAK/STAT pathway (including STAT6, SOCS1, STAT3, STAT5B, JAK1, JAK2, and PTPN1) [33]. Other genomic alterations also contribute to HRS survival by implicating the nuclear export of proteins and RNAs (XPO1), AKT signaling (GNA13 and ITPKB), and evasion of immune surveillance (CIITA, PDL1, B2M, CD58, and TNFRSF14) [33]. Finally, HRS cells have genomic instability resulting from ongoing chromosomal rearrangements [34] and disruption of 3D telomere-TRF2 interaction [35].
The HRS cell represents only ~1% of all cells within the tumor environment, the remaining being composed of various immune cells, such as macrophages, eosinophils, neutrophils, mast cells, fibroblasts, and B and T lymphocytes. The predominant fraction of these immune cells belong to the CD4+ T cell family, specifically T helper 2 (Th2) and T regulatory (Treg) cells [36,37,38]. These immune cells are recruited to this inflammatory milieu by the presence of cytokines and chemokines within the microenvironment. In fact, HRS cells can express and secrete CCL5, CCL17, CCL22, and IL-5, all of which can attract CD4+ T cells into the microenvironment [39]. Once the CD4+ T cells rosette the HRS cells, various ligand-receptor interactions occur, including CD40-CD40L, which has been shown to trigger the NF-κB pathway and lead to further production and maintenance of HRS cell colonies [40,41,42,43].
In order to thrive in a lymphocyte-rich microenvironment, HRS cells have developed multiple mechanisms to promote immune tolerance. The most clinically significant mechanism of dampening effector T cell function is by stimulating the programmed death 1 (PD-1)/programmed death ligand 1 (PD-L1) immune checkpoint. PD-L1 expression is variable in cHL patients [44,45], but recent evidence has demonstrated that the level of expression of PD-L1 is associated with the number of copies of the PDL1 gene locus present on chromosome arm 9p24. High-level amplification, present in a third of HL cases, is associated with the highest expression of PD-L1 protein at the cell surface [46]. The 9p24.1 amplification also contains Janus kinase 2 (JAK2) and PDL2, which further upregulates PD-L1 expression, the former through activation of JAK/STAT signaling [46]. Finally, Epstein–Barr virus (EBV), present in HRS in 30–40% of classical HL, can also promote the expression of PD-L1 and PD-L2 [47]. More specifically, EBV induces PD-L1 expression through the activation of the transcription factor pathway AP1 and downstream upregulation of c-Jun and JunB, a hallmark pathway of classical HL, irrespective of 9p24.1 copy numbers [48,49]. In addition to hijacking the immune checkpoint system, HRS cells have also evolved other mechanisms to evade immune surveillance. Recent evidence is emerging that highlights a lack of β2-microglobulin (B2M) and Major Histocompatibility Complex (MHC) class I at the HRS cell surface in ~90% of cHL cases, which is an essential requirement for an effective CD8+ T cell cytotoxic response [50,51,52]. Furthermore, MHC class II is not expressed on the surface of HRS in ~40% of cHL cases, which is critical for antigen presentation to CD4+ helper T cells [53]. Taken together, HRS cells have adapted multiple mechanisms to evade immune surveillance and thrive in an immune rich milieu (Figure 1).

Figure 1
Hodgkin Reed-Sternberg (HRS) cells escape immune detection by over-expressing program death ligands PDL1/PDL2 and silencing Major Histocompatibility Complex (MHC) expression. HRS cells over-express PDL1 and PDL2, both ligands for PD1 on T cells, which...
