This rhythm is rarely treated by paramedics in the field

A-Fib
Identify the name of this drug and when to use it
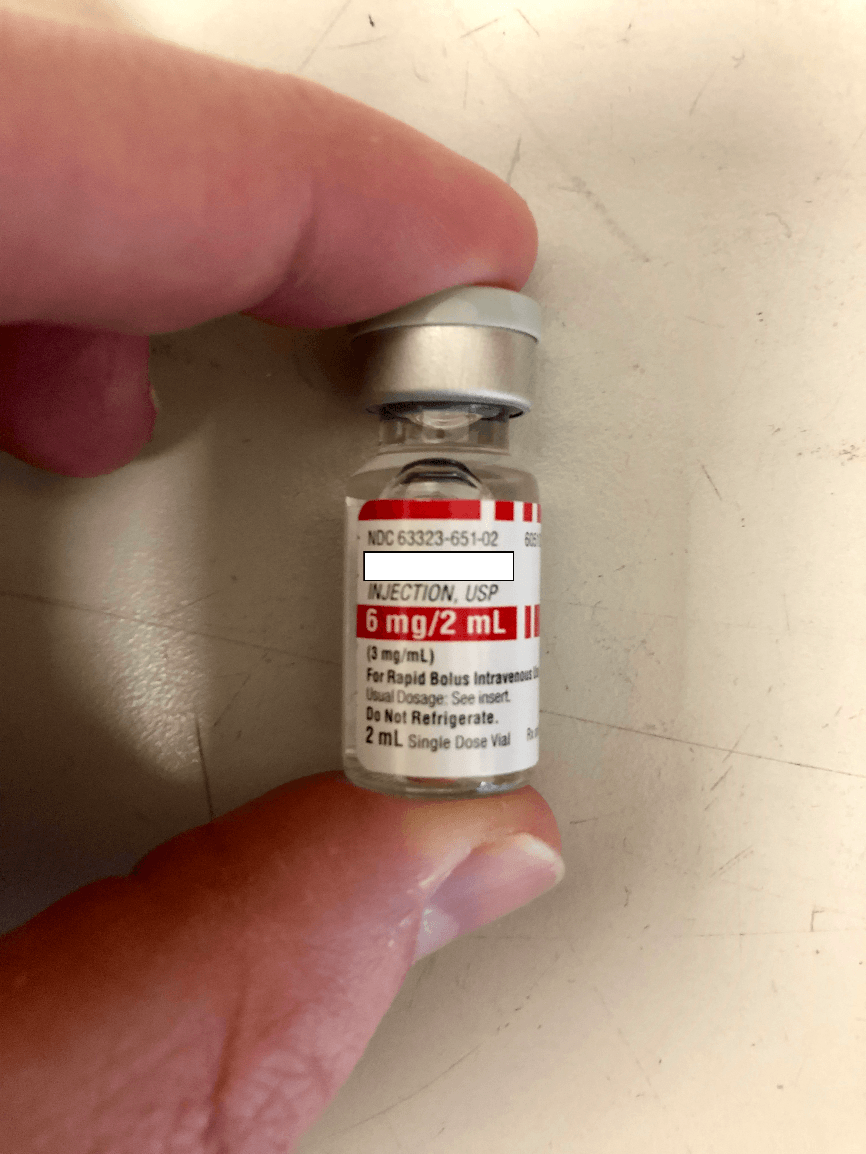
Adenosine, Stable SVT
You have a pt. in v-fib and are ready to shock for the first time, what is the appropriate dose?
120 Joules
You have a pt. in PEA, what medicine and dose is appropriate to administer
Epi 1:10,000 1 mg
Pt. is in V-Fib, you are defibrillating for the 2nd time, what is your dose?
150J
This rhythm can be easily distinguished by its "sawtooth" P waves
Atrial Flutter
What drug is this? How many mg's in how many ml's?
Epi 1:10,000, 1mg in 10 ml
Your patient is stable and has a regular pulse rate of approximately 200, you have attempted the vagal maneuver unsuccessfully, what is your next treatment?
Adenosine 6mg
You have a pt. that has been in V-Fib for the past two rhythm check, defibrillation has been attempted and Epi has been administered appropriately, what is your initial dose of amiodarone for this pt.?
