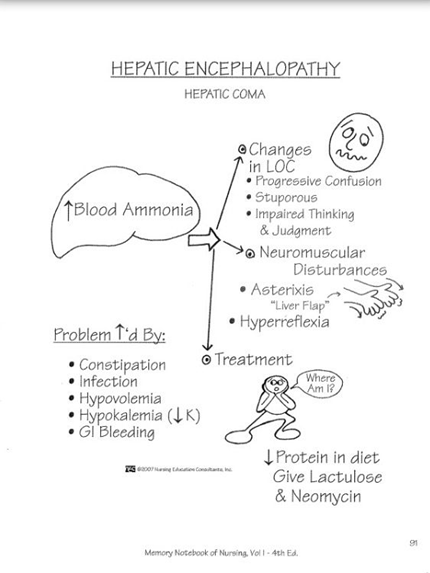
Clinical Manifestations of Hepatic Encephalopathy:
•Initial manifestations are subtle and may include:
•Irritability
•reversed sleep-wake cycles
•brevity of responses
•Apathy
postprandial confusion
Hypernatremia cause
•Cause:
increased insensible water losses, decreased thirst or access to water, infusion of large volumes of saline or bicarbonate, or diabetes insipidus
Post-Transplant Encephalopathy
• Encephalopathy following transplantation may be due to underlying conditions, operative procedures, immunosuppressive medications, cranial radiation, or opportunistic infections.
•Underlying disease that led to transplant
•Medications
•Rejection
•Infection
Unprovoked Seizures
•Unprovoked seizure refers to a seizure of unknown etiology as well as one that occurs in relation to a preexisting brain lesion or progressive nervous system disorder.
•Unprovoked seizures that are determined to be due to an underlying brain lesion or disorder are also referred to as remote symptomatic seizures.
•They carry a higher risk of future epilepsy compared with acute symptomatic seizures.
Acute hepatic encephalopathy
•In acute hepatic encephalopathy, an explosive, progressive course develops after the acute insult to the liver
PT shows with the following. what should be the tx? and dx?
•drowsiness, confusion, and occasionally seizures
Hypernatremia
Slow correction of sodiumpernatremia
•most common cause of acute TME
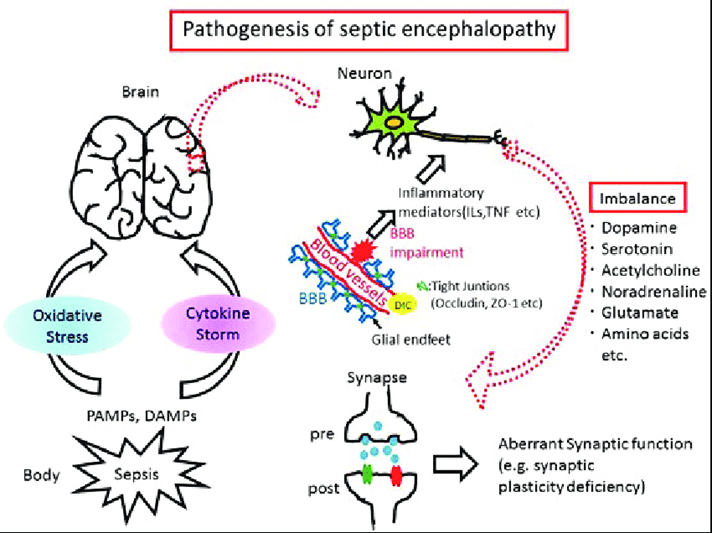
Septic Encephalopathy
What's epilepsy definition
•At least two unprovoked (or reflex) seizures occurring more than 24 hours apart.
•One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk after two unprovoked seizures (eg, ≥60 percent) occurring over the next 10 years. This may be the case with remote structural lesions such as stroke, central nervous system infection, or certain types of traumatic brain injury.
•Diagnosis of an epilepsy syndrome.
