A 72-year-old man is evaluated for an ulcerating, painful lesion on his left calf that began as a patch of red skin 2 to 3 weeks ago. He has dialysis-dependent end-stage kidney disease, atrial fibrillation, and hypertension. Medications are amlodipine, calcium acetate, calcitriol, insulin, and warfarin. There have been no recent changes in his medications.
On physical examination, vital signs are normal. Skin findings are shown. There are no other skin changes, lesions, or rash.

INR 2.5 (H)
Calcium 9.6 mg/dL (2.4 mmol/L)
Phosphorus 3.1 mg/dL (1.0 mmol/L)
Parathyroid hormone 361 pg/mL (361 ng/L) (H)
A skin punch biopsy shows calcifications in the subcutaneous tissue within necrotic lipocytes and within the walls of small blood vessels. There is confluent epidermal necrosis.
Which of the following is the most likely diagnosis?
A - Calciphylaxis
B - Leukocytoclastic vasculitis
C - Venous stasis ulcer
D - Warfarin skin necrosis
A - Calciphylaxis
- Calciphylaxis (calcific uremic arteriolopathy) is characterized by calcifications in the dermal arterioles resulting in painful ischemic skin lesions and is an increasingly recognized complication of end-stage kidney disease.
- Many patients with calciphylaxis have severe secondary hyperparathyroidism and elevated calcium-phosphorous product.
What signs can you see and what do they mean? Have to name both.
A - Chvostek's Sign: contraction of ipsilateral facial msucle while the facial nerve is tapped just anterior the ear.
B - Trousseau's sign: can be triggered by placing a BP cuff on an individual’s arm and inflating it to a pressure greater than their systolic blood pressure for 2 to 3 minutes. A positive Trousseau’s sign is defined by flexion of the wrist, the thumb, and the metacarpophalangeal joints, along with the extension of the fingers.
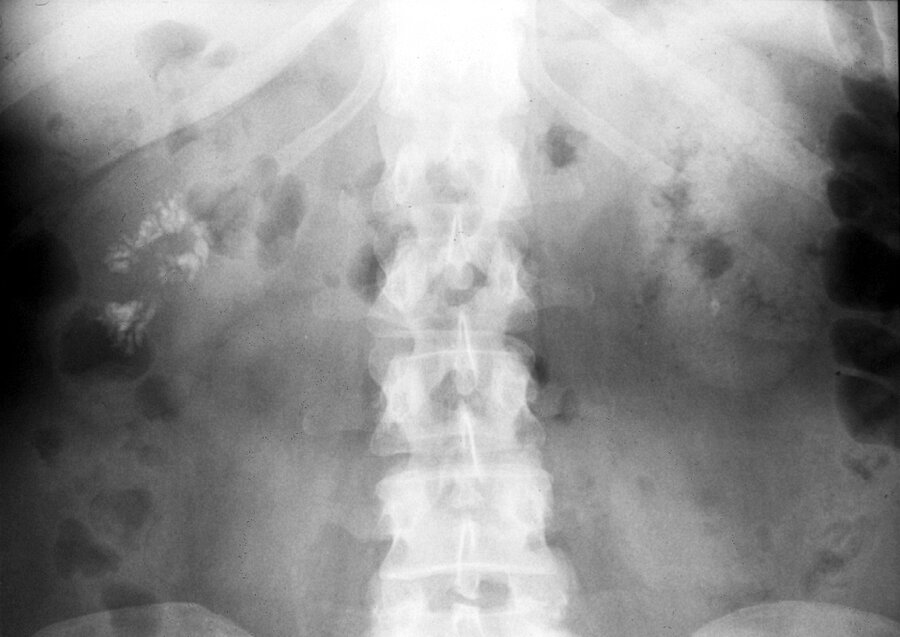
A 40-year-old woman with recently diagnosed primary hyperparathyroidism is evaluated with an abdominal radiograph:
Which of the following is the most likely diagnosis?
A - Chronic pancreatitis
B - Nephrocalcinosis
C - Nephrolithiasis
D - Renal cell carcinoma
B - Nephrocalcinosis
The most likely diagnosis is nephrocalcinosis. Nephrocalcinosis is defined by the deposition of calcium in the kidney parenchyma and tubules, which may be either macroscopic (as seen in this patient) or microscopic. It is the result of excessive excretion of calcium, phosphate, and/or oxalate in the urine with or without hypercalcemia. Severe hypercalcemia and hypercalciuria from primary hyperparathyroidism can lead to volume depletion and acute kidney injury, nephrolithiasis, or nephrocalcinosis.
A 67-year-old woman is evaluated for anemia and hypercalcemia.
Peripheral blood smear is shown.

Which of the following is the most likely diagnosis?