300mg
In order, what are your defibrillation doses for an adult pt. in v-fib
120J, 150J, 200J
An MI should be highly suspected with this rhythm
3rd degree block, CHB
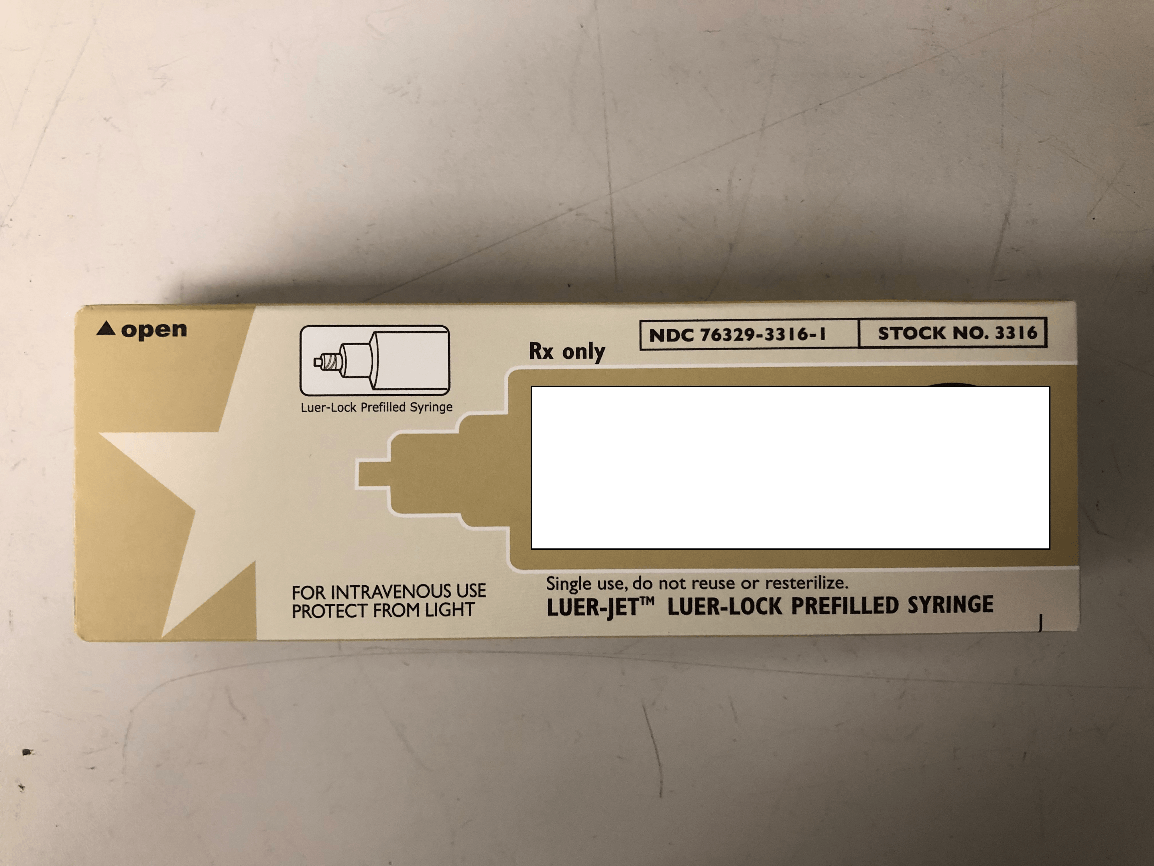
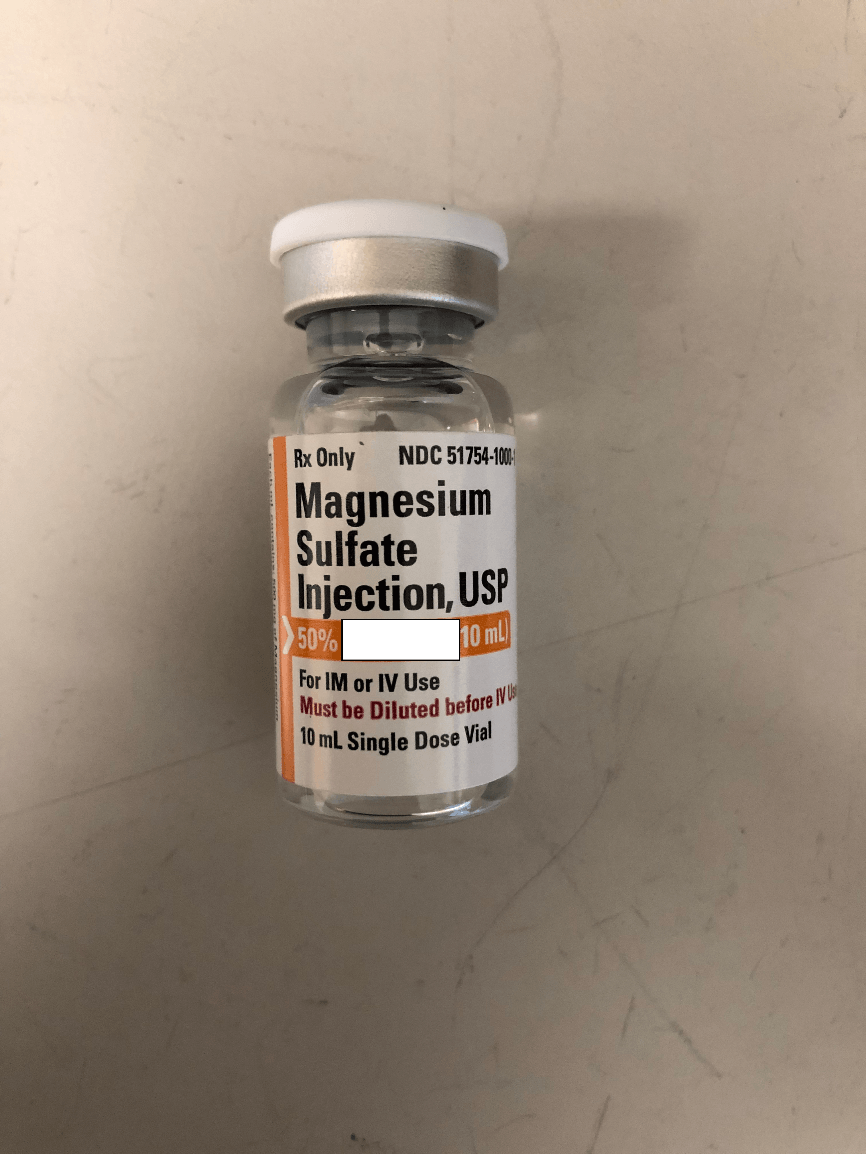
What is the name is this medication? How many mg's in how many ml's?
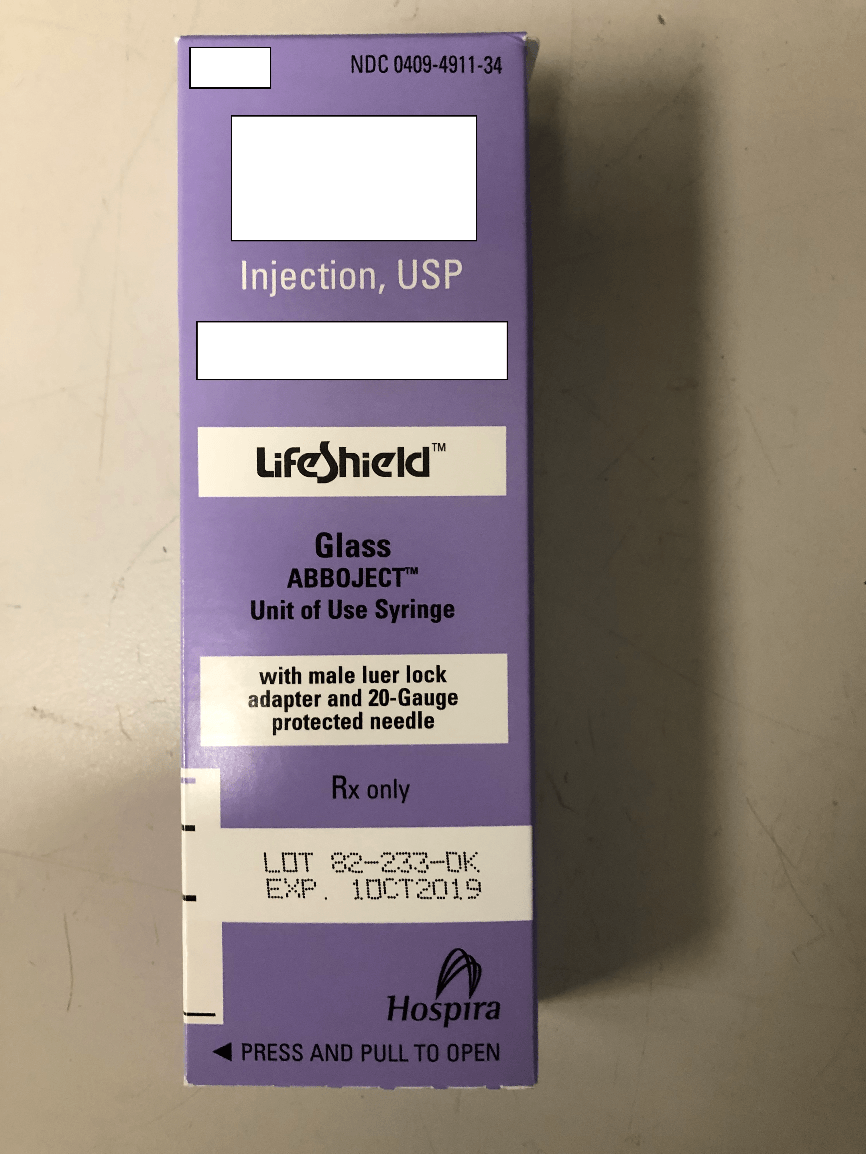
Atropine, 1 mg in 10ml
This medication is routine in all non traumatic cardiac arrests
Epinephrine 1:10,000
A woman calls st. 40 for her husband who is "feeling funny". As you walk in the pt. is sitting in his recliner reporting he is having some difficulty breathing, but does not