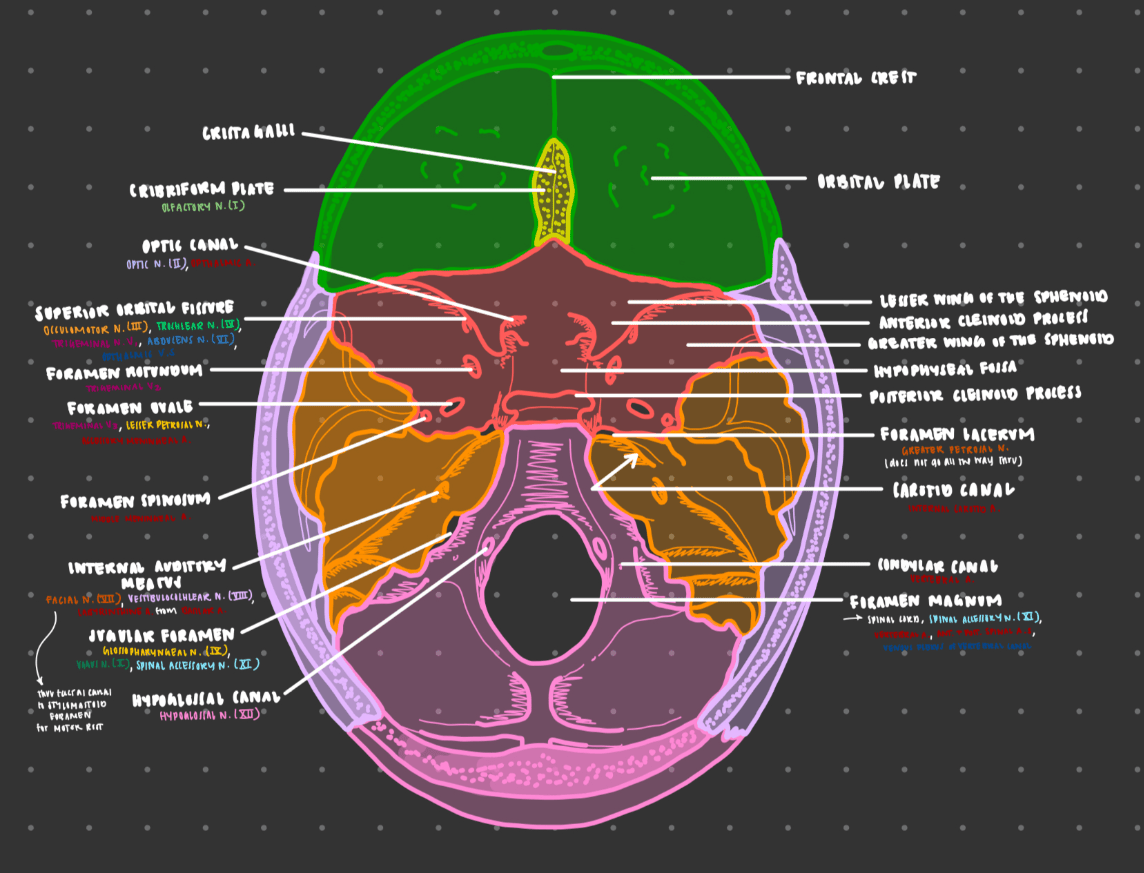
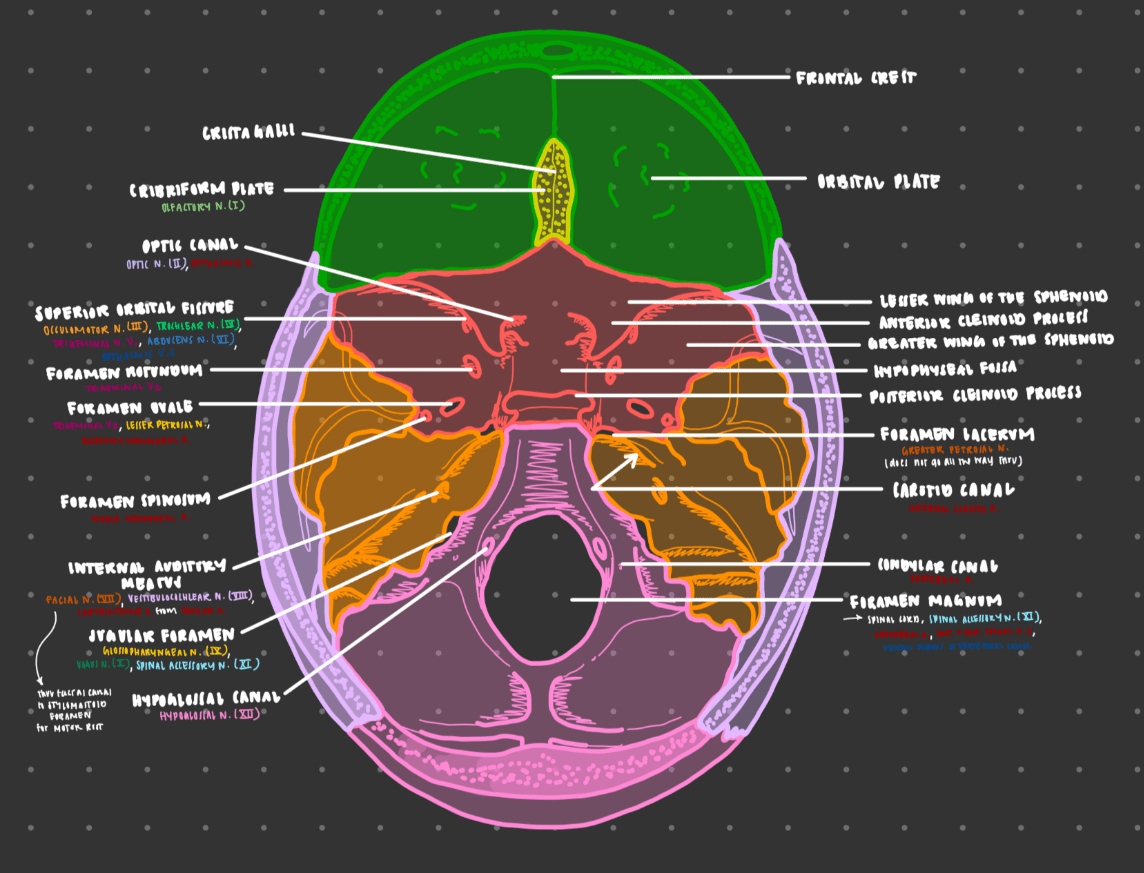