A - Cold agglutinin disease
B - Multiple myeloma
C - Paroxysmal nocturnal hemoglobinuria
D - Polycythemia vera
B - Multiple myeloma
This patient most likely has multiple myeloma. Increased serum proteins associated with multiple myeloma will cause rouleaux formation, or stacking of the erythrocytes, as shown. This “stacked-coin” appearance (arrow) of the erythrocytes can be seen in any condition associated with increased plasma proteins, including polyclonal or monoclonal gammopathies.
A 78-year-old man is evaluated for progressive weakness, fatigue, and myalgia over the past 6 months. He lives alone in his home after the death of his partner 4 years ago. Physical examination is noncontributory.
Albumin 3.9 g/dL (39 g/L)
Alkaline phosphatase 190 U/L (H)
Calcium 8.5 mg/dL (2.1 mmol/L) (L)
Phosphorus 2.4 mg/dL (0.78 mmol/L) (L)
Parathyroid hormone 100 pg/mL (100 ng/L) (H)
What is the best next step?
A - 1,25-Dihydroxyvitamin D measurement
B - Dual-energy x-ray absorptiometry
C - 25-Hydroxyvitamin D measurement
D - Radiographic survey
C - 25-Hydroxyvitamin D measurement
- Vitamin D deficiency may result in osteomalacia, which is characterized by diffuse bone pain, bone tenderness to palpation, and proximal muscle weakness; however, early osteomalacia may present only with low bone mass on dual-energy x-ray absorptiometry and may be indistinguishable from osteoporosis without further testing.
- Vitamin D deficiency is characterized by mild hypocalcemia, mild hypophosphatemia, increased alkaline phosphatase and parathyroid hormone levels, and a decreased serum 25-hydroxyvitamin D level.
A 22-year-old woman is evaluated in the office for a 6-month history of intermittent nausea, anorexia, and occasional constipation. She does not smoke cigarettes, drink alcohol, or use recreational drugs. She otherwise feels well and takes no medications. Family history is unremarkable.
Vital signs and physical examination are normal.
Calcium 11.1 mg/dL (2.8 mmol/L)
Creatinine 1.0 mg/dL (88.4 μmol/L)
Phosphorus 4.4 mg/dL (1.4 mmol/L)
Parathyroid hormone <10 pg/mL (<10 ng/L)
25-Hydroxyvitamin D 36 ng/mL (89.9 mmol/L)
1,25-Dihydroxyvitamin D 97 pg/mL (233.0 pmol/L) (H)
24-Hour urine calcium 450 mg/24 h (H)
Which of the following is the most appropriate additional test?
A - Chest radiography
B - Neck ultrasonography
C - Parathyroid hormone-related protein measurement
D - Urine calcium-creatinine ratio determination
A - Chest radiography
Unregulated conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D may occur in granulomatous tissue associated with fungal infection, tuberculosis, sarcoidosis, and lymphoma, leading to increased intestinal absorption of calcium.
Key points:
- Vitamin D-dependent hypercalcemia is associated with a suppressed parathyroid hormone level, hypercalcemia, a high or high-normal serum phosphorus level, and an elevated 1,25-dihydroxyvitamin D level.
- Unregulated conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D and resultant hypercalcemia may occur in granulomatous tissue associated with fungal infection, tuberculosis, sarcoidosis, and lymphoma.
A 33-year-old woman is evaluated for persistent mild hypercalcemia that was incidentally discovered several years ago. Her father also has persistent, asymptomatic hypercalcemia. The patient has no medical concerns and takes no medications. She takes vitamin D, 5000 IU, daily.
Physical examination is normal.
Calcium 10.7 mg/dL (2.7 mmol/L) (H)
24-Hour urine calcium 40 mg/24 h (L)
Creatinine 1.0 mg/dL (88.4 μmol/L)
Calcium-creatinine clearance ratio 0.008
Parathyroid hormone 40 pg/mL (40 ng/L)
Which of the following is the most likely diagnosis?
A - Ectopic parathyroid hormone–secreting tumor
B - Familial hypocalciuric hypercalcemia
C - Multiple endocrine neoplasia type 1
D - Vitamin D toxicity
B - Familial hypocalciuric hypercalcemia
The parathyroid glands and kidney detect serum calcium concentrations through the calcium-sensing receptor (CaSR). In FHH, inactivating mutation of the CaSR gene causes the parathyroid gland to perceive serum calcium levels as low, resulting in increased parathyroid hormone (PTH) secretion and a higher serum calcium level. Simultaneously, the mutated CaSR in the kidney increases kidney reabsorption of calcium, leading to paradoxical hypocalciuria in the setting of hypercalcemia. Although these patients appear to have primary hyperparathyroidism, FHH is a benign condition that will not resolve with parathyroidectomy. Patients do not have sequelae of hypercalcemia, such as stones or osteoporosis. Signs suggestive of FHH include mild hypercalcemia since childhood; low 24-hour urine calcium excretion, especially if the calcium-creatinine clearance ratio is less than 0.01; and/or family history of parathyroidectomy without resolution of hypercalcemia.
