The medical name for "Nearsightedness "
Myopia - difficulty seeing objects in the distance, but can see near objects clearly)
Near vision is tested by asking a person to read the small print on this chart
Jaeger Eye Chart
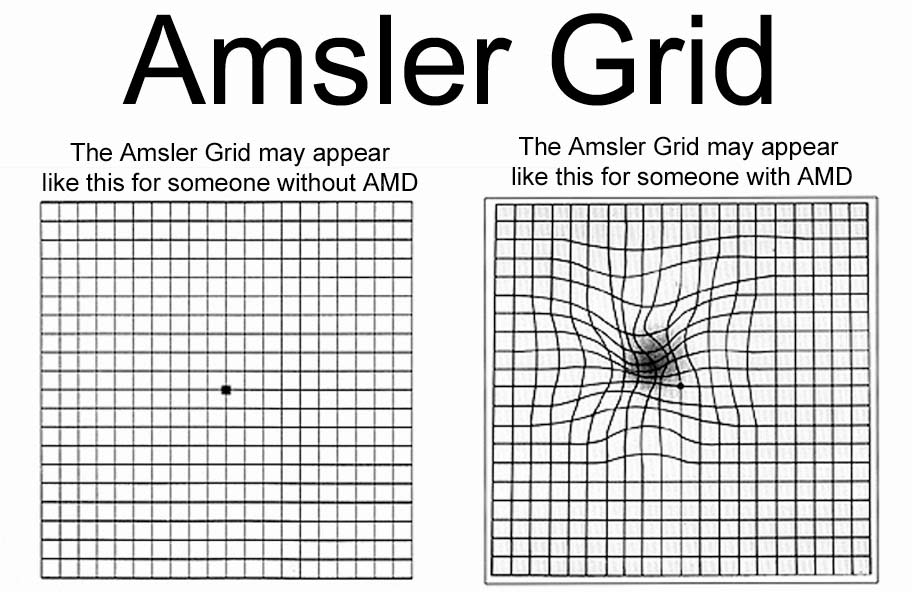
This test monitors dry age-related Macular Degeneration (MD) for progression to wet
AMsler test
This ocular emergency presents with severe eye pain, ciliary flush, decreased acuity, and "cloudy vision", and "halo" around lights at night. A risk factor is prolonged periods of darkness (ie: movie theater). Refer to ophthalmology only if pt can be seen within one hour...otherwise refer to ED
Acute Angle Closure Glaucoma - due to elevated IOP, initially causing peripheral visual field loss and can lead to central vision loss and ultimately total vision loss.
DDX: conjunctivitis, acute uveitis, and corneal disorders.
Recommend: Annual eye exam with ophthalmology
This type is highly contagious and caused by staphylocococcus aureus. Eye has sticky, yellow/green discharge and eyelids may be stuck together upon waking. Spread by direct contact only.
Bacterial Conjunctivitis - treat with ABx eye drops
Can affect one or both eyes
The name for gradual, age-related vision loss
Presbyopia
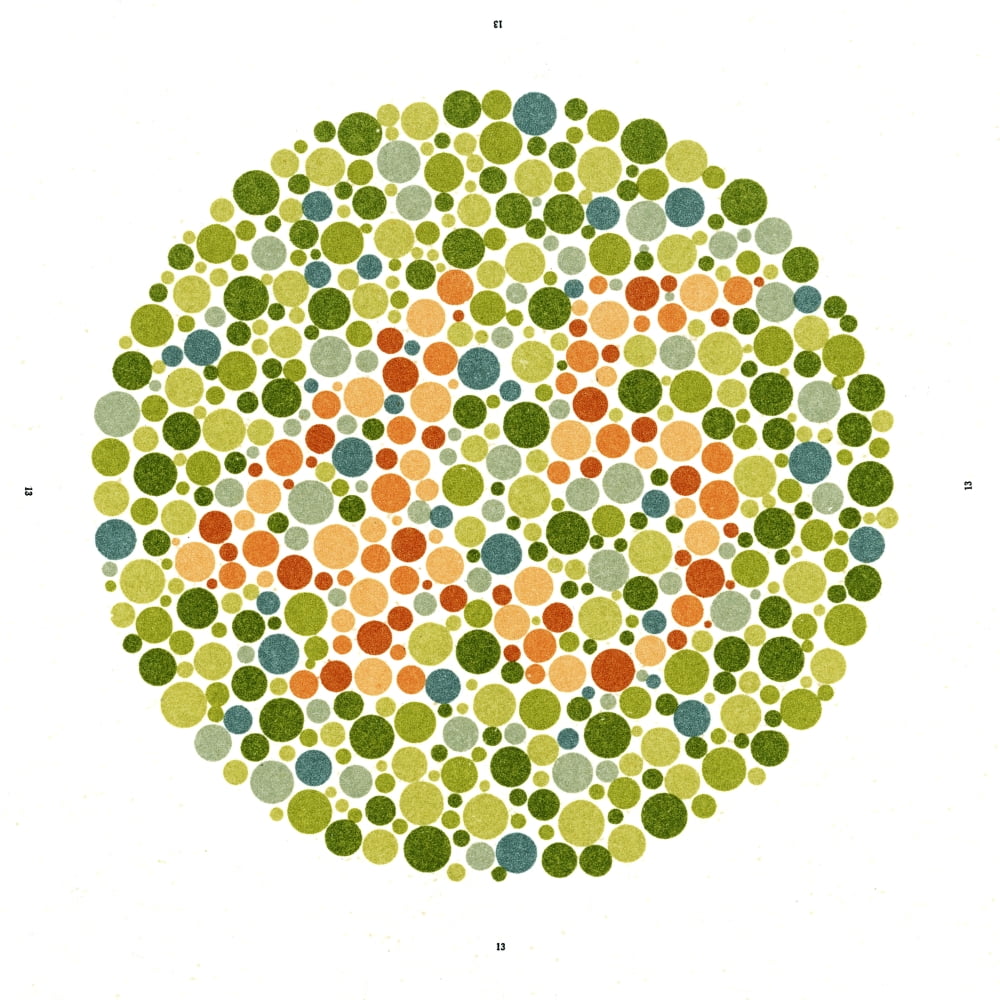
The Ishihara Chart/test is used to detect __________.
Color blindness - the test appropriate for school-age children to adults.
This test is a pocket version of the Snellen chart and is used to test distance acuity
Rosenbach Pocket Vision Screening Card
Stand between 6-14 ft away (see instructions)
This type of emergency is usually not red or painful. However, pt will report sudden onset of floaters (or increase in floaters, looking through a curtain, flashes of light (photopsia). Central vision may be intact or loss if macula is detached.