present in significant respiratory distress. Pt. also reports some chest pain that began just before EMS arrived on scene. You begin your assessment including vitals: BP: 112/74, pulse 38, O2 sat.- 98%, blood glucose- 118 mg/dl. You apply a three lead to confirm the pulse and a 12-lead to evaluate the presence of an MI. No MI is noted. You note a bradycardic rhythm, with rate confirming your earlier findings. You decide to try medicaitons before pacing due to your pt. condition. What medication and what dose would you administer?
Bonus: What is your total max dose of that medication?
.5mg Atropine
3mg Total
You have decided to pace a bradycardic pt. what is our monitors initial milliamps?
20ma
This rhythm is usually wide and very sloooooooooowwwww
Idioventricular Rhythm
How many mg's in how many ml's in total in this vial? How many of these are carried in the drug bag?
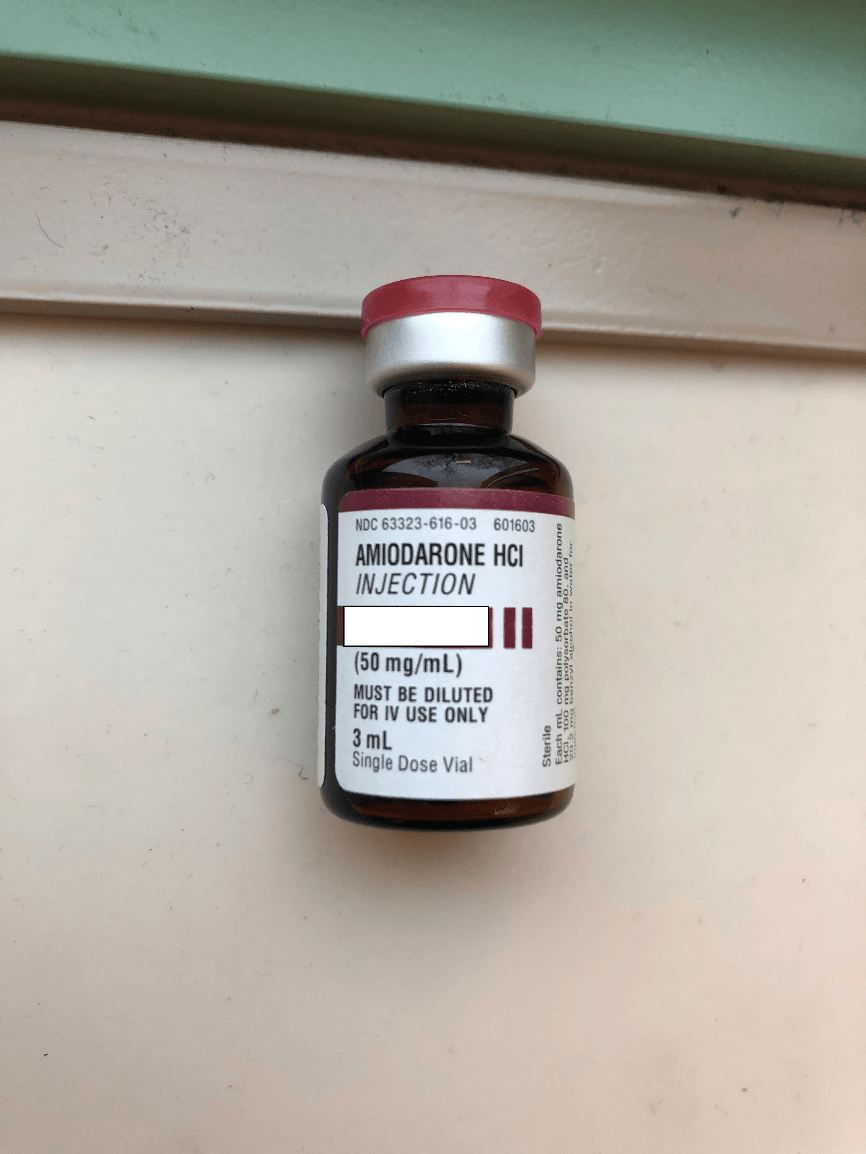
150mg/3ml, 3 carried in total
You have a pt. experiencing crushing chest pain, SOB a BP of 90/70. The pt. has a lengthy cardiac hx. including stints, heart attack and previous cardiac arrest, he is displaying a wide complex rhythm with a pulse at a rate of approx. 150. What should your treatment be (medications or electricity), and what is your dose?