Chronic clinical manifestations of hetatic encephatopathy
•In chronic hepatic encephalopathy, the findings tend to fluctuate with periods of remission interspersed
Hypercalcemia
manifests as drowsiness that can progress to coma, and is readily reversible
Septic encephalopathy Pathophysiology:
•Microcirculatory abnormalities, altered blood-brain barrier permeability, inflammatory cytokines, reductions in monoamine neurotransmitters, and an increase in the concentration of the false neurotransmitter octopamine
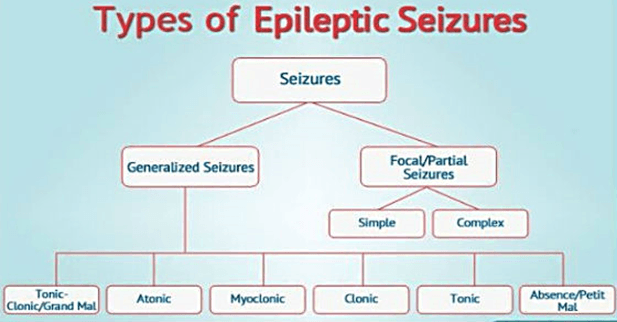
Types of Seizures
•Focal with retained awareness
A simple partial seizure
•Focal with impaired awareness
AKA complex partial seizure
•Generalized
AKA grand mal seizures, major motor seizures, or convulsions
Treatment of Hepatic Encephalopathy
Treatment of hepatic encephalopathy begins with correction of:
•coagulation parameters
•electrolyte abnormalities
•volume depletion
•hypoxemia
and identification and treatment of potential infectious precipitants (make sure to start on antiotics)
made worst when pt is constipated
Severe hypophosphatemia
leads to muscle weakness with particular preference for the diaphragm. Confusion, ataxia, nystagmus, and abducens palsy may occur.
Diagnosis for septic encehalopathy?
•Diagnosis:
•A lumbar puncture performed to exclude meningitis may be entirely normal or show an elevated protein concentration
•The electroencephalography (EEG) is usually diffusely slow
Focal with retained awareness symptoms:
•Symptoms depend entirely on the part of the cortex that is disrupted at the onset of the seizure.
•Aura: occurs at the beginning of a seizureà
•focal seizures that affect enough of the brain to cause symptoms, but not enough to interfere with consciousness
•Postictal
•May return immediately to baseline
•May have period of worsened neurologic function
•Todd paralysis (example- seizure in left arm remains weak after seizure for several hours)
Uremic Encephalopathy:
diagnosis
•Diagnosis:
•The EEG in uremia reflects the severity of encephalopathy. (pt with increased confusion)
•The most common EEG finding is prominence of slow waves.
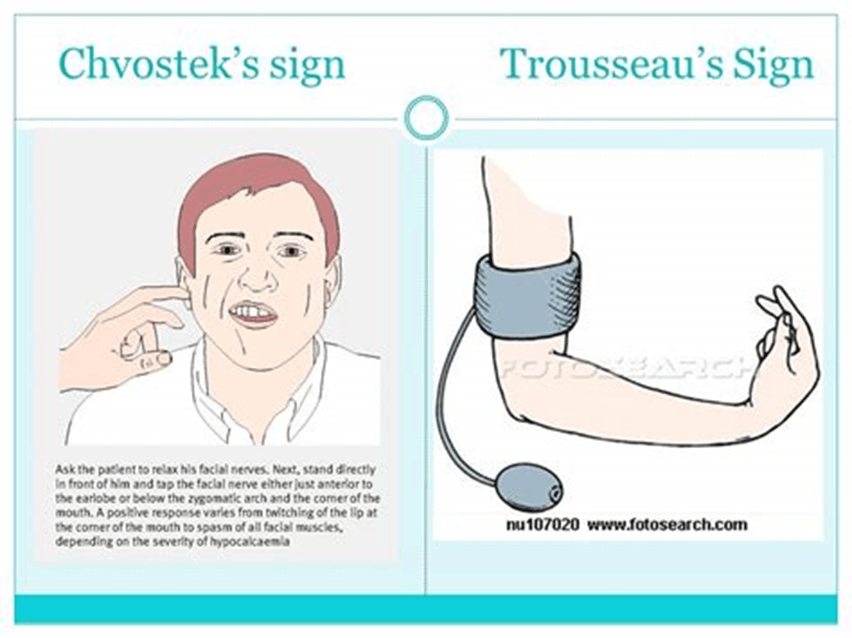
Hypocalcemia
and hypomagnesemia frequently coexist and present with muscle weakness, behavioral changes, hallucinations, seizures, and coma. Chvostek's and Trousseau's signs may be present.
Patient presents to ER with Lp is normal shows an elevated protein conenctration, the EEG is diffusely slow. HOw would you tx and diagnose pt?