Key point:
- Signs suggestive of familial hypocalciuric hypercalcemia include mild hypercalcemia since childhood; low 24-hour urine calcium excretion, especially if calcium-creatinine clearance ratio is less than 0.01; and/or family history of parathyroidectomy without resolution of hypercalcemia.
Antihypertensive medication associated with hypercalcemia?
Thiazide diuretics
A 55-year-old woman is evaluated for hypercalcemia discovered during an emergency department visit 5 days ago. She had a 2-day history of vomiting and diarrhea that prompted her emergency department visit, where she was treated for volume depletion with intravenous 0.9% saline. She has since made a complete recovery and is asymptomatic.
Vital signs and physical examination are normal.
Blood urea nitrogen 35 mg/dL (12.5 mmol/L)
Calcium 10.7 mg/dL (2.7 mmol/L)
Creatinine 1.9 mg/dL (168.0 μmol/L)
Sodium 144 mEq/L (144 mmol/L)
Potassium 4.5 mEq/L (4.5 mmol/L)
Chloride 102 mEq/L (102 mmol/L)
Bicarbonate 27 mEq/L (27 mmol/L)
Which of the following should be measured?
A - 25-Hydroxyvitamin D
B - Ionized calcium
C - Parathyroid hormone
D - Serum calcium
E - Serum phosphorus
B - Ionized calcium
The most appropriate test to perform next is measurement of serum calcium. Total calcium is the sum of protein and anion-bound calcium as well as ionized calcium in serum. Changes in blood protein, anion content, or blood pH can transiently change total calcium concentrations. Volume loss results in an increase in the concentration of calcium in serum. Unless acute and severe, such fluctuations in binding or blood volume do not affect ionized calcium concentrations.
Key points:
- Changes in blood protein, anion content, or blood pH can transiently change total calcium concentrations.
- Unless acute and severe, transient fluctuations in calcium binding or blood volume do not affect ionized calcium concentrations.
A 55-year-old woman is evaluated for a 5-month history of fatigue and constipation. More recently, she has experienced polydipsia and polyuria. She has no other medical problems.
Physical examination findings, including vital signs, are normal. Serum albumin level is 4.5 g/dL (45 g/L), calcium level is 11.4 mg/dL (2.9 mmol/L), and phosphorus level is 2.2 mg/dL (0.71 mmol/L). Complete blood count, anion gap, and kidney function are normal.
Which of the following should be measured next?
A - Calcitonin
B - 25-Hydroxyvitamin D and 1,25-dihydroxyvitamin D
C - Ionized calcium
D - Parathyroid hormone level
D - Parathyroid hormone level
Primary hyperparathyroidism is the most common cause of hypercalcemia in the outpatient setting, and the first step in diagnosing hypercalcemia is to determine the parathyroid hormone (PTH). If the PTH level is high or “inappropriately” normal, primary hyperparathyroidism is the diagnosis. If the PTH level is suppressed, a search for other entities that cause hypercalcemia must be conducted.
A 66-year-old man is evaluated for increased confusion and lethargy over the past 2 days, as well as nausea and vomiting. He has also had diffuse bone pain that began 6 weeks ago and has worsened over the past month. His medical history is otherwise unremarkable, and he takes no medications.
On physical examination, temperature is 36.4 °C (97.6 °F), blood pressure is 110/60 mm Hg, pulse rate is 110/min, and respiration rate is 16/min. He is somnolent but can be aroused. Mucous membranes are dry, and he has decreased skin turgor. Cardiopulmonary examination is normal.
Results of laboratory studies show an albumin level of 3.8 g/dL (38 g/L), calcium level of 14.8 mg/dL (3.7 mmol/L), and creatinine level of 2.5 mg/dL (221 µmol/L).
Which of the following is the most appropriate initial management?
A - Denosumab
B - Intravenous isotonic saline and calcitonin
C - Intravenous isotonic saline and furosemide
D - Zoledronic acid
B - Intravenous isotonic saline and calcitonin
This patient has hypercalcemia, likely due to malignancy, and should be treated urgently with intravenous isotonic saline and calcitonin. Patients with severe or symptomatic hypercalcemia should receive isotonic saline volume expansion, which will increase renal perfusion and urine calcium excretion. Calcitonin increases kidney excretion of calcium and decreases bone resorption; it can decrease calcium within several hours in responsive patients. Tachyphylaxis to calcitonin may appear after 24 to 48 hours, so therapy is usually discontinued after this time period.