Retinal Detachment -
Most common RF: Myopia and after cataract surgery
Most common type: Rhegmatogenous (tear or hole in retina and fluid builds up behind)
Spread through hand to eye contact, _(1)_______ conjunctivitis is known as the "pink eye". It's highly contagious, typically caused by _(2)_______ and only requires supportive care (cold compress and lubricants)
1. Viral
2. Adenovirus
**Can affect one or both eyes
Fat deposits on the in the edge of the cornea.
Arcus Senilis - doesn't affect vision, nor does it require treatment.

When arcus senilis occurs in older adults, it isn't related to high cholesterol. However, sometimes occurs in younger people who have severe cases of high cholesterol and high triglycerides passed down through families (familial hyperlipidemia)- typically occurs before age 45 and is associated with an increased risk of heart disease.
The Snellen Chart test CN II by measuring __________
Distance vision / acuity;
Assesses CN II – Optic Nerve; Abnormal if a two-life difference b/w each eye or fewer than 4 of 6 correct. Legally blind – 20/200 or less corrected
THE NEXT 3 question (300, 400 and 500 QUESTIONS) ARE EYE CONDITIONS...
This condition can cause painless vision loss due to inflammation in the arteries.
Giant Cell Arteritis
Signs/Symptoms: flu-like sx, (severe)h/a, fatigue, fever, blurred vision, diplopia, scalp tenderness, jaw ischemia (cramps when chewing), stiffness/pain in neck/ hips or arms, unexplained wt. loss. Most common in older adult (~ 70 yr. old); women twice as likely than men. Co-exist with Polymyalgia Rheumatica is common
DX: Elevated ESR and CRP; thrombocytosis (elevated PLT), elevated Alkaline phospotase. Gold standard: Temporal Arterial Bx.