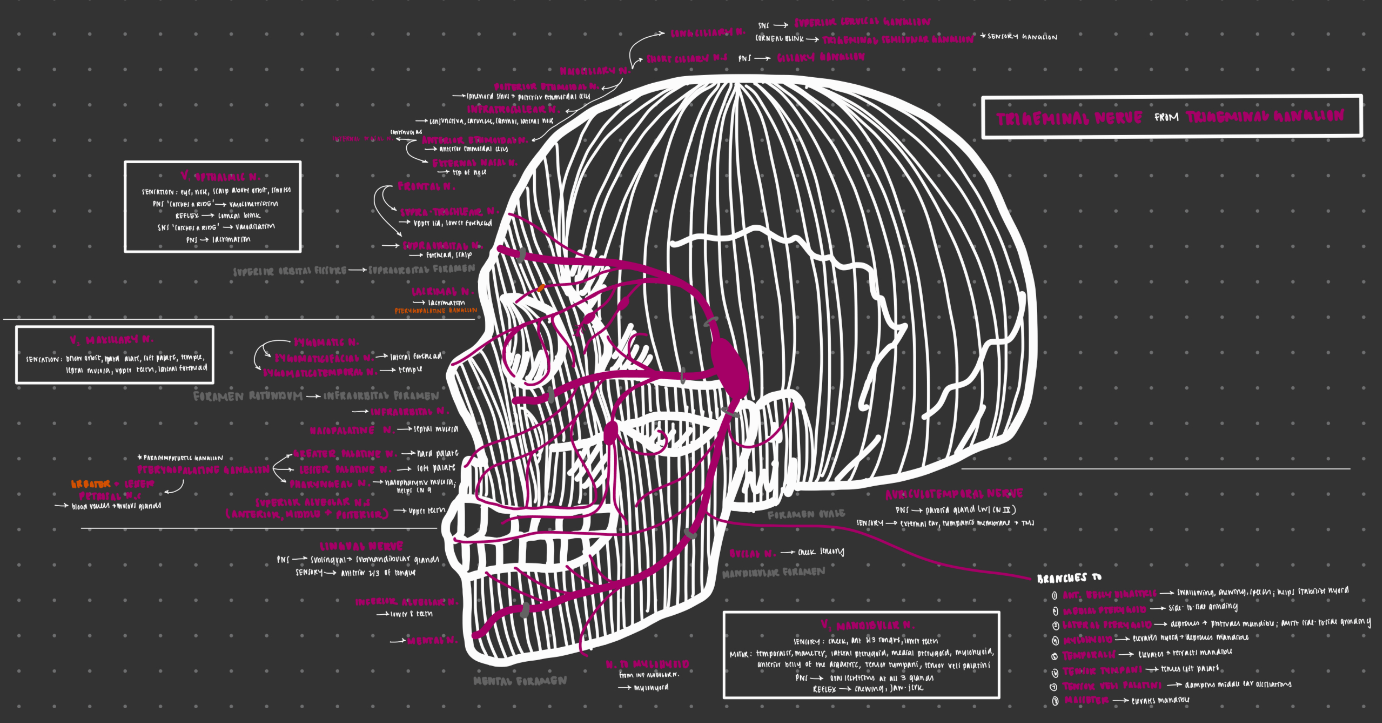
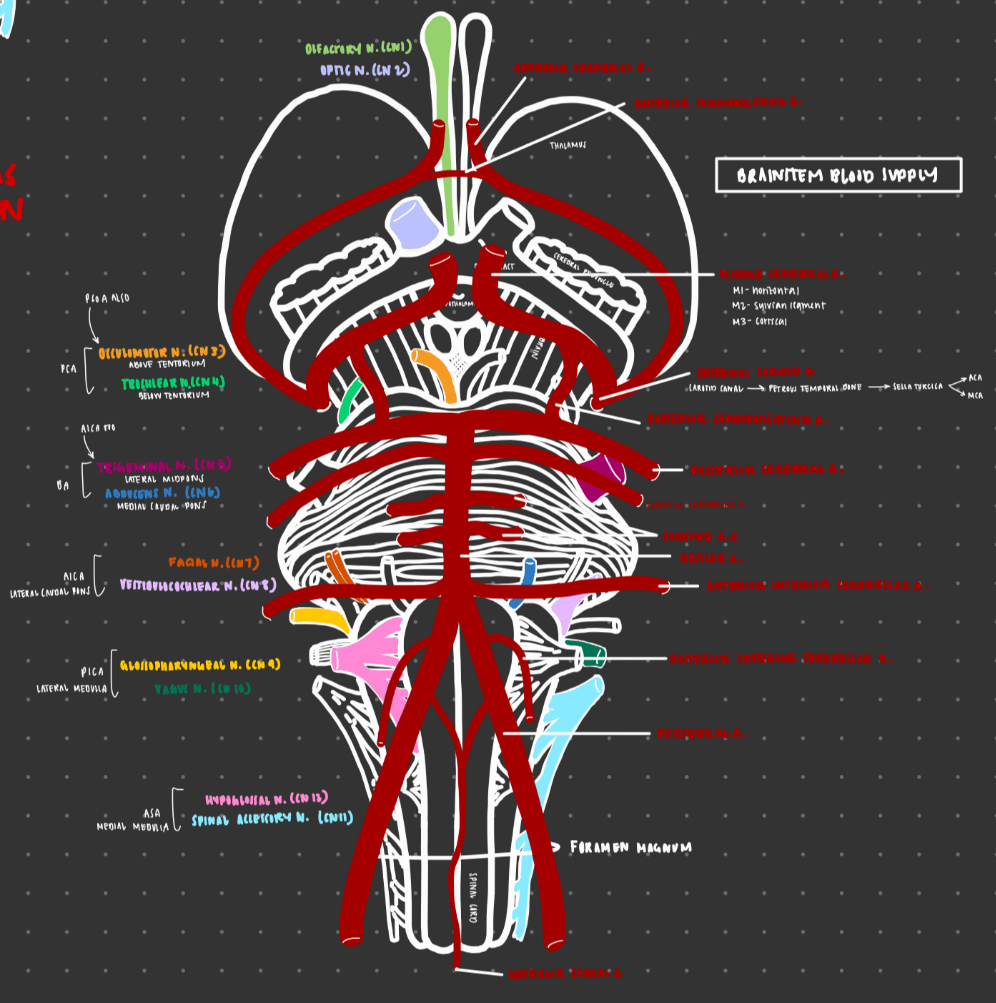
Which 4 nerves travel through the superior orbital fissure?