3. Management of Classical Hodgkin Lymphoma
The initial management of cHL is based on the patient’s stage and presence of adverse factors at the time of diagnosis. Positron emission tomography and contrast-enhanced computed tomography (PET/CT) is recommended for initial staging and for subsequent assessment of response to treatment [54]. Chemotherapy remains the standard initial treatment of limited and advanced stage cHL, but the preferred regimen, the number of cycles administered, and the addition of radiation therapy is a matter of debate, which has already been featured in recent reviews [55,56,57]. The two main chemotherapy regimens include either (1) adriamycin (A), bleomycin (B), vinblastine (V), and dacarbazine (D) (ABVD) or (2) bleomycin, etoposide, adriamycin, cyclophosphamide, vincristine, procarbazine, and prednisone (BEACOPP). The two main treatment options for patients with limited stage cHL are either a standard abbreviated course of chemotherapy, typically ABVD, followed by involved field radiation therapy (IFRT) [58,59] or 4–6 cycles of chemotherapy in patients who are deemed not candidates for radiotherapy [60], or a risk-adapted strategy based on the results of an interim PET (iPET) scan performed after 2–3 cycles of ABVD [61,62]. Approximately 80% of patients will be classified as low-risk (iPET-negative), and chemotherapy alone (total 3–4 cycles) without radiation could be considered at a cost of ~5% increased risk of relapse [61]. Combined modality therapy, with possible escalation to BEACOPP, can be considered for the remaining high-risk patients with iPET-positive scans [62]. Patients with advanced stage disease are managed with chemotherapy, either ABVD or BEACOPP, or can follow a risk-adapted approach in which patients are given 2 cycles of ABVD, and, if the iPET is negative, bleomycin can be omitted from the subsequent cycles and if the iPET scan is possible, one can consider escalation to BEACOPP [63,64]. The United States Federal Drug Administration (USFDA) recently approved the addition of brentuximab vedotin (BV) to AVD as an alternative front-line option for patients with advanced HL. BV is an anti-CD30 antibody conjugated monomethyl auristatin E (MMAE) that has significant activity in the relapse setting. In the ECHELON-1 trial, which included 1334 patients with untreated stage III or IV cHL, BV + AVD (AAVD) had a 5% 2 year modified progression-free survival (PFS) advantage over ABVD, but was associated with increased rates of neutropenia and neuropathy [65]. In this trial, 67/1334 (5%) of patients died, with over 90% of events due to treatment-related toxicity, febrile neutropenia in patients treated in the AAVD arm and bleomycin-lung toxicity in the ABVD arm.
The management of patients with relapsed and refractory classical Hodgkin lymphoma (rrHL) that has progressed after frontline therapy is to proceed with salvage chemotherapy followed by autologous stem cell transplant (ASCT) in eligible patients [66]. Multiple salvage chemotherapy regimens have been tested in this setting, but none have been shown to improve overall survival over another [67]. Consolidation with an ASCT in patients with chemo-sensitive disease is considered curative in ~50% of cases [66,68,69,70]. One drug that has been extremely effective in rrHL is BV due to the hallmark feature of increased CD30 expression. The unconjugated anti-CD30 antibody, without MMAE, had minimal clinical activity in patients with rrHL, having an overall response rate (ORR) of 0% [71]. Based on these data, one can conclude that the main clinical benefit of BV is not a consequence of immune-mediated cytotoxicity, but rather the delivery of a potent anti-microtubule inhibitor to HRS cells [71,72]. In patients with rrHL that has relapsed after ASCT, BV has an ORR of 75% and a complete response (CR) rate of 34%. The 5-year PFS and overall survival (OS) was 22% and 41%, respectively [72,73]. Given the impressive response rates of BV in this setting, it has been studied in combination with chemotherapy as part of salvage therapies. For example, BV combined with bendamustine demonstrated impressive results in 2 recent phase I–II trials, with an ORR of 78–93% and CR rate of 43–77% [74,75]. In the study by LaCasce et al., 56% of patients treated with BV and bendamustine experienced infusion-related reactions (IRR) events, which were found to be associated with the production of anti-BV antibodies after cycle 1 in 75% of their patients [75]. BV maintenance can also extend the duration of remission in high-risk patients post ASCT. In the AETHERA phase III trial, maintenance BV extended PFS by 19 months compared to observation alone [76]. There was no overall survival benefit with this strategy and the main toxicities were neutropenia and sensory peripheral neuropathy, which were reversible in most patients.
Taken together, the general approach in treating cHL patients has been to select a treatment that will maximize cure (OS) and minimize long-term toxicity. Unfortunately, these end-points are not often reported in clinical trials due to the extended follow-up time required to capture them. Adding a therapy that has no or very little long-term toxicity to the initial chemotherapy backbone has the potential to improve the outcome of patients with cHL by limiting exposure to subsequent therapy and ASCT that can increase long-term morbidity.
4. Immune Checkpoint Inhibitors in Classical Hodgkin Lymphoma
In the past decade, there has been a tremendous success in the field of cancer immunotherapy with the introduction of immune checkpoint inhibitors (ICI). Following exposure to antigen and T cell activation, immune checkpoints (ICs) become expressed at the surface of T cells to inhibit T cell function [77]. This innate mechanism of avoiding damage to self upon chronic antigen exposure is often hijacked by tumors to escape immune detection. The most clinically-relevant IC in cHL is PD-1. PD-L1 expression is not only seen on HRS cells but also on tumor-associated macrophages (TAMs), which may further contribute to so-called T cell exhaustion [44,78]. Engaging PD-1/PD-L1 impairs antitumor T cell function by inhibiting downstream signaling from co-stimulatory receptors and by inducing direct transcription of genes known to suppress T cell function
What is the dreaded complication of Inotuzumab?
SOS