What is an Arterial Blood Gas (ABG)?
The arterial oxygen tension (partial pressure or PaO2) indicates the degree of oxygenation of the blood, and the arterial carbon dioxide tension (partial pressure or PaCO2) indicates the adequacy of alveolar ventilation. ABG studies aid in assessing the ability of the lungs to provide adequate oxygen and remove carbon dioxide and the ability of the kidneys to reabsorb or excrete bicarbonate ions to maintain normal body pH.
What are the questions to ask when a patient states they are having pain when taking a deep breath?
Rate 1-10, describe, how long, what makes it worse or better, increased with inspiration or expiration, have you ever had this discomfort, does it radiate any where,
Name 2 causes for Respiratory Acidosis.
Hypoventilation
Respiratory Depression
Asthma
COPD
Pneumonia
Pulmonary Edema
Name 3 causes of Respiratory Alkalosis.
Hyperventilation
Hypermetabolic states: Fever, anemia, septicemia
Anxiety
fret
pain
pneumothorax
Patient has hoarseness, weight loss, history of smoking what may the patient have?
Hoarseness is an early symptom of laryngeal cancer. Dyspnea, dysphagia, and lumps are later signs of laryngeal cancer.
Assessment of the airway patency is paramount
What are the differences between wheezes and crackles when auscultating lung sounds?
wheezes-narrowed airways
crackles-fluid accumulations
What are the first signs of hypoxia?
There is inadequate gas exchange depends on an adequate ventilation-perfusion ratio therefore, S/SX include restlessness, agitation, change in LOC
Name 3 signs and symptoms of Respiratory Acidosis.
bradycardia
Hypotension
Agitation-altered metal status trouble staying awake, retaining Co2
Confusion
Lethargy
Coma
Name 2 signs and symptoms of Respiratory Alkalosis.
Tachycardia
anxiety
confusions
diaphoresis
dizziness
coma
I arrive at the ER after playing football, and my nose is misshaped and bleeding. I have ice on my nose while being told to keep my head elevated. Why the ice and told not to lay down?
Possible nasal fracture.
Swelling: dependent will cause increase bleeding
remain upright t decrease bleeding and airway protection
What is tidal volume?
Tidal volume refers to the volume of air inspired and expired with a normal breath.
When entering a patient's room and you notice the o2 sats is 88%, what are 2 nursing interventions?
Assess:
can the patient speak in full sentences
Assess lungs
Is the reading accurate?
Normal level of oxygen is usually 95% or higher if lower start with 02 nasal cannulas at 2 liters.
If the patient decompensates and has COPD use a Venturi mask because it can accurately provide an appropriate level of supplemental oxygen, thus avoiding the risk of suppressing the hypoxic drive.
The nasal cannula is a low-flow oxygen delivery method that gives the patient 24% - 44% FiO2 at a rate of 1 – 6 lpm, each additional 1 lpm of oxygen increases FiO2 by 4%; a venture mask is an accurate high-flow oxygen delivery system
Name 2 Causes of Metabolic Acidosis
Acid increase: Keto Acidosis, starvation, Lactic Acidosis: Shock hypoxemia
Decreased Bicarbonate: severe diarrhea, renal failure
What are two causes of Metabolic Alkalosis?
Antacids
Hyperaldosteronism; Cushing's disease, steroids'
Acid loss by: vomiting, gastric suctioning, Diuretics-K+/NA+ loss
I snore loudly, periods of apnea, excessive daytime sleepiness what am I? What can you do for me?
OSA
CPAP or Bipap
What is spirometer used to assess?
What are they used for?
Spirometer is used to assess/measure the volume of air inspired and expired with a normal breath
Incentive spirometer is used to promote deep breathing and prevent pneumonia and atelectasis; it should be used 10 times every hour in a semi-Fowler or upright position; nurse should encourage the patient to cough during/after to mobilize secretions
What is an essential factor when patients are prescribed antibiotics?
Is it viral or bacterial
Length of symptoms
Name 3 signs/Symptoms of Metabolic Acidosis.
