What is the name of the risk scale used in hospitals for DVT?
Name two congential stuctural issues in the chest wall? (musculoskeletal causes of restrictive diseases)
Pectus Carnivatum (pigeon chest)
Pectus Excavatum (funnel chest)
What are the types of emphysema?
Panacinar: alveoli within an acinus are uniformly destroyed.
Centriacinar: affects alveoli arising from resp bronchiole or proxima acinus.
Paraseptal: enlarged airspace at the periphery of the acinus
What blood test is used to diagnose vasculitis?
ANCA: Antineutrophil cytoplasmic antibodies
Location for Arterial vs Venous ulcers
Venous: medial ankle
Arterial: Distal toes, foot, lateral ankle
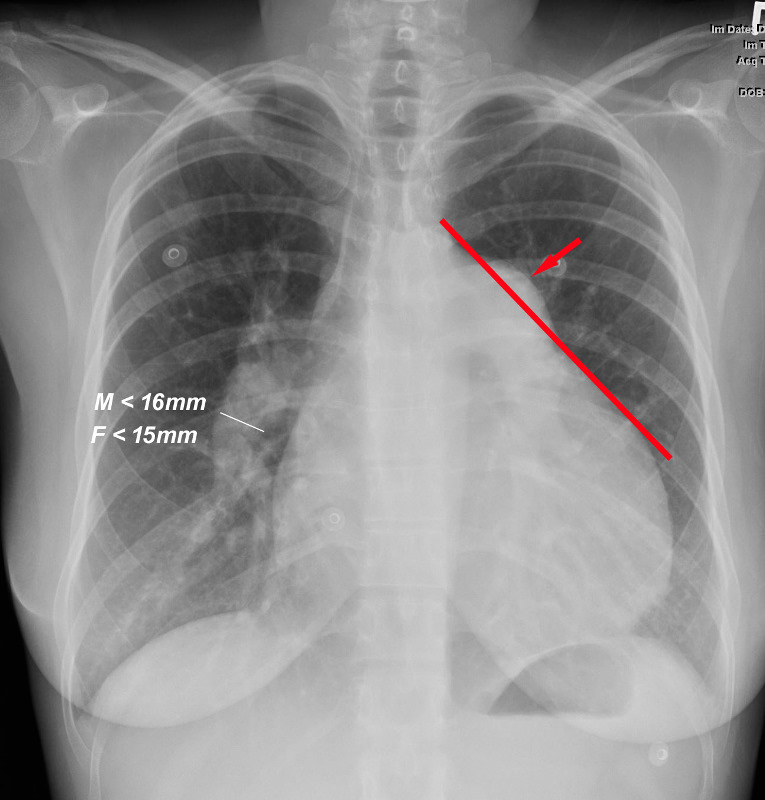
What will be found on an X-ray that will indicate pulmonary hypertension.
Prominent pulmonary artery on x-ray.
Describe Cystic Fibrosis?
Multi-system hereditary disease of exocrine
glands. Recessive trait: defective gene on chromosome #7
• Inability to move chloride in and out of cells
• Salt accumulates on lung and digestive tissue
• Mucous becomes abnormally thick
• Obstruction of bronchioles by mucous plugs
Can develop barrel chest over time, 2 positive sweat tests (sweat chloride above 6 mEq/L)
Layers of skin (thick and thin)
CLGSB-Thick Skin (palms and soles)
Stratum Corneum, Lucidum, Granulosum, Spinosum, Basale
CGSB-Thin Skin
Stratum Corneum, Granulosum, Spinosum, Basale
What is the difference between arteriosclerosis and atherosclerosis?
Arteriosclerosis is the hardening or narrowing of arteries
Atherosclerosis is the build up of plaque on arterial walls
Ulcer margin for arterial vs venous
Venous: Irregular
Arterial: Smooth, round, punched out
What is Cor Pulmonale?
Changes in the structure and function of the right ventricle as a result of prolonged pulmonary hypertension
• Hypertrophy
• Dilation
• Failure
• Seen in chronic lung disease
What are the two types of asthma?
Extrinsic (identifiable triggers; common in kids)
Intrinsic (no identifiable triggers, develops later in life)
Partial thickness integumentary wounds heal by_____________
Full thickness integumentary wounds heal by________
regeneration
repair
Loss of normal capillary network between higher pressure arterial to venous
Arteriovenous Malformations
Venous: yellow slough or red granulation
Arterial: Black or pale pink granulation
What are the 4 types of cancers involving the lungs?
Squamous cell: centrally located in segmental bronchi, bulky, and causes obstructive disease.
Small cell: any part of bronchial tree widespread metastasis
Adeno-carcinoma: involves the pleura
Large Cell carcinoma: involves the chest wall
What is the difference between asthma inducers and triggers?
Inducers of asthma act by inducing airway inflammation which leads to AHR.
• Genetic factors
• Allergies
• Infections
• Occupational/environmental
Triggers of asthma are factors that cause airway smooth muscle contraction and asthma symptoms on a background of pre-existing airway responsiveness
• Exercise
• Irritants
• Smoke
• Polutants
Allergens are important as both inducers and triggers
• Dust Mites
• Fungi
• Pets
• Pollens
• Food: sulpher dioxide (preservative)
Describe what happens in each stage of wound healing.
Hemostasis: (first few hours- goal is to stop bleeding) Platelets, Fibrin; Vasoconstriction, Platelet adhesion, activation & aggregation
Inflammation: (1-4days) Clean & clear debris,
granulation foundation -pain, swelling, warmth, red
- Mast Cells (histamine)
– Platelets: fibrin clot, growth factors
– Neutrophils: (↑first 24-48 hrs) kill bacteria
– Macrophages: cleans debris & destroy bacteria, secrete collagenase, growth factors, lactate
Proliferation: (3-60days) Rebuilding: angiogenesis,
fibroplasia, re-epithelialization
Fibroblasts →→ Granulation Tissue
• collagen, elastin, growth factors, proteoglycans &
fibronectin
• able to differentiate into myofibroblasts
Myofibroblasts →→ Wound Contraction
Angioblasts →→ bl. vessels
Keratinocytes →→ Re-epithelialization
Remodeling (2+years): Scar formation-collagen crosslinking, scar tissue strengthens
What are the 6 P's of PAD?
Pulselessness
Pain
Pallor
Poikilothermy
Paresthesia
Paralysis
Edema, venous vs arterial
Arterial: Minimal unless leg in dependent position
Describe the pathophysiology of COVID 19?
Crown shaped virus (spikes) enter lungs and bind to ACEII receptor. It multiplies inside the body and eventually will cause a full inflammatory response which in some will cause ARDS. This leads to damages to the basement membrane of the alveoli and type II pneumocyte.
What is a key feature of asthma?
Episodic in nature
Superficial inflammation of the skin, caused by irritant exposure, allergic sensitization, or genetic idiopathic factors.
3 primary stages: Acute, Subacute, Chronic
Eczema/Dermatitis
Indicates a Positive Buerger's Test for PAD
_______ with elevation
_______ with dependency
Pallor with elevation
Rubor with dependency
Periowound skin, arterial vs venous
Venous: hemosiderin staining, lipodermatoslcerosis
Arterial: Pale, thin, shiny, hairless, rubor of dependency