1) occulomotor nerve (CN III)
2) trochlear nerve (CN IV)
3) V1 of trigeminal (CN V/V1)
4) Abducens nerve (CN VI)
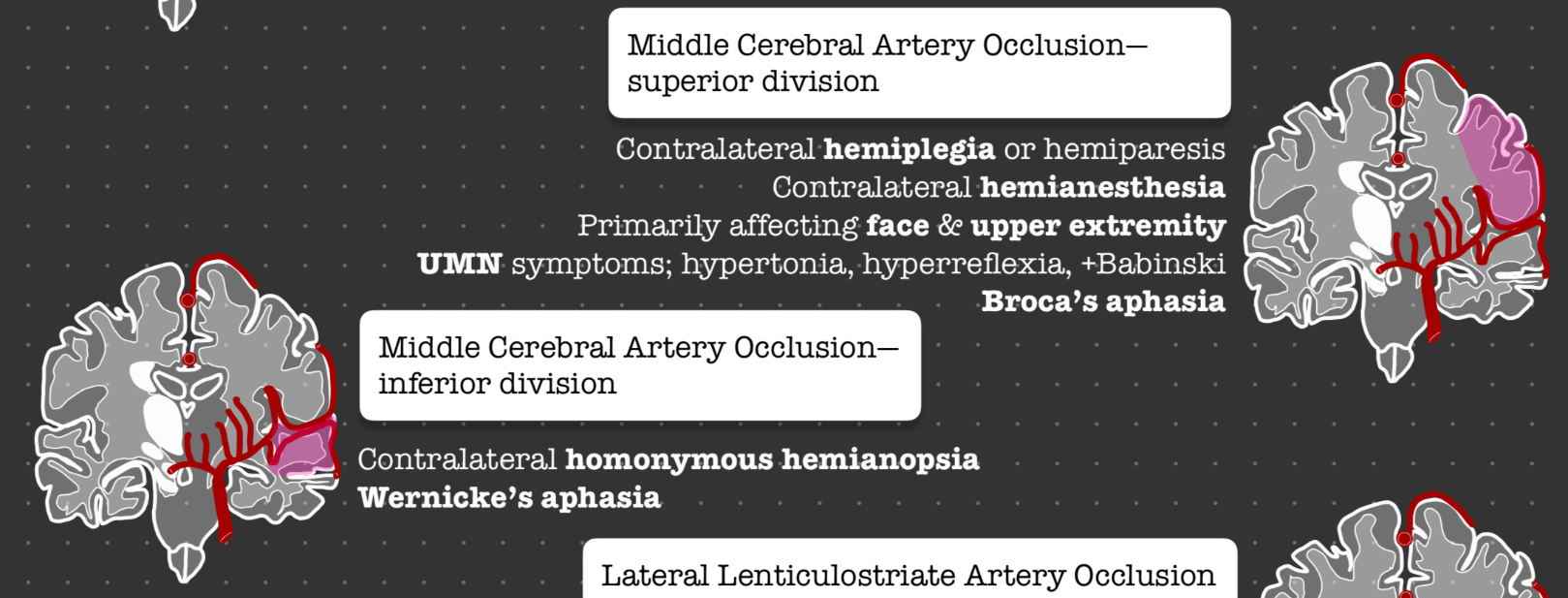