Treatments: steroids most common – stabilizes vision loss, but still may have some permanent vision loss. New medication: tocilizumab (brand: Actemra; Immunosuppressive drug used in mod-severe RA, other arthritis type illness and GCA).
Contact lens users
S/S: severe pain, foreign body sensation, tearing and photophobia.
DX: Look for whitish lesion on cornea using penlight or slit lamp and fluorescein dye test
__________ Conjunctivitis is accompanied by nasal congestion, sneezing, eyelid swelling, and sensitivity to light. Both eyes are affected and it is NOT contagious.
Allergic
The cranial nerve responsible for visual acuity (#/name)
CN II - Optic Nerve
This test looks for blind spots (aka scotoma) and peripheral visual field defects
Visual fields of confrontation
Patient presents with a rapid onset of unilateral, dully painful red eye w/ discomfort radiating to the temple and periorbital area, w/ visual changes. The pupil is usually constricted, nonreactive, and irregularly shaped and ciliary flush. A risk factor is autoimmune disease.
Patients presenting with this ______________will typically be referred to ophthalmology and Rheumatology.
Anterior Uveitis -
Labs: HLA-B27, ESR, ANA
DDX: acute angle-closure glaucoma, corneal ulcer and ulcerative keratitis, HSV Keratitis (to name a few).
Treatments: Treat the anterior eye inflammation a/w the condition, but also dx and tx the underling autoimmune disease contributing to the condition. Will need an ophthalmological consultation as well as Rheumatological referral is usually warranted.
This type of emergency may have lid, conjunctival or corneal ulceration...although it is typically characterized by dendritic (branching) corneal ulcer and is typically unilateral. To diagnose use fluorescein stain and exam with blue light.
Herpes simplex keratitis - Simple debridement/ patching; more rapid healing w/ addition of topical antivirals (see Table 7-2 in Current 2021). Topical antiviral agents may cause corneal toxicity after ~ 10-14 days of use; therefore, are not usually used for long-term suppressive therapy
HSK – precipitating factors: may be recurrent, precipitated by fever, excessive exposure to sunlight, immunodeficient.
HZO: RF is HIV. S/S: fever, malaise, h/a, periorbital burning and itching. These sx may precede an eruption by a day or more. Rash is vesicular initially, quickly becomes pustular then crusts. Involvement of tip of nose or lid margin predicts involvement of the eye
treat with high dose antiviral for 7-10 days. Refer to ophthalmology
This condition is the leading cause of blindness in the US. RF include age, smoking, CVD, Caucasian race, etc. There are two types: Dry and Wet
Macular Degeneration
•Two types: Dry (secondary to retinal atrophy) and Wet (secondary to abnormal vascular growth in the subretinal space; probable immune-mediate inflammation). Dx: fundoscopic exam, visual changes can often be detected w/ an Amsler Grid. C/o gradual loss of vision in one or both eyes; scotoma (dark patch in center of visual field) or distorted straight edges. Tx: see Current, 2020; but Dietary supplements may slow progression, stop smoking. No specific Tx for dry age-related MD. Both types benefit from “low vision aids” (rehab). Should be referred urgently to an ophthalmologist.
The following are considered ___________ for eye conditions: autoimmune conditions, contact lens wearers, and anticoagulants.
Risk Factors
This is used to detect foreign bodies in the eye using orange dye, a blue lit, and slit lamp.
Fluorescein Eye stain
This condition is often associated with MS as it is demyelinating inflammation of the optic nerve. Patients may also report Uhthoff's phenomenon (transient worsening vision with increased body temperature)
Optic Neuritis - refer to Neurology
Example presentation: Young adult female w/ new or intermittent loss of vision in one eye alone or accompanied by nystagmus or other abnormal eye movements. Aphasia, paresthesia, abnormal gait, spasticity. Daily fatigue upon awakening that worsens as the day goes on. Heat exacerbates symptoms. Has recurrent episodes.
An infection involving the adipose tissue and muscles of the eye is known as
Orbital cellulitis
Etiology: Occurs more often in children than adults, Bacterial rhinosinusitis (most common), orbital trauma w/ fracture/foreign body, Dacryocystitis, teeth, middle ear, face infection.
Differentiate from preseptal cellulitis
TX: broad spectrum abx and surgery
This eye condition is associated with age and cigarette smoking. Patients may present with: progressed blurred vision, glare (esp in bright light and driving at night).
Cataracts