Key points:
- Loop diuretics are not indicated in the treatment of hypercalcemia of malignancy unless kidney failure or heart failure is present; in these circumstances, intravenous expansion of vascular volume should precede the administration of loop diuretics.
A 70-year-old woman is evaluated for incidentally discovered hypercalcemia. She has no symptoms or other medical conditions and takes no medications.
On physical examination, vital signs are normal. A height loss of 5 cm (2.0 inches) has occurred since age 65 years. Thoracic kyphosis is noted.
Calcium 10.8 mg/dL (2.7 mmol/L) (H)
Creatinine 0.8 mg/dL (70.7 μmol/L)
Phosphorus 2.5 mg/dL (0.81 mmol/L) (L)
Parathyroid hormone 77 pg/mL (77 ng/L) (H)
25-Hydroxyvitamin D 30 ng/mL (75.0 nmol/L)
24-Hour urine calcium 260 mg/24 h
Kidney-urinary-bladder radiograph is negative for kidney stones. Dual-energy x-ray absorptiometry scan shows femur neck T-score of -1.9, lumbar spine T-score -1.8, and distal one-third radius T-score of -1.7.
Which of the following is the most appropriate management?
A - Order parathyroid sestamibi scan
B - Order thoracic and lumbar spine radiography
C - Repeat serum calcium and creatinine measurement in 6 months
D - Start alendronate
B - Order thoracic and lumbar spine radiography
This patient has hypercalcemia, hypophosphatemia, and an inappropriately elevated serum parathyroid hormone level, establishing the diagnosis of primary hyperparathyroidism. For asymptomatic patients with primary hyperparathyroidism, additional evaluation is necessary to determine if parathyroidectomy is indicated. Evaluation in most patients includes assessment of kidney function, bone mineral density (BMD) measurement, and in some patients, assessment for nephrolithiasis or nephrocalcinosis. In addition to evidence of bone disease, indications for parathyroidectomy in patients with primary hyperparathyroidism include age younger than 50 years; serum calcium 1 mg/dL (0.3 mmol/L) or greater above upper limit of normal; creatinine clearance less than 60 mL/min; 24-hour urine calcium greater than 400 mg/dL (100 mmol/L); or nephrolithiasis or increased risk for kidney stones. This patient's evaluation is nearly complete except for evaluation for vertebral fractures. Because this patient's height loss and kyphosis suggest the possibility of vertebral fractures, she should undergo thoracic and lumbar spine radiography; the presence of vertebral fractures would be an indication for parathyroidectomy.
- In patients with primary hyperparathyroidism, bone-related indications for parathyroidectomy include fragility fractures, vertebral fractures, and a dual-energy x-ray absorptiometry T-score of less than -2.5 or less at lumbar spine, total hip, femoral neck, or distal one-third radius.
A 67-year-old woman presents to her primary care physician to follow up on her evaluation for hypercalcemia. She was incidentally found to have a serum calcium level 11.2 mg/dL (2.8 mmol/L) and a serum albumin level of 4.5 g/dL 6 weeks ago. Repeat serum calcium level last week was 11.6 mg/dL (2.9 mmol/L) with a serum albumin level of 4.3 g/dL. Past medical history is notable for osteopenia and hyperlipidemia. She takes simvastatin daily as well as multiple over-the-counter vitamin supplements but does not take any calcium supplementation. On further testing, her intact parathyroid hormone level is 9 pg/mL. Her parathyroid hormone-related peptide level and 1,25-dihydroxy vitamin D level are normal, and her 25-hydroxy vitamin D level is elevated.
Which of the following is the most likely diagnosis for this patient?
A - Granulomatous disease
B - Primary hyperparathyroidism
C - Vitamin A intoxication
D - Vitamin D intoxication
D - Vitamin D intoxication
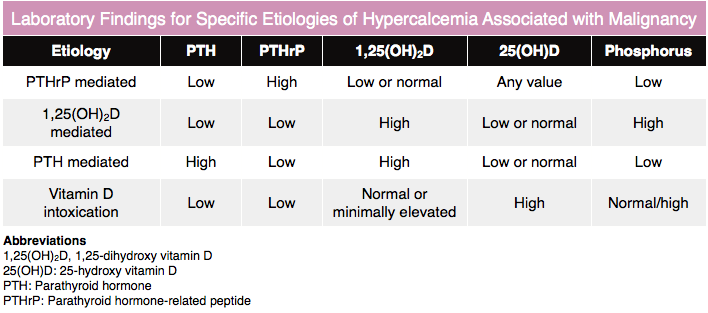 Patients without parathyroid hormone-related peptide level or 1,25-dihyroxy vitamin D level elevations but with elevated 25-hydroxy vitamin D levels are likely to have vitamin D intoxication, whereas those without elevated 25-hydroxy vitamin D levels should undergo further evaluation for other causes of hypercalcemia. Vitamin D intoxication can occur from direct ingestion of vitamin D or calcidiol.