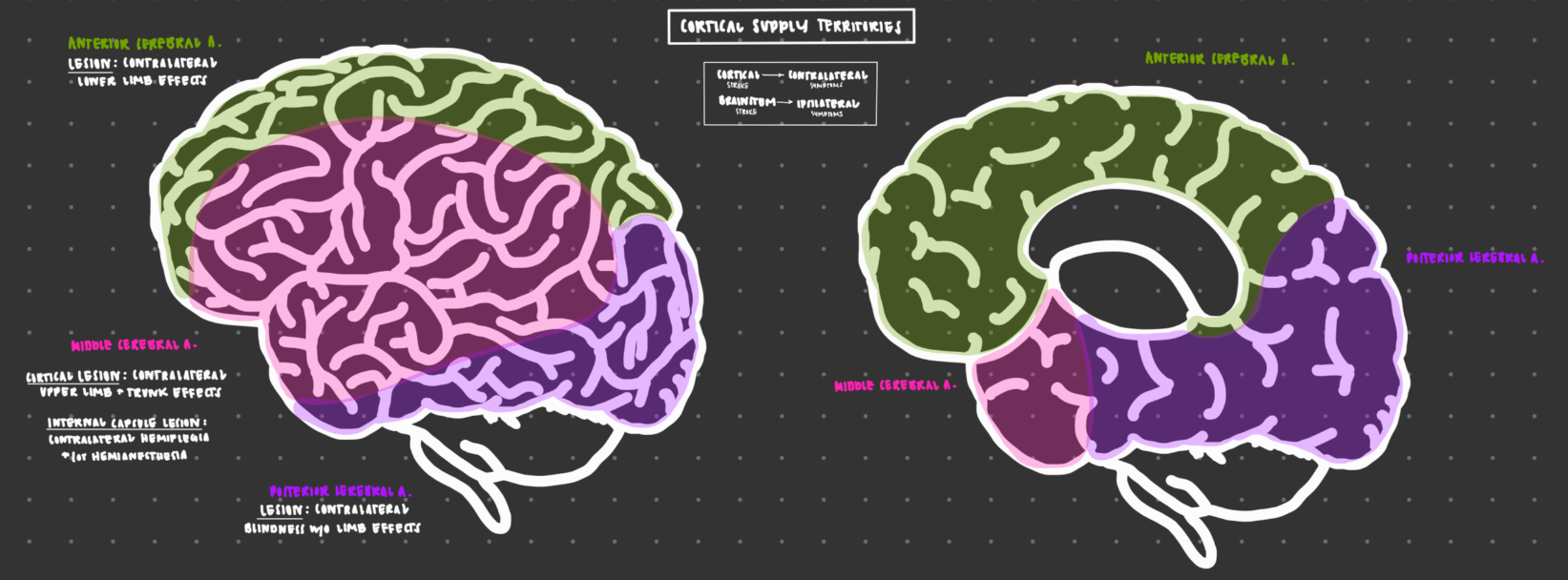
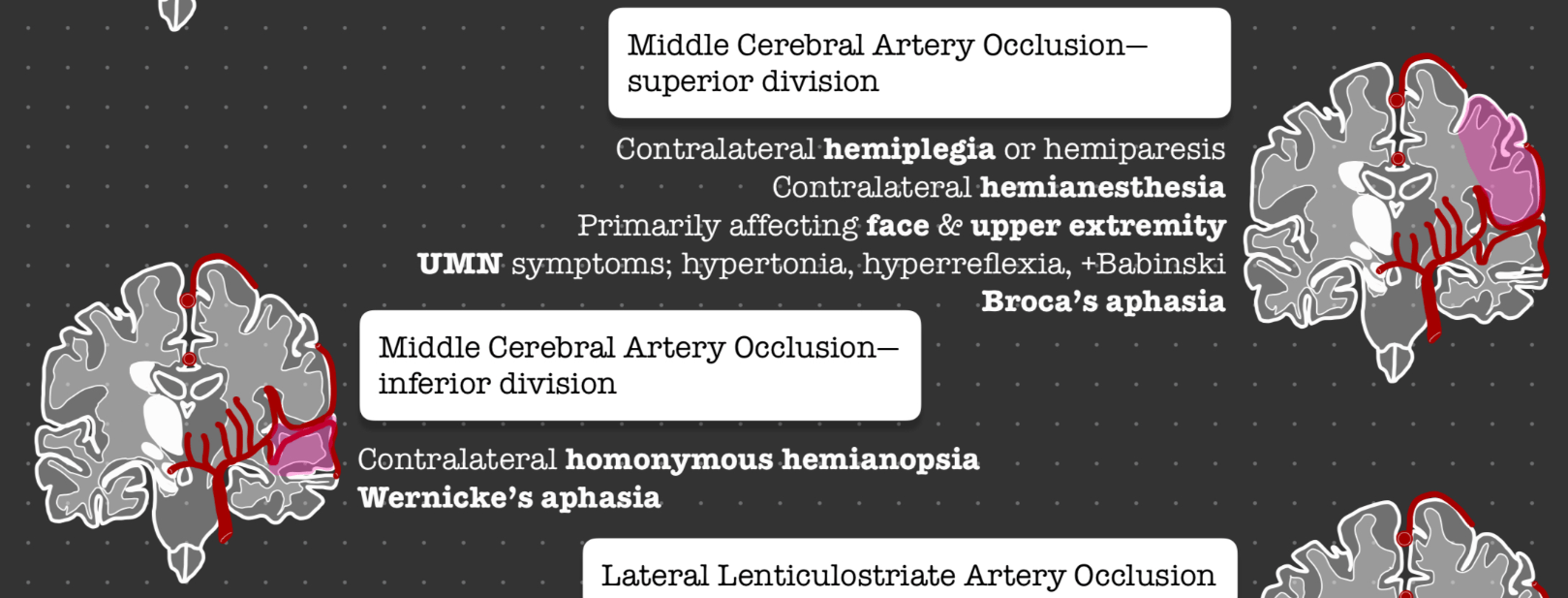
Patient presents with LUE and L facial numbness and weakness, as well as slurred speech. Which artery is impacted?
