What is the MOA of beta lactam antibiotics?
They binds to the penicillin binding protein (PBP), resulting in degradation of the cell wall and impaired synthesis of a new one result in permeability to the local environment and bacterial lysis
What is the MOA of aminoglycosides?
Aminoglycosides inhibit bacterial protein synthesis by binding to the ribosome 30S subunit. 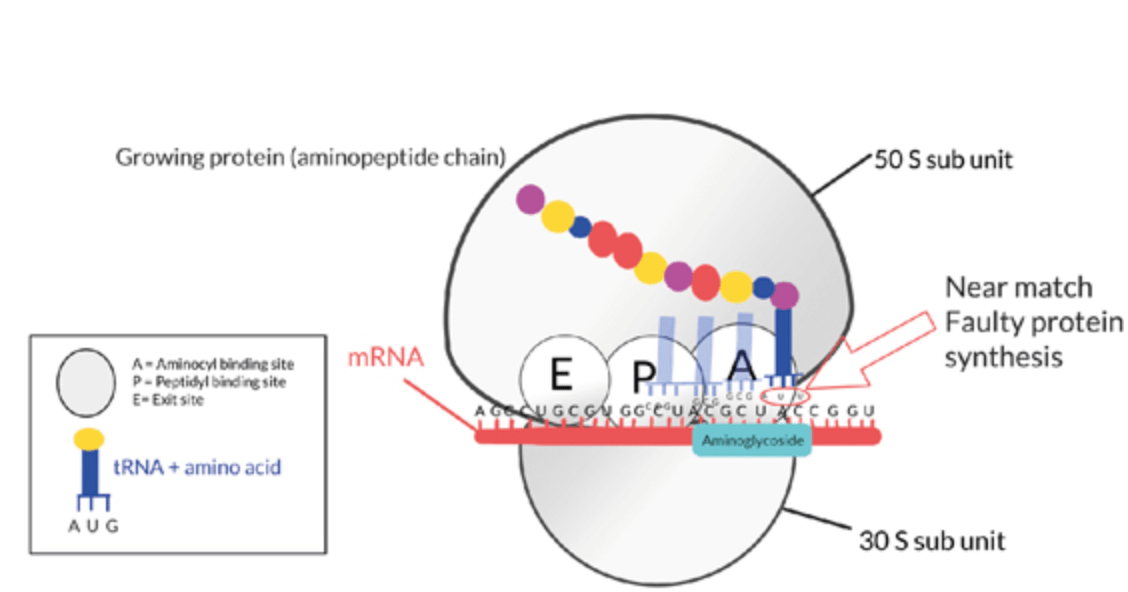
What is the MOA of fluoroquinolones?
All fluoroquinolones exert antimicrobial activity via inhibition of bacterial topoisomerase IV and DNA gyrase (a member of the topoisomerase family). Inhibition of these enzymes prevents normal bacterial DNA synthesis, replication, and division, resulting in bacterial cell death. DNA gyrase catalyzes the negative supercoiling of circular bacterial DNA as well as relaxing positive supercoiling, the latter of which would otherwise interfere with DNA replication. Topoisomerase IV unlinks DNA following DNA replication, facilitating the separation of daughter cells. Inhibition of DNA gyrase is the predominant mechanism for the killing of Gram-negative bacteria, whereas inhibition of topoisomerase IV is primarily responsible for effects on Gram-positive bacteria.
What is the MOA of metronidazole?
Within the bacteria, it gets reduced and is incorporated within the bacterial DNA, causing a loss of helical structure, inhibition of nucleic acid synthesis, and cell death. The nitrous reduction of metronidazole can only be achieved in anaerobic bacteria.
List the anti-Pseudomonal antibiotics.
Antipseudomonal penicillins (ticarcillin and piperacillin), ceftazadime, +/- aztreonam, aminoglycosides, fluoroquinolones, third generation cephalosporins (cefepime, cefpirome and cefquinome)
What are the mechanism of methicillin resistance Staph and expression of this confers resistance to what antimicrobials?
Insertion of the mecA gene, which encodes a mutation in the PBP2a. Expression of this gene will make the organism resistant to the entire class of β-lactam antimicrobials except fifth-generation cephalosporins
What are the three mechanisms of acquired resistance in aminoglycosides and the intrinsic resistance mechanism?
Acquired resistance:enzymatic mutation of the aminoglycoside molecules themselves, target modification with a change in ribosomal 30S subunit structure, and an increase in aminoglycoside efflux out of the bacteria.
Intrinsic resistance: Aminoglycoside uptake requires active electron transport, which is the result of aerobic metabolism. As such, aminoglycosides are ineffective against anaerobic bacteria. Similarly, Gram-positive facultative anaerobes such as Enterococcus faecalis and Enterococcus faecium are resistant due to poor cellular uptake and the presence of AME.
What antibacterial spectrum do fluoroquinolones cover? 7 bacteria required for credit.