Patients without parathyroid hormone-related peptide level or 1,25-dihyroxy vitamin D level elevations but with elevated 25-hydroxy vitamin D levels are likely to have vitamin D intoxication, whereas those without elevated 25-hydroxy vitamin D levels should undergo further evaluation for other causes of hypercalcemia. Vitamin D intoxication can occur from direct ingestion of vitamin D or calcidiol.
A 70-year-old man is evaluated in the emergency department for a 2-day history of worsening confusion as well as polyuria and polydipsia. Medical history is notable only for hypertension. His only medication is lisinopril.
On physical examination, he is disoriented. Temperature is 37.0 °C (98.6 °F), blood pressure is 105/60 mm Hg, and pulse rate is 115/min. The mouth and axillae are dry, and skin tenting is observed.
Hemoglobin 9 g/dL (90 g/L)
Calcium 13.4 mg/dL (3.4 mmol/L) (H)
Creatinine 7.1 mg/dL (628 µmol/L) (H)
Protein, total 9 g/dL (90 g/L)
Chest radiograph shows no infiltrate, but lytic lesions are seen on multiple ribs.
Which of the following is the most likely diagnosis?
A - Lymphoplasmacytic lymphoma
B - Monoclonal gammopathy of renal significance
C - Multiple myeloma
D - Smoldering multiple myeloma
C - Multiple myeloma
Key points:
- The diagnosis of multiple myeloma requires the presence of an M protein spike (may be absent in nonsecretory disease); biopsy evidence of a bony or extramedullary plasmacytoma or greater than 10% bone marrow clonal plasma cells or lymphoid cells; and disease-specific symptoms and signs.
- The CRAB mnemonic is often used to identify myeloma-specific symptoms and signs: hyperCalcemia, Renal failure, Anemia, and Bone disease.
A 77-year-old woman is evaluated for generalized weakness and diarrhea, paresthesia of the hands and feet, and perioral numbness. She has alcohol use disorder.
On physical examination, vital signs are normal. BMI is 18. Spontaneous carpopedal spasm is present, and muscle spasm can be demonstrated by percussion of the facial nerve.
Albumin 4.0 g/dL (40 g/L)
Calcium 6.5 mg/dL (1.6 mmol/L) (L)
Creatinine 1.1 mg/dL (97.2 µmol/L)
Potassium 2.8 mEq/L (2.8 mmol/L)
ECG shows QT prolongation.
Which of the following is the most appropriate next diagnostic test?
A - 24-Hour urine calcium excretion
B - Ionized calcium
C - Serum magnesium level
D - Serum parathyroid hormone level
C - Serum magnesium level
- Hypomagnesemia impairs the release of parathyroid hormone and results in renal potassium wasting.
- In patients with hypokalemia, hypocalcemia, and hypomagnesemia, it is crucial to correct the magnesium level, as it is difficult to increase potassium or calcium levels until this is done.
A 37-year-old woman is evaluated for secondary fracture prevention 3 months after surgery for a right distal radius fracture sustained from a fall. Family history is significant for low bone mass in her mother. Her only medication is an ethinyl estradiol and norgestimate oral contraceptive. Her medical history is otherwise unremarkable.
Physical examination is normal. BMI is 22.
Which of the following is the most appropriate management?
A - Bone mineral density measurement
B - Calcium supplementation
C - Fracture Risk Assessment score calculation
D - Oral contraceptive discontinuation
E - Therapeutic lifestyle interventions
E - Therapeutic lifestyle interventions (including maintenance of healthy body weight, balanced nutrition, physical fitness, abstinence from smoking, and moderation of alcohol intake)
Key point:
In otherwise healthy young adults, a low-energy fracture is not an indication for bone mineral density measurement
A 65-year-old man is evaluated for a 7-week history of increasing fatigue and poor appetite. Medical history is otherwise unremarkable. He takes no medications.
Physical examination findings, including vital signs, are normal.
Hematocrit 28%
Albumin 3.0 g/dL (30 g/L)
Calcium 10.4 mg/dL (2.6 mmol/L)
Creatinine 1.6 mg/dL (141.4 µmol/L)
Sodium 130 mEq/L (130 mmol/L)
Potassium 3.6 mEq/L (3.6 mmol/L)
Chloride 99 mEq/L (99 mmol/L)
Bicarbonate 23 mEq/L (23 mmol/L)
Osmolality 290 mOsm/kg H2O
Total protein 9.8 g/dL (98 g/L)
Urine osmolality 240 mOsm/kg H2O
Urine sodium 45 mEq/L (45 mmol/L)
Which of the following is the most likely cause of this patient's hyponatremia?