superior division R MCA
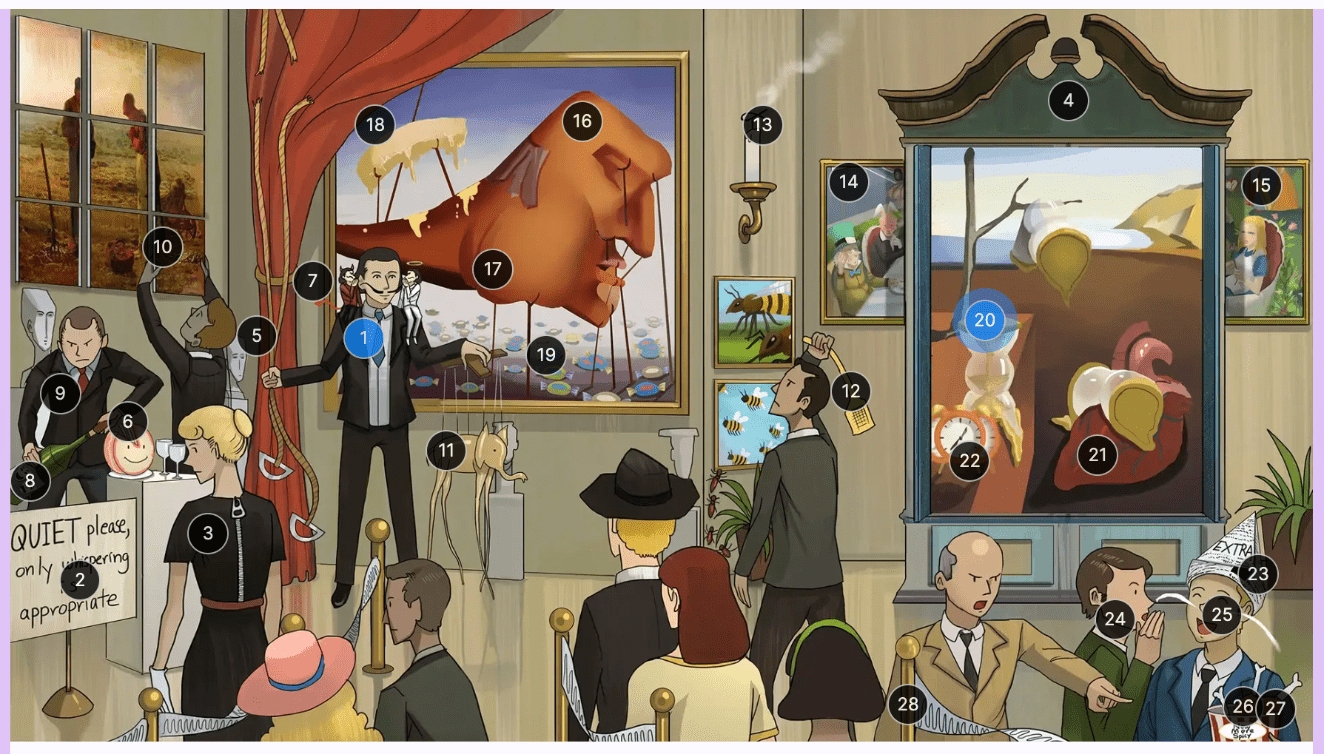
Which defense mechanism is most characteristic of patients with borderline personality disorder?