Synchronized Cardiovert at 75J
You have a pt. displaying a narrow complex tachycardia and is presenting stable (negative- CHAPS) you have administered two rounds of Adenosine, how many mg's total have you given?
18mg
You have found a pt. in pulseless v-tac and are preparing to utilize the zoll, are you going to defibrillate or cardiovert? What is your dose?
Defibrillate at 120J
This rhythm usually has a lengthening PR interval followed by a dropped beat
Wenkebach, second degree type I
How many G's are in this vial and how many would you give to someone in Torsades De Pointes
5G total, 2G over 10 minutes
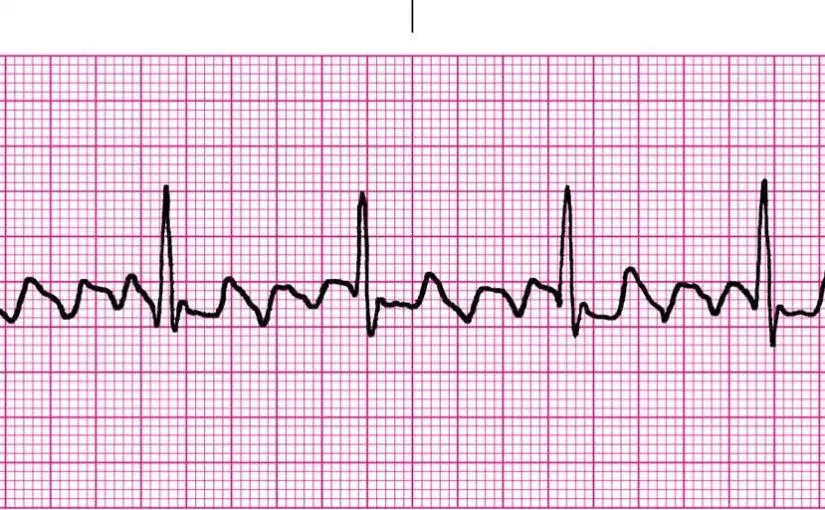
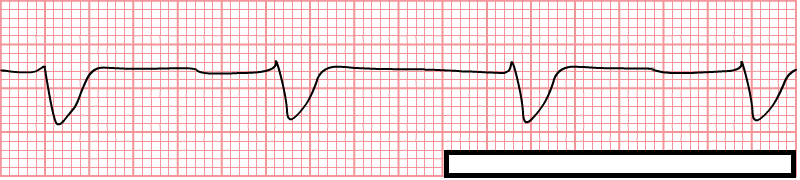
A 65 year old male is found on scene, pt. is reporting a recent headache and nausea. Pt. presents A&Ox4 and GCS-15. After your assessment you note a BP of 134/86, blood glucose