A - Hypercalcemia
B - Multiple myeloma
C - Poor solute intake
D - Psychogenic polydipsia
ESyndrome of inappropriate antidiuretic hormone secretion
B - Multiple myeloma
Results of this patient's laboratory studies, including elevated serum calcium, anemia, and elevated total protein and low albumin suggesting an increased gamma globulin fraction, support the diagnosis of multiple myeloma. The key finding, however, is that the patient has a normal measured serum osmolality in the context of hyponatremia. When evaluating a patient with hyponatremia, the first step is to measure serum osmolality. In this patient, the serum osmolality is normal, and thus he has isotonic hyponatremia. Isotonic hyponatremia (serum osmolality, 275-295 mOsm/kg H2O) is a laboratory artifact caused by the method by which serum sodium is measured. Plasma is divided into a water phase (93%), in which the sodium is dissolved, and a solid phase (7%), which consists of lipids and proteins. If the solid phase is increased by an increase in proteins, such as those found in multiple myeloma or severe elevations in serum triglycerides, there is a decrease in the water phase (i.e., from 93% to 80%).
A 62-year-old woman is evaluated after a fall, sustaining a right humerus fracture. Medical history is significant for gastric bypass surgery 10 years earlier. She takes a multivitamin and vitamin B12. She discontinued calcium and vitamin D assuming that the multivitamin was sufficient for her needs.
On physical examination, vital signs are normal. BMI is 29.
Alkaline phosphatase 92 U/L
Calcium 9.0 mg/dL (2.3 mmol/L)
Creatinine 1.1 mg/dL (97.2 μmol/L)
Parathyroid hormone 92 pg/mL (92 ng/L) (H)
25-Hydroxyvitamin D 31 ng/mL (77.4 nmol/L)
Dual-energy x-ray absorptiometry shows a left femur neck T-score of -2 and lumbar spine T-score of -2.2.
Which of the following is the appropriate next step in the evaluation of this patient?
A - Measure 24-hour urine calcium excretion
B - Measure serum 1,25-dihydroxyvitamin D
C - Order parathyroid sestamibi scan
D - Order technetium bone scan
A - Measure 24-hour urine calcium excretion
The list of potential nutrient deficiencies after bariatric surgery is extensive; replacement therapy with daily multivitamin, folate, iron, vitamin B12, calcium, and vitamin D are routinely recommended. However, this patient is no longer taking either calcium or vitamin D. Malnutrition or malabsorption of vitamin D and/or calcium may be suspected based on clinical history (bariatric surgery, celiac disease) and confirmed by low serum 25-hydroxyvitamin D level or low 24-hour urine calcium excretion (a proxy indicator of calcium intake and absorption). This patient has a normal 25-hydroxyvitamin D level, so measurement of urine calcium excretion is the next diagnostic step.
- Malnutrition or malabsorption of vitamin D and/or calcium may be suspected based on clinical history (bariatric surgery, celiac disease) and confirmed by a low serum 25-hydroxyvitamin D level or low 24-hour urine calcium excretion.
A 46-year-old woman is evaluated for a 1-year history of progressive diffuse pain in the legs that worsens with weight bearing. She also reports two episodes of acute chest pain after bending followed by chest soreness lasting weeks. She has generalized muscle weakness, a waddling gait, weight loss, and postprandial bloating. She describes no other medical concerns and takes no medications or supplements.
On physical examination, the chest and abdomen are tender to palpation over the ribs bilaterally. The remainder of the physical examination is normal.
Alkaline phosphatase 190 U/L
Calcium 7.8 mg/dL (2.0 mmol/L)
Creatinine 0.8 mg/dL (70.7 μmol/L)
Phosphorus 2.4 mg/dL (0.78 mmol/L)
A right rib radiograph shows unhealed rib fractures corresponding to the region of chest soreness. Whole-body bone scan shows increased uptake of technetium throughout the skeleton and foci of intense uptake in the ribs and pubic rami bilaterally.
Which of the following is the most likely diagnosis?
A - Bone metastases
B - Osteomalacia
C - Osteonecrosis
D - Osteoporosis
B - Osteomalacia
Diffuse signs and symptoms of skeletal disease versus an isolated low-energy fracture should raise suspicion for bone disorders other than osteoporosis. In the setting of disorders associated with malabsorption such as celiac disease or gastric bypass surgery, chronic deficiencies of vitamin D, calcium, or phosphorus can lead to osteomalacia, manifesting as impaired skeletal mineralization and low bone mineral density (BMD). Diffuse pain with weight bearing or palpation, especially if accompanied by fractures of ribs and bones of the pelvis and feet, are late presentations of osteomalacia. A progressive rise in total alkaline phosphatase precedes overt hypocalcemia or hypophosphatemia and is an early indicator that low BMD is the result of osteomalacia rather than osteoporosis. Very low levels of 25-hydroxyvitamin D, secondary hyperparathyroidism, and low urine calcium excretion could serve as corroborating evidence that this patient has osteomalacia caused by malabsorption.