Splitting is most characteristic of patients with borderline personality disorder. Splitting is a defense mechanism where the patient believes people are all good or all bad, marked by both extreme idealization and devaluation. This is identical to dichotomous thinking, however this is a cognitive distortion rather than a coping mechanism.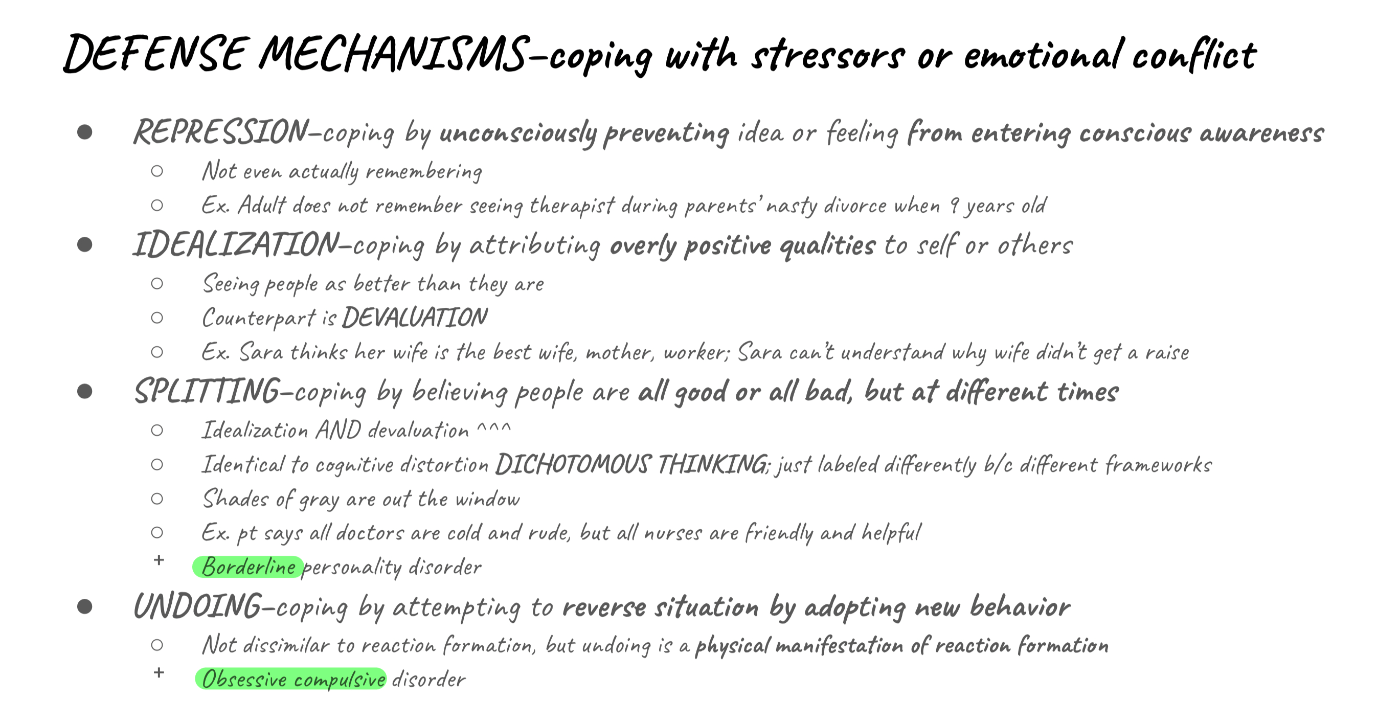
Which finding seen on pathology is associated with HSV-1 viral encephalitis?