of 97mg/dl, pulse of 154, lungs clear bilaterally. Pt. denies any chest pain or shortness of breath. You obtain a 3-lead to confirm your pulse and you see this on your monitor? What is the most appropriate treatment. 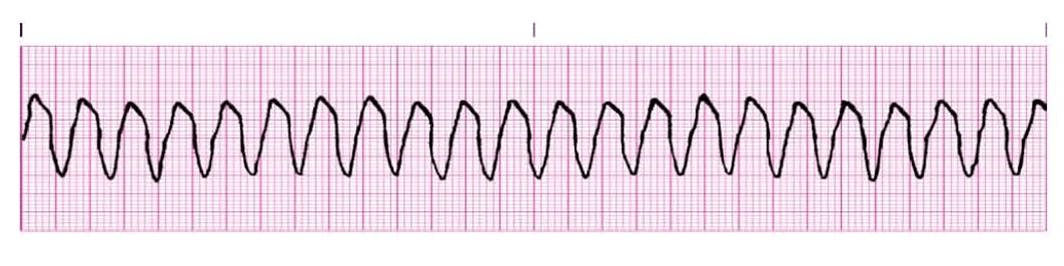
Pt. is in stable v-tac, the most appropriate treatment is 150mg Amiodarone over 10 minutes
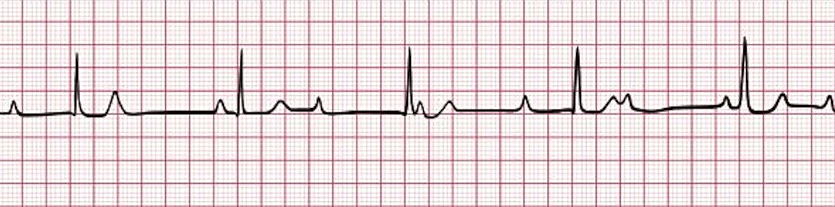
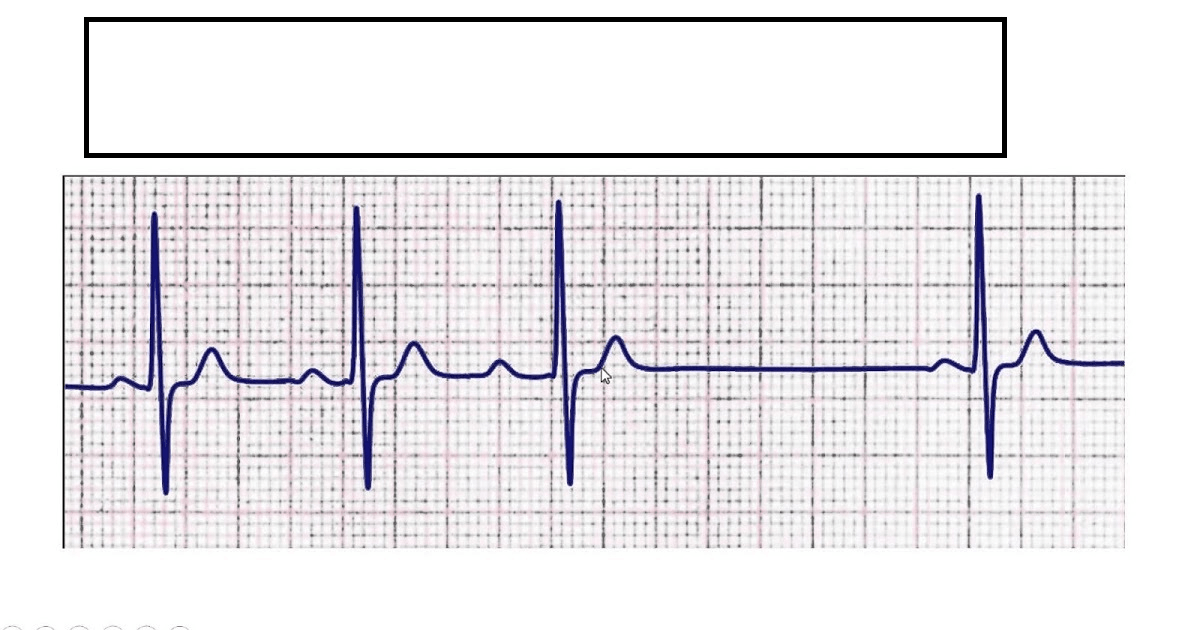
You have a post cardiac arrest pt. that you have successfully resuscitated that is now displaying this rhythm. What is this rhythm? What drug do we carry that we can administer to this pt.? What would your dose be and how would you administer it?
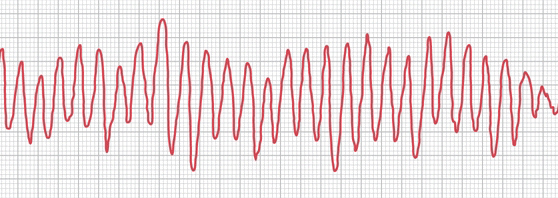
Torsades, magnesium sulfate, 2G. over 10-15 minutes
Correctly describe the doses in order for cardioverting off the zoll monitor
75J, 120J, 150J, 200J