Septic Encephalopathy
•Treatment:
•control of the underlying infection
•Aura: occurs at the beginning of a seizureà
•focal seizures that affect enough of the brain to cause symptoms, but not enough to interfere with consciousness
Early clinical features: of urimic encephalatophy
•Lethargy
•Irritability
•Disorientation
•Hallucinations
•Rambling speech
Recognize and describe these? Chvostek's sign and trousseasus's sign
Acute hepatic encephalopathy
•associated with marked cerebral edema is seen in patients with the acute onset of hepatic failure.
focal seuzures begin in
•A seizure that begins in the occipital cortex may result in flashing lights
HOw would you treat a pt with this symptoms and what's the dignosis?
•Lethargy
•Irritability
•Disorientation
•Hallucinations
•Rambling speech
Uremic Encephalopathy
•Treatment:
•reverses with dialysis, although a lag time of one to two days usually is required before mental status clears
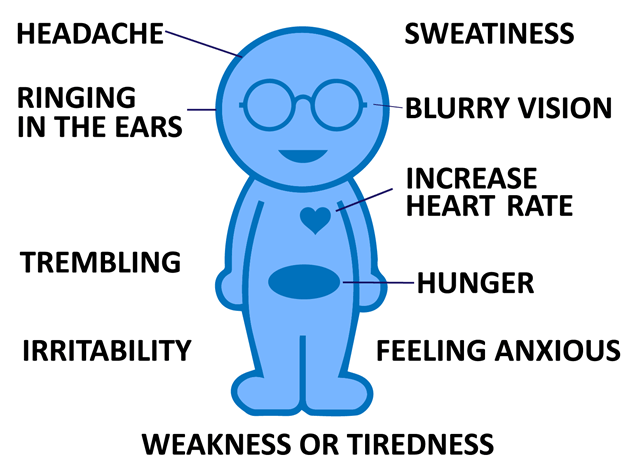
Hypoglycemia presentation?
•symptoms of increased epinephrine release (eg, tremor, diaphoresis)
•neurologic symptoms that correlate poorly with glucose concentrations and include generalized seizures, bizarre behavior, coma, and focal deficits
Chronic hepatic encephalopathy
•occurs in subjects with chronic liver disease and portosystemic shunting of blood.
What part of the brain does seizures affect?
•A seizure that affects the motor cortex will result in rhythmic jerking movements of the face, arm, or leg on the side of the body opposite to the involved cortex (Jacksonian seizure)
•A seizure that begins in the parietal cortex may cause distortion of spatial perception; a seizure that begins in the dominant frontal lobe may cause sudden speech difficulties.
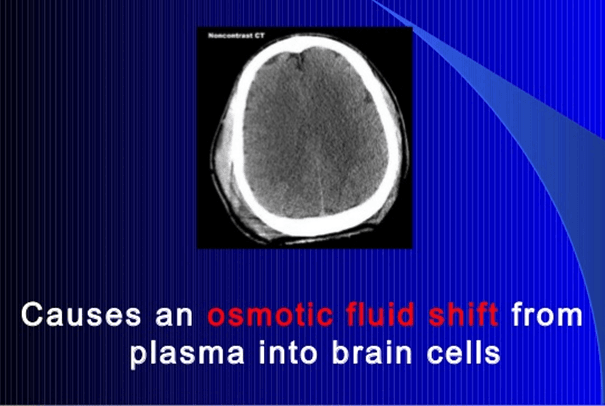
Hypoanatremia cause
•Most often due to the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) or a decrease in effective circulating blood volume
Pt shows witht the following symptoms what's the diagnosis and how should you treat it?
•symptoms of increased epinephrine release (eg, tremor, diaphoresis)
•neurologic symptoms that correlate poorly with glucose concentrations and include generalized seizures, bizarre behavior, coma, and focal deficits
Hypoglycemia
Glucose replacement
Pathophysiology found in hepatic encephalopathy?
Multifactorial -> increased ammonia concentration, false neurotransmitters, endogenous benzodiazepine-like substances, abnormal fatty acid metabolism, free radical damage, cerebral edema, and increased mercaptans (waste product)
•Most common type of seizure in adults with epilepsy!
Focal impaired awareness
Pt presents with Confusion, disorientation, agitation, delirium, lethargy, muscle cramps, and generalized weakness are common
whats the diagnosis? and tx?
Hyponatremia
•Treatment:
•Slow correction of sodium
Hyperosmolar Hyperglycemia and DKA what could happen if they present with this?