Enterobacteriaceae (Escherichia coli, Klebsiella), Pasteurella spp., Bordetella spp., Salmonella, and Campylobacter spp. Pseudomonas aeruginosa is variably susceptible to different fluoroquinolones, and resistance to fluoroquinolones can develop during the course of treatment.6 Isolates of P. aeruginosa appear to have greater susceptibility to marbofloxacin than enrofloxacin.7 Susceptible Gram-positive organisms include Staphylococcus spp. and Neisseria spp., while Streptococcus spp. are frequently resistant.Intracellular pathogens potentially susceptible to fluoroquinolones include Mycoplasma spp., Chlamydophila spp., Brucella canis, and certain mycobacteria. Of note, tick-borne rickettsial and rickettsia-like infections are variably susceptible to fluoroquinolones, and many are resistant.
What four antibiotics inhibit the 50 s ribosome as their mechanism of action?
Chloramphenicol, clindamycin, macrolides (erythromycin, azithromycin), linezolid
What are the anti-mycoplasma antibiotics?
Tetracyclines, clindamycin, chloramphenicol, aminoglycosides (?) and fluoroquinolones
What are the 4 mechanisms of resistance of beta lactams?
Resistance to the β-lactam class can be due to alterations in the PBPs of a bacteria, development of antimicrobial efflux pumps, changes to porins in the bacterial cell wall, or inactivation by β-lactamases.
Penicillinases, AmpC-type cephalosporinases, extended spectrum β-lactamases (ESBLs), and carbapenemases.
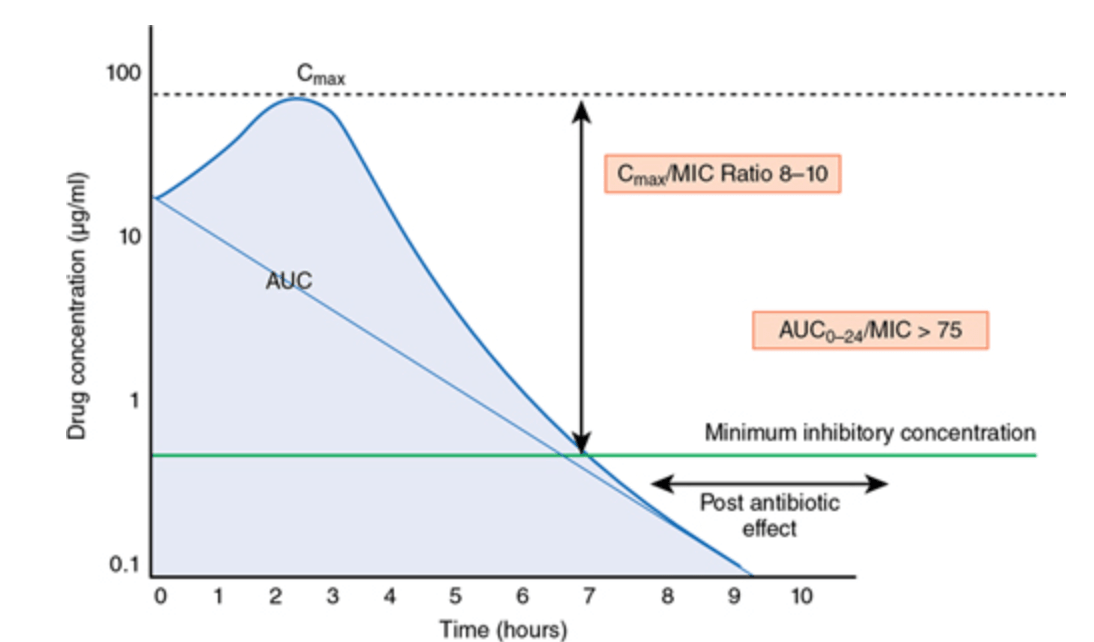
What are the PK/PD goals for maximal antibioic effects of aminoglycosides?
Maximum (peak) drug plasma concentration (CMax) over the minimum inhibitory concentration (MIC) of 8 to 10 or the area under the curve (AUC) over MIC ratio >75.16 Increasing the ratio Cmax/ MIC >10 does not significantly increase bactericidal activity
What are mechanisms of resistance to fluoroquinolones?
1. Increased efflux and 2. Alterations to the antimicrobial targets DNA gyrase and topoisomerase IV. Specifically, point mutations for the bacterial genes encoding the gyrA subunit of DNA gyrase and the parC subunit of topoisomerase result in reduced drug affinity for these complexes.
Plasmid-mediated fluoroquinolone resistance has been documented, and plasmids may confer resistance to multiple classes of antimicrobials, resulting in multidrug resistant organisms
What is the MOA of TMS?
Sulfonamide and trimethoprim work on different steps of bacterial folic acid production. Sulfonamide is a competitive analog to P aminobenzoic acid (PABA). Trimethoprim inhibits folic acid reduction (via dihydrofolate reductase) lower down the folic acid production pathway. Each drug used individually is bacteriostatic. The combination of sulfonamide and trimethoprim results in a bactericidal and time-dependent drug.
What antibiotics are time dependent vs. concentration dependent? List 3 examples of each.
