Describe the 3 components that make up the pathophysiology of asthma.
1. inflammatory response: mast cells, macrophages, eosinophils, etc flood the airway
2. airflow constriction: bronchial wall edema and smooth muscle contraction
3. excess mucus production and hyper responsiveness (bronchospasm)
What medication is a first line respiratory therapy of asthma causing the smooth muscle of the bronchial to relax?
Bonus (+50): what are some side effects to be aware of :) name at least 2.
albuterol
SE: tremors, tachycardia, dizzy, H/A, hypokalemia
Why is bipap or HFNC used in asthmatics?
overall, temporary measure to support oxygenation or ventilation while allow medications to set in.
Where can I find the asthma CCG?
Weblinks through EPIC or all-connect
You listen to the patient, and hear no breath sounds or air movement. What do you do?
Notify your provider ASAP-this is a medical emergency.
Asthma is a curable condition? T or F.
False-chronic condition!
What are the common corticosteroids used to reduce inflammation?
Methylprednisolone (IV), Prednisone (PO/sent home on)
SE: hypertension, hypokalemia, hyperglycemia
Why is magnesium sulfate given in an asthmatic patient?
Smooth muscle relaxant-->inhibits calcium uptake
What is the LCAS? What does it stand for? How do you use it?
Lurie Children's Asthma Score (LCAS)
Objective way to measure severity using respirations, WOB, oxygen requirement, and air exchange.
Will determine frequency of albuterol
Why are asthmatics at higher risk of a cardiac arrest?
-severe bronchospasm leading to mucus plugging
-prolonged hypoxia can lead to cardiac arrhythmia
-increased intrathoracic pressure can limit venous return ("clamping")
Name 2 common triggers for asthma?
Allergens: dust/mites, mold, animals, pollen, trees
Irritants:smoke, perfumes, paints
Infection
Exercise
What medication is given IM to help with bronchodilation and counteract the histamine attack of asthma?
Bonus (+50): for your safety and patient's safety, what precaution should be taken when preparing this medication?
Epinephrine
Bonus: crack with nipple bottle and draw up with filtered needle
Why do we hesitate (or have a high threshold) to intubate asthmatics?
-at risk for bronchospasm and incresae in airway resistance--harder to intubate
-hypotension due to change from negative to positive pressure by impending venous return to heart
-hard to ventilate
What is one extra step you should remember when planning discharge paperwork for an asthmatic?
Asthma Action Plan
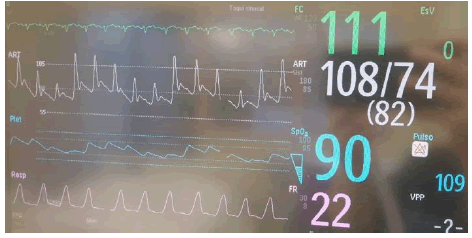
Pulsus Paradoxus: drop in BP (wave-like look), due to increased intra-thoracic pressure.
Bonus: what intervention can you anticipate that may help with this?
Describe 2 common clinical presentations for a patient with asthma?
wheezing, coughing, chest pain/tightness, SOB, increased WOB.
What IV medication is started when your patient is not responding to albuterol?
Bonus (+50): what intervention should be considered prior to starting?
Terbutaline
SE: cardiac considerations (arrhythmias, electrolyte abnormalities, ST depression, prolonged QTC) YIKES! Grab an EKG.
Your asthmatic patient is not improving, despite lots of intervention. Your team is planning on intubating. What sedative would you anticipate using?
ketamine! Why?
bonus (+50): what sedative would you anticipate avoiding?
You have a patient on continuous albuterol and HFNC. Would you expect to wean off your albuterol first or HFNC first?
First albuterol, then can wean respiratory support.
You are taking care of your intubated asthmatic and you notice their PIPs on the home screen of your Drager are in the high 40s. What's going on here? What should you do?
-ask your respiratory therapist to check the "peak v. plateau"
-this will determine what is really going in in your alveolar and more indicative of lung compliance
-the peak is the resistance or high pressure It is taking to deliver ventilator support
Your team decided to intubate your asthmatic patient. Once the patient is stable and placed on their vent with an end tidal in line, you see on the monitor a "shark fin" end tidal shape. What's going on here?
Indicative of obstruction, but why?
What is IV bronchodilator is commonly used as a continuous gtt in the PICU?
aminophylline
Bonus (+50): what daily lab value can you anticipate needing?
You patient is intubated and placed on a ventilator. What is at least one setting you could anticipate seeing when looking at your settings/orders?
-short i:time
-low RR
-low TV
-auto-peep present (why?)
*overal goal: minimize hyperinflation*
You admit a patient from the ED with a history of asthma in respiratory failure, testing positive for the R/E. On arrival, they are on continuous albuterol and HFNC. True or false--you complete q2 assessment.
False: q1 respiratory assessments are indicated for this patient.
*If the patient is on continuous with ETT or bipap, then they are excluded from this.
You are taking care of an asthmatic that was just intubated. Your team mentions you we may be escalating to an anesthesia vent? What is this used for and what can you anticipate?
-inhaled anesthetics (i.e. Isoflurane/Halothane) used for bronchodilation effects
-tell charge so you can move to a negative pressure room if already there