•Patients with hyperosmolar hyperglycemic state (HHS) and diabetic ketoacidosis (DKA) will develop progressive neurologic impairment with lethargy and progressive obtundation and, ultimately, coma
•Focal deficits and seizures can occur
•Often precipitated by infection or medical noncompliance
Definition of Seizure disorders?
•A sudden change in behavior caused by electrical hypersynchronization of neuronal networks in the cerebral cortex
Focal with impaired awareness
presentation:
•appear to be awake but are not in contact with others and do not respond normally to instructions or questions
•may stare into space and either remain motionless or engage in repetitive behaviors, called automatisms, such as facial grimacing, gesturing, chewing, lip smacking, or repeating words or phrases
may become hostile or aggressive if physically restrained
What's Acute Toxic-Metabolic Encephalopathy?
•Definition:
•Acute toxic-metabolic encephalopathy (TME) is an acute condition of global cerebral dysfunction in the absence of primary structural brain disease.
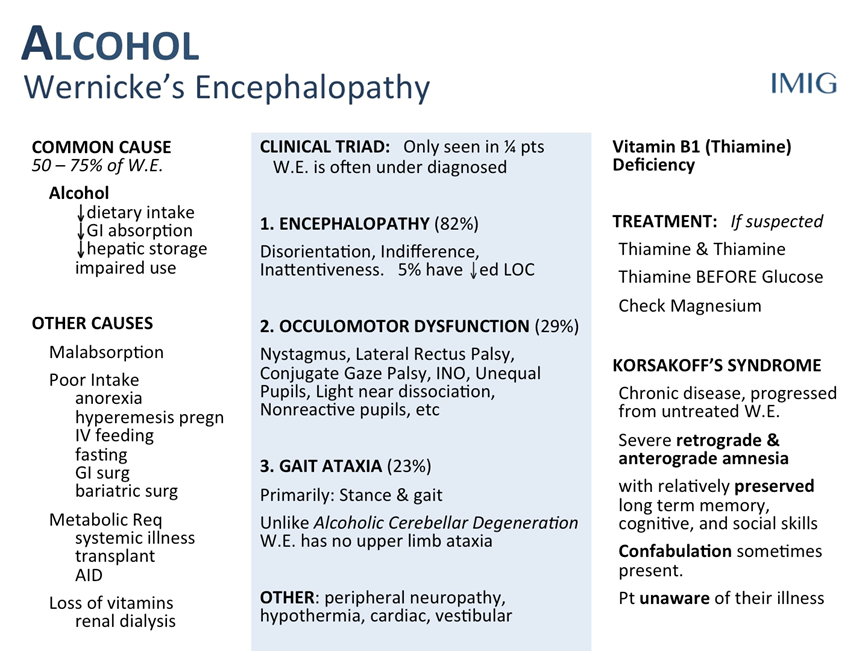
Triad for Thimine deficiency ?
•triad of confusion, ataxia, and ophthalmoplegia.
Seizure Disorders are referred as these tow types?
•Seizures are typically referred to as either acute symptomatic seizures or unprovoked seizures depending on the clinical circumstances at the time of the event.
•How long do focal with imparied awareness seizures last?
•Typically less than 3 minutes
What's the pathophysiology of Acute Toxic-Metabolic Encephalopathy?
•Pathophysiology:
The neurophysiologic mechanisms of TME include interruption of polysynaptic pathways and altered excitatory-inhibitory amino acid balance.
Wernicke’s Encephalopathy
•THIAMINE DEFICIENCY
•Alcoholism
•Wernicke encephalopathy is characterized by a triad of confusion, ataxia, and ophthalmoplegia.
•refers to the tendency for recurrent, unprovoked seizures.
Epilepsy
•characterized by somnolence, confusion, and headache for up to several hours
often have no memory of what took place during the seizure other than, perhaps, the aura
Focal with impaired awareness
What are the clinical manifiestations ffound in acute toxic-metabolic encephalopathy?
•Clinical manifestations:
•TME manifests clinically as a delirium with either an agitated confusion or somnolence.
•Impaired attention is a cardinal feature.
•Other more variably appearing features include tremor, myoclonus, and asterixis.
•In severe cases, posturing may occur and brainstem reflexes may be impaired.