Key points:
- Chronic deficiencies of vitamin D, calcium, or phosphorus lead to osteomalacia.
- In patients with osteomalacia, a progressive rise in total alkaline phosphatase precedes overt hypocalcemia or hypophosphatemia and is an early indicator that osteomalacia rather than osteoporosis is the cause of low bone mineral density.
A 57-year-old man is evaluated during routine follow-up of hypoparathyroidism. He underwent resection of locally advanced squamous cell carcinoma of the tongue base with laryngectomy, thyroidectomy, tracheostomy, and percutaneous gastrostomy tube placement 2 years ago. He also received adjuvant radiation therapy. Hypoparathyroidism developed after treatment. He has no evidence of cancer recurrence and has maintained a normal weight and hydration. Medications are levothyroxine, calcium citrate, calcitriol, hydrochlorothiazide, and potassium chloride.
Serum calcium, magnesium, and urine calcium excretion are measured today.
Which of the following measurements should also be obtained for management of this patient's hypoparathyroidism?
A - 25-Hydroxyvitamin D
B - Ionized calcium
C - Parathyroid hormone
D - Serum phosphorus
D - Serum phosphorus
Hypocalcemia is the most immediate manifestation and primary cause of symptoms attributable to hypoparathyroidism. Therefore, normalization of serum calcium is the primary goal and most frequently monitored endpoint of therapy. A reasonable goal for most patients is a serum calcium concentration at or just below the reference range without hypercalciuria. Monitoring of urine calcium excretion is mandatory because hypercalciuria often limits therapy. Correction of coexisting hypomagnesemia is also required. Thiazide diuretics are commonly used because they decrease urine calcium excretion. However, loss of parathyroid hormone (PTH)-mediated renal excretion of phosphorus may also result in hyperphosphatemia.
Key points:
- Loss of parathyroid hormone–mediated renal excretion of phosphorus may result in hyperphosphatemia.
- Initial treatment of hyperphosphatemia is reduction of dietary phosphorus but occasionally requires the addition of oral phosphate binders if serum phosphorus exceeds the normal range.
A 52-year-old woman is evaluated for hypercalcemia that was incidentally discovered during a recent office visit. Serum calcium level was 10.7 mg/dL (2.7 mmol/L) three weeks ago. She is asymptomatic, has no other medical conditions, and takes no medications.
On physical examination, vital signs are normal; the examination is unremarkable.
Calcium 10.9 mg/dL (2.7 mmol/L)
Creatinine 0.9 mg/dL (79.6 μmol/L)
Parathyroid hormone 58 pg/mL (58 ng/L)
24-Hour urine calcium 290 mg/24 h
Which of the following is the most likely diagnosis?
A - Familial hypocalciuric hypercalcemia
B - Milk-alkali syndrome
C - Primary hyperparathyroidism
D - Surreptitious thiazide diuretic use
E - Vitamin D toxicity
C - Primary hyperparathyroidism
This patient has a mildly elevated serum calcium level associated with an inappropriately normal parathyroid hormone (PTH) level. Primary hyperparathyroidism is usually caused by a parathyroid adenoma, and calcium levels are often only mildly elevated. PTH levels may be frankly elevated or inappropriately normal (typically the upper half of the reference range), as seen in this patient. Hypercalciuria may be present in up to 30% of patients. Overt hypercalciuria or high-normal levels of urine calcium, as seen in this patient, can help distinguish primary hyperparathyroidism from familial hypocalciuric hypercalcemia, which typically presents with low urinary calcium excretion.
Key Points:
- Overt hypercalciuria or high-normal levels of urine calcium can help distinguish primary hyperparathyroidism from familial hypocalciuric hypercalcemia, which typically presents with low urinary calcium excretion.
- In patients with primary hyperparathyroidism, calcium levels are often only mildly elevated; parathyroid hormone levels may be frankly elevated or inappropriately normal.
Condition characterized by low calcium, high phosphate, and elevated PTH in association with short stature, carpopedal spasm, cramping, and the 'knuckle knuckle dimple dimple' sign.
Psueodhypoparathyroidism
Patients with pseudohypoparathyroidism are hypocalcemic due to a deficient response to PTH. Hypocalcemia results in and elevated PTH level but there is no effective response in raising the calcium level towards normal. Patients have hypocalcemia with subsequent carpopedal muscle spasm, cramping, tetany and even seizures. Other features include: short stature, developmental delay, and calcification of the basal ganglia in the deep white matter of the brain. Some patients have bone resorption with blunting of the fourth and fifth knuckles of the hand which is most notable when the dorsal of the hand is viewed in a closed fist position. This presentation is known as the knuckle knuckle dimple dimple sign or archibald's sign.
