Remains on instruments and is made up of microorganisms and cellular tissue
What is biofilm or bioburden
Test systems containing viable microorganisms providing a defined resistance to a specific sterilization process
– Provides information on whether necessary conditions were met to kill a specified number of microorganisms for a given sterilization process, providing a level of confidence in the process
What is a biological indicator
What scopes require prior before they are sent to sterile processing
What is point of use cleaning
Identify three steps done in the OR room prior to transport to prepare instruments for processing (5)
1. Wipe Bioburden off as instruments are returned to scrubber
2. Open tips of instruments on stringers and remove disposable sharp objects
3. Place delicate items in a separate area or on a towel to avoid damage
4. Use enzymatic product for pre treatment
5. Cover and place bio hazard sign on cart
The three categories of Spaulding's Classification
What is : Critical, Semi Critical, Non Critical
High level disinfection kills most microorganisms with the exception of
What are spores
The yellow dot indicates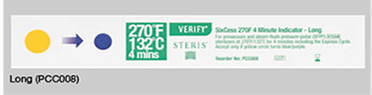
Unsterile, not exposed to sterilization
1. What do scopes require before transport?
2. Recommendation for time that cleaning is performed after pre cleaning
1. remove organic soil and biofilm with precleaning kits
2. No more than one hour after pre cleaning
The instructions we follow when decontaminating or cleaning instruments
What are manufacturer's instructions for use (IFU)
First step of decontamination
What is wiping off bioburden from instruments returned to scrubber
Give an example of devices in OR using Spaulding's Classification
Critical
Semi Critical
Non Critical
Critical: Instruments, Implants, Sutures, Cardiac Catheters
Semi Critical: Endoscope, cystoscopies, bronchoscopes, endocavity ultra sound probes
Non Critical: Blood pressure cuffs. OR furniture and tables, Linen
The four principles of steam sterilization
What are steam, pressure, temperature, and time
Two actions to do if any evidence of contamination (water, wet spots, organic material) in the scope storage cabinet
Reprocess scope
Clean cabinet
The difference between Cleaning and Decontamination
Cleaning does not remove pathogenic microorganisms or make them safe to handle, use or discard
Decontamination removes pathogenic microorganisms and makes them safe to handle
Any instrument or device opened for a procedure, even if the procedure does not occur
What is contaminated
Concept that sterility is dependent upon: amount of handling, conditions during transport and storage, quality of packaging material , adherence to packaging manufacturers IFUs
What is event related sterility
The five steps of sterilization
1.Items are cleaned at point of use
2.Decontaminated
3.Inspected/Sterilized
4.Packaged
5.Stored in a controlled environment
Two reasons we do leak testing on scopes
To find
1. Leaks in the endoscope.Openings in the scope that can let water and organic materials
2. It reduces damage and repair costs and decreases the potential for patient infections or injury
Many facilities use this machine to clean and decontaminate instruments prior to sterilization
What is a washer sterilizer or mechanical washer
The steps to take if an unsterile tray is opened and on the sterile field (Name at least three)
•Immediately remove
•Circulator notifies SPT staff
•Remove sterilizer from use.
•Confirm what the failure was.
•Investigate cause of failure.
•Inform key people: charge nurse, core, managers
•Completes a PASS report
•Root Cause Analysis
•Prevention of future failure events
Where instructions are found for a particular disinfecting solution
The level of disinfection required for reusable devices that enter the mucosa or an endocavity
1. MSDS
2. High Level Disinfection
Identify difference between Pre Vac and Gravity Displacement steam sterilizers
Gravity Displacement: Steam enters from top and displaces lighter air out thru air vent
Pre Vac are high speed sterilizers similar to gravity except they are fitted with a vacuum pump (ejector) to insure air removal from sterilizing chamber and load before steam is admitted.Advantage is immediate, instantaneous steam penetration
Name five steps for processing a scope
1. Pre Clean
2. Leak Test
3. Clean
4. High Level Disinfection
5. Proper Storage
The steps of cleaning and decontamination that occur in decontam (name 3 of 5)
1. Verification all instruments are in fully opened position
2. Verification that multipart instruments are disassembled
3. All instruments are rinsed to remove foamss or gel
4. Instruments are manually soaked in neutral ph enzymatic detergent following IFU
5. Instruments are manually or mechanically cleaned: ultrasonic washer, mechanical washers
Three types of sterile processing
What are:
•STEAM
Gravity
Pre-vacuum
•CHEMICAL
Sterrad
Ethylene oxide sterilization (EOS)
•HIGH LEVEL DISINFECTION
Combination of chemical solution and high heat
Medivator