•Ocular signs are the hallmark of the disease, including horizontal nystagmus, bilateral abducens palsy, complete ophthalmoplegia, and pupillary abnormalities
Wernicke’s Encephalopathy
Seizures are categorized as
Seizures are further categorized as either focal or generalized according to whether the onset of electrical activity involves a focal region of the brain or the entire cortex simultaneously.
Differential Diagnosis: acute toxic-metabolic encephalopathy?
•Alcohol withdrawal
•Meningitis
•Encephalitis
•Brain tumors
•Nonconvulsive seizures
•Central venous thrombophlebitis
•Bacterial endocarditis
•Fat embolism
•Basilar artery thrombosis
•Traumatic brain injury
•Right hemisphere stroke
who can be afected by wernicke's encephalopathy ?
•Patients who are fasting, receiving parenteral nutrition, recovering from gastrointestinal surgery, being fed after a period of starvation, undergoing hemodialysis, or suffering from advanced cancer are particularly susceptible to this disorder.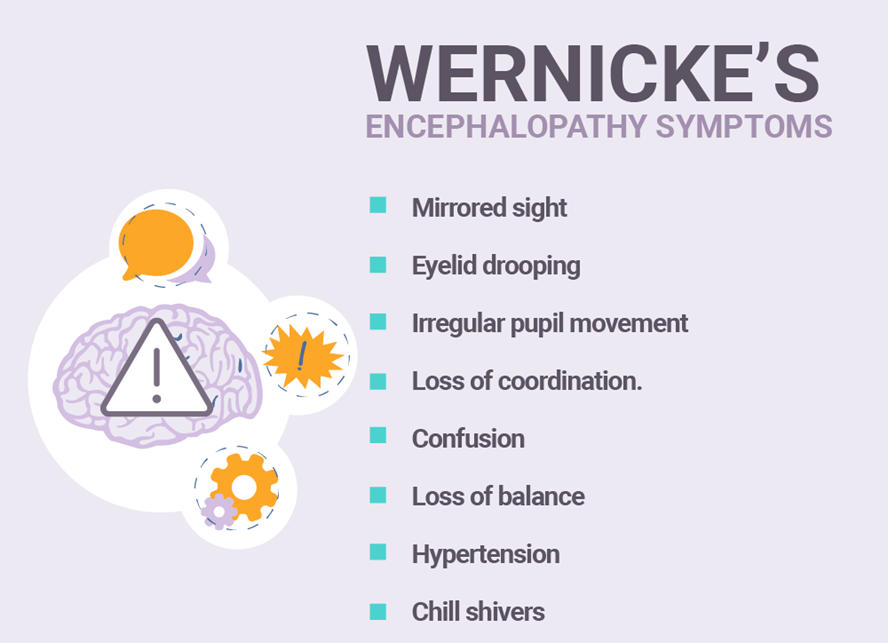
Clinical manifestations of seizures and causes?
•The clinical manifestations of seizures vary based on the location of the seizure in the brain and the amount of cortex that is involved.
•The causes of epilepsy can be broadly categorized as genetic, structural, metabolic, immune, infectious, and unknown.
•While a significant proportion of epilepsy in childhood has a genetic, metabolic, or congenital structural basis, epilepsy diagnosed in adults is more likely to be due to an acquired vascular, degenerative, or neoplastic etiology.
•Seizure is largely a clinical diagnosis made by history, physical and neurologic examinations, and selected additional tests to identify an underlying cause.
Pt presents with impaired attention what's diagnosis
Acute Toxic-Metabolic Encephalopathy
HOw do we treat wernicke's encephalopathy?
Acute Symptomatic Seizure
•What is an acute symptomatic seizure?
•A seizure that occurs at the time of a systemic insult or in close temporal association with a documented brain insult
•Carry low risk for future epilepsy
What's Hypoxic-Ischemic Encephalopathy?
•Straightforward diagnosis that follows an obvious precipitating event such as cardiac arrest with prolonged resuscitation efforts
Clinical findings for Hypoxic-Ischemic Encephalopathy?
•Clinical findings range from subtle memory difficulties to coma
Other common clinical findings include cortical blindness, myoclonus, seizures, cerebellar ataxia, akinetic-rigid syndromes, and bilateral arm weakness due to watershed-territory infarctions
What causes Acute Seizure?
•Within one week of stroke, traumatic brain injury, anoxic encephalopathy, or intracranial surgery
•At first identification of subdural hematoma
•During the active phase of a central nervous system infection
•Within 24 hours of a severe metabolic derangement