Name Katerina's doggies and their breeds.
Judy (English Bulldog) and Hugo (Pug).
A 74-year-old woman is evaluated during a follow-up visit for osteoporosis. She sustained fractures in thoracic vertebra 11 and lumbar vertebra 1 without a fall 2 years earlier. Dual-energy x-ray absorptiometry scan at the time of injury showed left femur neck T-score of -2.9. Teriparatide was initiated.
Which of the following is the most appropriate management?
A - Discontinue teriparatide
B - Discontinue teriparatide, start alendronate
C - Discontinue teriparatide, start romosozumab
D - Discontinue teriparatide, start abaloparatide
B - Discontinue teriparatide, start alendronate
Although the choice of initial therapy for established postmenopausal osteoporosis always has implications for the disease course, this consideration is especially true when anabolic agents (e.g., teriparatide, abaloparatide) are used. The bone formative effect of anabolic agents rapidly declines with discontinuation of therapy whereas the increased bone resorption caused by these agents persists. Rapid loss of the newly formed bone gained during therapy ensues with discontinuation unless antiresorptive therapy, typically a bisphosphonate or denosumab, is initiated within 1 month of completing the course of anabolic treatment.
Key point:
- In patients receiving anabolic therapy for osteoporosis, an antiresorptive agent must be started within 1 month of completing the course of anabolic treatment to prevent the loss of newly formed bone.
A 39-year-old woman presents to her primary care physician for evaluation of constipation. Over the past 2 weeks, she has developed constipation without associated abdominal pain, nausea, vomiting, melena, or bloody stools. She eats a regular diet rich in fruits, vegetables, and whole grains and stays well-hydrated, avoiding caffeine and alcohol. Past medical history is notable for acne. She takes oral isotretinoin and vitamin supplements daily. Vital signs and physical exam are unremarkable. Complete blood count and comprehensive metabolic panel are notable for a serum calcium level of 12 mg/dL with a serum albumin of 4.4 g/dL. Repeat serum calcium level is 11.6 mg/dL with a serum albumin of 4.3 g/dL. Intact parathyroid hormone level is 7 pg/mL. Subsequent parathyroid hormone-related peptide, 1,25-dihydroxyvitamin D, and 25-hydroxyvitamin D levels are all normal. Serum protein electrophoresis, urine protein electrophoresis, and serum free light chain assay are unremarkable.
Which of the following is the most likely cause of this patient’s hypercalcemia?
A - Primary hyperparathyroidism
B - Pseudohypercalcemia
C - Vitamin A toxicity
D - Vitamin D toxicity
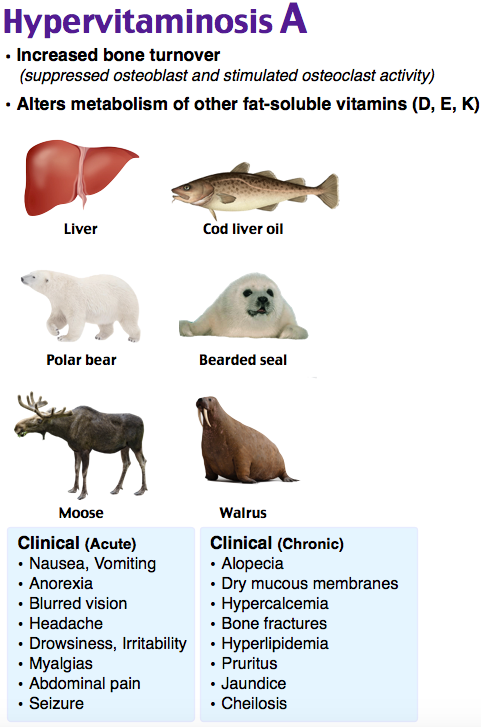
C - Vitamin A toxicity
Vitamin A toxicity is the most likely cause of this patient’s hypercalcemia. While uncommon, vitamin A toxicity can occur secondary to excessive chronic ingestion of oral vitamin A. Toxicity is unlikely to occur from beta-carotene ingestion from plant sources. Vitamin A toxicity is a rare cause of hypercalcemia, as well as other effects such as neurologic changes, vomiting, hepatotoxicity, and nonspecific changes. A patient with hypercalcemia secondary to vitamin A toxicity will classically have a normal or low-normal serum intact parathyroid hormone as well as normal parathyroid hormone-related peptide, 1,25-dihydroxyvitamin D, and 25-hydroxyvitamin D levels. Testing to exclude multiple myeloma should additionally be performed. Vitamin A excess is difficult to measure since the vitamin is largely stored in the liver, but measuring serum retinyl ester levels may aid in diagnosis.