(and Burkitt)
oh my!
What is the most frequent gene rearrangement in adult ALL?
t(9;22)
Found in ~30% of adult ALL. Results in the Philadelphia chromosome.
Which nerve in the face is commonly involved in patient's with Burkitt lymphoma?
Mental nerve.
50% of patients report chin numbness.
What is the mechanism of action of blinatumomab?
B-specific T-cell engager that targets CD19 on B-cells.
What age range is considered to be adolescent and young adult?
Age 18-39
This age group has been shown to have improved event free survival of 64% with pediatric inspired regimens containing daunorubicin, vincristine, steroids and asparaginase when compared to adult regimens (EFS 34%)
What is the mechanism of the BCR-ABL1 fusion protein?
Results in constitutively active tyrosine kinase.
Name two cytogenetics that are considered poor risk.
Hypodiploidy
Complex karyotype (> 5 chromosomal abnormalities
Ph-like
t(4;11)
11q23 (MLL rearrangement)
Name two translocations associated with Burkitt Lymphoma
t(8;14), t(8;2), t(8;22)
TKI of choice in Ph+ ALL?
Dasatinib
A multi-targeted TKI that has activity in Ph+ ALL resistant to imatinib.
Name 2 common adverse effects associated with 'BFM' regimen (daunorubicin, steroids, vincristine, asparaginase).
20% - Asparaginase allergy (hypersensitivity ranges from localized skin reaction to anaphylaxis)
35%- DIC
~40%- Elevated LFTs/bilirubin
85M with T2DM, HFrEF, HTN presents with malaise and weight loss. BMB shows +Ph ALL. What treatment is offered?
TKI + steroids
High rates of CR and well tolerated but likely to be followed by relapse.
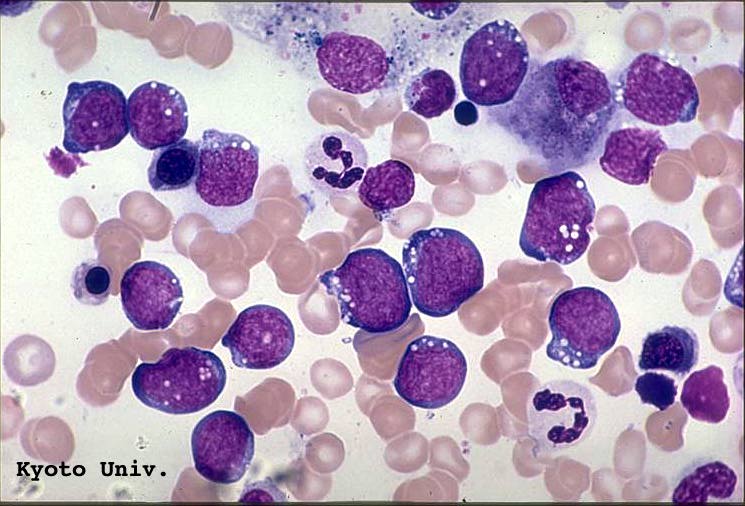
What is the diagnosis?
Burkitt's Lymphoma
Characteristic vacuolated cytoplasm and 'starry sky' appearance
What is the preferred CNS prophylaxis?
Intrathecal methotrexate.
Generally cranial radiation is no longer used due to neurotoxicity.
What is the target of Ponatinib?
T3151.
In Ph+ 25% have this mutation and it is the predominant clone in 75% of Ph+ patients that relapse. The mutation confers resistance to other TKIs.
50M presents with fatigue, abdominal distension. WBC 72k with 37% blasts. BMB shows TdT+, CD3, CD7. What are some characteristic sites of disease in this diagnosis?
T-ALL often presents with marked leukocytosis, CNS, mediastinal and testicular involvement.
48F with no pmhx presents to the ED with fatigue, bone pain, epistaxis x 4 weeks. Labwork shows anemia, neutropenia, thrombocytopenia. BMB shows small to medium sized lymphoblasts with uniform appearance and scant cytoplasm. Cytogenetics show t(9;22) in all metaphases. Which therapy do you offer?
HyperCVAD + TKI
Previously Ph+ conferred a poor prognosis though that has improved dramatically with addition of TKIs (OS from 35% to 60%)
58M presents with fatigue and pallor. CBC shows WBC 8.9k (29% blasts), Hb 9.2, Plt 65k. Bone marrow biopsy shows CD1a negative, CD8 negative, absent/weak CD5, CD34 positive. What is the diagnosis?
Precursor T-ALL
Characterized by CD1a negative, CD8 negative, absent/weak CD5 and 25% have > 1 myeloid marker (CD117, CD34, HLA-DR, CD13, CD33)
In a patient suspected of having Burkitt lymphoma, in addition to CBC and BMB, what other workup must be included?
CMP, LDH, uric acid - high risk of TLS
Also hepatitis B if planning to use rituximab
What is the indication for CAR-T in ALL?
Tisagenlecleucel (Kymriah) is approved for precursor B-ALL in patients < 26 years old in second or later relapse.
68M with T-ALL presents with relapse after initial therapy with hyperCVAD + high dose methotrexate. He is started on second line chemo but has a second relapse. What therapy do you offer next?
Nelarabine
Nelarabine is a pro-drug of ara-GTP approved in patients with T-ALL who have relapsed following two chemotherapy regimens. German study of 126 patients showed 36% with CR; 80% of CR patients were able to proceed to stem cell transplant.
52M with Ph+ ALL undergoes hyperCVAD with imatinib and obtains complete remission. He is MRD negative. What therapy do you offer at this time?
Allogeneic transplant.
If donor is available therapy with allo-transplant should be offered after CR is obtained.
What are the molecular alterations in Ph-like ALL?
80% have CRLF2 rearrangement which results in an aberrant cytokine receptor. 50% of these have JAK2 mutation though they are usually not responsive to ruxolitinib. Add blinatumomab or ?venetoclax in the future
20% without CRLF2 rearrangement have ABL fusions and can be treated similarly to Ph+ ALL (ie chemo + TKI)
34M presents with chin numbness, fatigue and pallor. WBC 57k with 50% blasts. BMB shows t(8;14) translocation. What therapy do you recommend?
Short term dose intense chemotherapy: HyperCVAD x 8 with 16 intrathecal treatments. Rituximab improves survival (add with second cycle to minimize risk of TLS)
No role for maintenance therapy or transplant.
Black box warning with inotuzumab?
Hepatotoxicity including veno-occlusive liver disease known as sinusoidal obstruction syndrome.
65M with pre-B cell ALL completes hyperCVAD+rituximab. Bone marrow after cycle 1 shows MRD positivity. What therapy do you offer?
In studies 80% of patients who received Blinatumomab became MRD negative, improving OS to 40% from less than 25%
79M with Ph+ ALL underwent TKI+steroids but has relapsed. He is frail and not eligible for transplant. What therapy do you offer?
Blinatumomab or Inotuzumab
Inotuzumab can be administered in the outpatient setting and is better tolerated than Blinatumomab. Blast cells must be CD22+ (found in 90% of adults)