Time dependent:
Beta lactams, linezolid (oxazolidinones), TMS (sulfas), tetracyclines, cindamycin (lincosamides),
Concentration dependent
Daptomycin (lipopeptides), metronidazole (nitroimidazole), fluoroquinolines, aminoglycosides
List three beta lactamase inhibitors and their MOA.
The three β-lactamase inhibitors clavulanic acid, sulbactam, and tazobactam are weak β-lactam antimicrobials each possessing the β-lactam ring.
They irreversibly bind to β-lactamases, and when administered with a β-lactam antimicrobial (e.g., ampicillin/sulbactam, amoxicillin/clavulanate, or piperacillin/tazobactam), the β-lactam can then bind to the bacterial PBP resulting in cell death
What are three adverse effects of aminoglycosides?
Nephrotoxicity, ototoxicity and NMB
What adverse events have been reported secondary to fluoroquinolone use?
GI; neurologic (seizures, tremors, and abnormal electroencephalographic finding)s; cartilage defects in juvenile animals, and irreversible blindness in cats
Competitively inhibit binding of γ-aminobutyric acid, which may lower the seizure threshold in patients with idiopathic epilepsy, and thus should be avoided or used with extreme caution in patients with seizure disorders.
The injectable form of enrofloxacin has an alkaline pH (pH = 11), and subcutaneous administration has been associated with localized reactions and skin necrosis. The injectable formulation is labeled for intramuscular use, and subcutaneous use should be avoided.
Additional adverse effects in people: peripheral neuropathy, delirium, tendinitis/acute tendon rupture, altered glucose homeostasis, QT prolongation, phototoxicity, hepatotoxicity, interstitial nephritis, hemolytic uremic syndrome, crystalluria, and Clostridioides difficile infection.
Rapid intravenous administration may result in histamine release in dogs. Higher than recommended intravenous doses of marbofloxacin (12 mg/kg) resulted in cardiovascular signs including hypotension, decreased heart rate, and prolongation of the QT interval in healthy anesthetized dogs. There is debate as to whether rapid intravenous enrofloxacin may also decrease seizure threshold in dogs, but this has not been studied or formally reported.
The use of fluoroquinolones in patients with necrotizing fasciitis is potentially detrimental. Rare reports have documented that fluoroquinolones can induce activation of a latent bacteriophage within exotoxin-producing Streptococcus spp. (i.e., S. canis) isolated from a dog with necrotizing fasciitis. Bacteriophage activation can result in rapid bacterial cell lysis, release of a bacteriophage encoded streptococcal superantigen, and the potential sequelae of toxic shock syndrome.
What is the MOA of vancomycin?
Vancomycin prevents the formation of peptidoglycan in Gram-positive pathogens.
What antibiotics are bacteriostatic?
Choramphenicol, clindamycin (vs. cidal), tetracyclines, and linezolid
What are the side effects of beta lactams?
Type 1 HS --> urticaria to acute anaphylaxis. The frequency is unknown in animals, in people, allergic reactions occur in 0.7%–10% receiving penicillin, with acute anaphylactic reactions occurring in 0.01%–0.05%.
Type 2 HS reactions: hemolytic anemia, thrombocytopenia, and neutropenia have reported.
Type 3 and 4 HS reactions are also possible with unknown incidences, with the type 4 HS reactions usually manifesting as cutaneous disease. Nausea, vomiting, and diarrhea with PO administration. If they are administered in high doses, resulting seizures and other neurologic diseases are possible. These are more likely if brain disease is already present.
What is the antibacterial spectrum of aminoglycosides? List 7 bacteria for credit.
Escherichia coli, Klebsiella pneumoniae, Enterobacter cloacae, and Proteus spp, Yersinia pestis, tularemia (Francisella tularensis), Staphylococcus aureus and Staphylococcus pseudointermedius, MRSP/MRSA, Pseudomonas aeruiginosa, Acinetobacter baumanii.
What is the Vd of fluoroquinolones and what tissue penetration is achieved with this class of drugs?
Fluoroquinolones have a relatively high volume of distribution (Vd) and distribute into tissues and the intracellular space soon after administration. Concentrations in kidney, lung, and prostate tissue, as well as urine, bile, macrophages and neutrophils often exceed that of serum. They are lipophilic molecules that exhibit variable protein binding within the class, ranging from low to moderate (18%–35%).
What are adverse effects of TMS? List 5 for credit.
Dogs have a decreased ability to acetylate sulfonamide, creating allergenic, immunogenic, and toxic metabolites. Doberman Pinschers, Samoyeds, and Miniature Schnauzers are thought to be more sensitive to TMS than other breeds. Side effects include hypersensitivity reactions such as fever, polyarthropathies, pancreatitis, hepatitis, glomerulonephritis, anemia, immune-mediated thrombocytopenia, and mucosal skin lesions, none of which are dose-dependent. Keratoconjunctivitis sicca (KCS) is the most common side effect due to the direct cytotoxic effect of sulfonamides on the lacrimal gland. Additionally, a reversible decrease in thyroid hormones has been reported in dogs.
What antibiotics are exhibit a post antibiotic effect (PAE)?
Aminoglycosides, fluoroquinolines, clindamycin, macrolides, glycopeptides, linezolid, carbapenams