Headache, lethargy, Kussmauls's respiration, Nausea, vomiting, confusion. coma
What are two signs/symptoms for Metabolic Alkalosis?
weakness muscle cramps, hyperactive reflexes, tetany, confusion, slow shallow respirations to minimize co2 loss(Body needs this to counter alkalotic state), nausea, seizures
Viral infection of upper respiratory tract
Characterized by inflammation of nasal mucosa
Viral rhinitis, AKA Common cold
Most frequent respiratory infection (~ 2 – 3/year)
Transmitted via direct contact (hands, fingers)
Sore throat, rhinorrhea (mucus), congestion, cough, sneezing
Malaise, fatigue, headache, fever (children)
URI: Rhinitis
What is pulmonary function test (PFT) ?
PFTs are routinely used in patients with chronic respiratory disorders. They are performed to assess respiratory function and to determine the extent of dysfunction. Such tests include measurements of lung volumes, ventilatory function, and the mechanics of breathing, diffusion, and gas exchange. Lung elasticity and diffusion can often be implied from PFTs, but they are not directly assessed
What are the nursing interventions with URI? Name 2
URI treatment, non-pharmacologic:
Saline mists, sprays, vaporizers: Moisten nasal mucosa
Salt water gargles: reduce swelling, loosen mucus
Promote fluid intake, rest (avoid alcohol, caffeine which can cause dehydration & interact w/medications)
Avoid irritant exposure (smoke, allergens, etc.)
Assess, monitor pain
Maintaining Patent Airway:
Resp assessment for changes to work of breathing
Promote expectoration of secretions (hydrate, moisten air, upright position to promote drainage)
Reduce risk of aspiration (upright position)
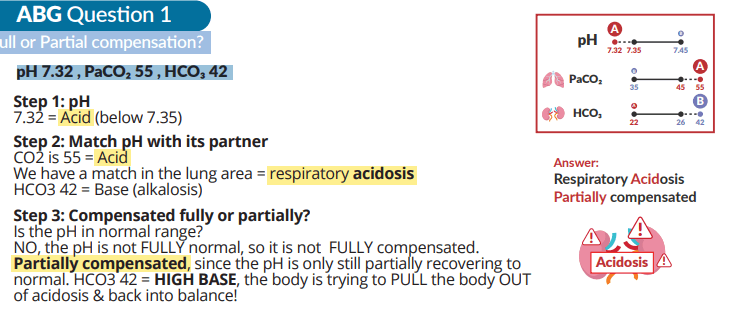
What am I in when you see my ABG?
pH 7.32 , PaCO₂ 55 , HCO₃ 42
Respiratory Acidosis Partially compensated
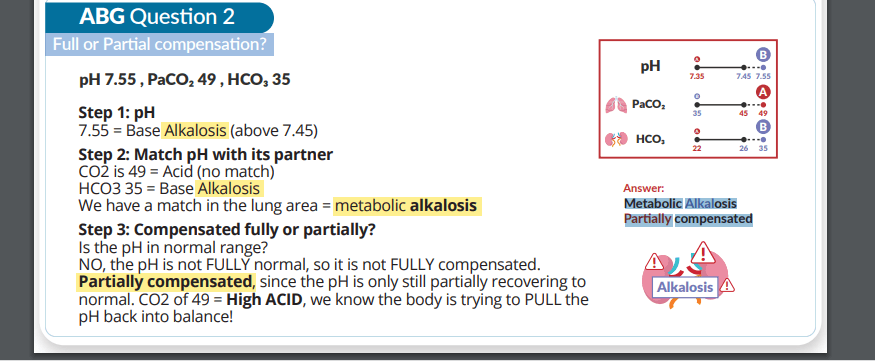
What am I in when you see my ABG?
pH 7.55 , PaCO₂ 49 , HCO₃ 35
Metabolic Alkalosis Partially compensated
What is this?
Etiology, Risk factors:
Edema from allergy (anaphylaxis), burns, infection
Foreign body: inhalation or ingestion
Hereditary angioedema: recurrent laryngeal edema
Assessment:
Resp: decreased Sp02, increased breathing effort
Sensation of inadequate airflow (anxiety)
Medical management:
Resolve cause if foreign body, restore airway patency
Head-tilt, chin-lift; sweep mouth for foreign objects
Laryngoscope to visualize, forceps to remove
Immediate tracheotomy if can’t resolve
Laryngeal Obstruction