Cowdry bodies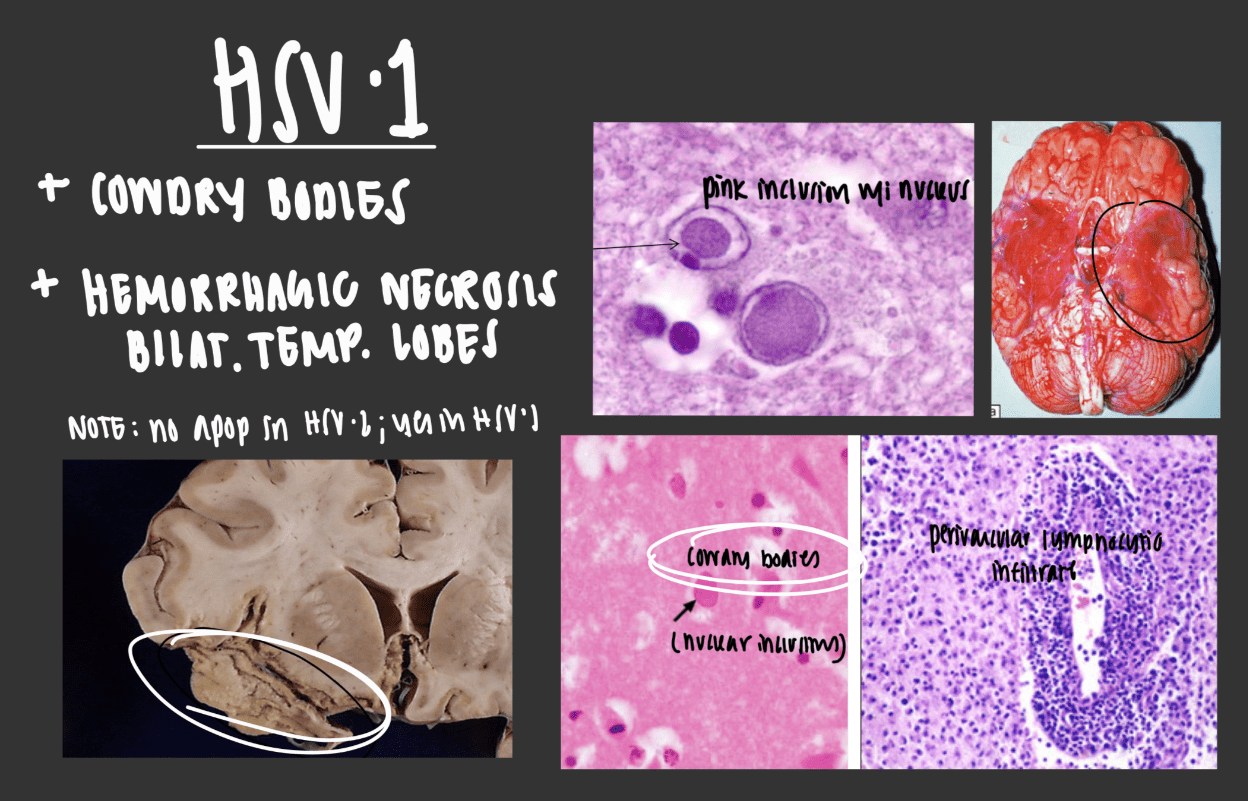
Which antipsychotic is notorious for causing agranulocytosis?
Clozapine
What is the pathway by which the facial nerve travels from the brainstem to the muscles of facial expression?
caudal pons --> internal auditory meatus --> facial canal --> stylomastoid foramen --> muscles of facial expression
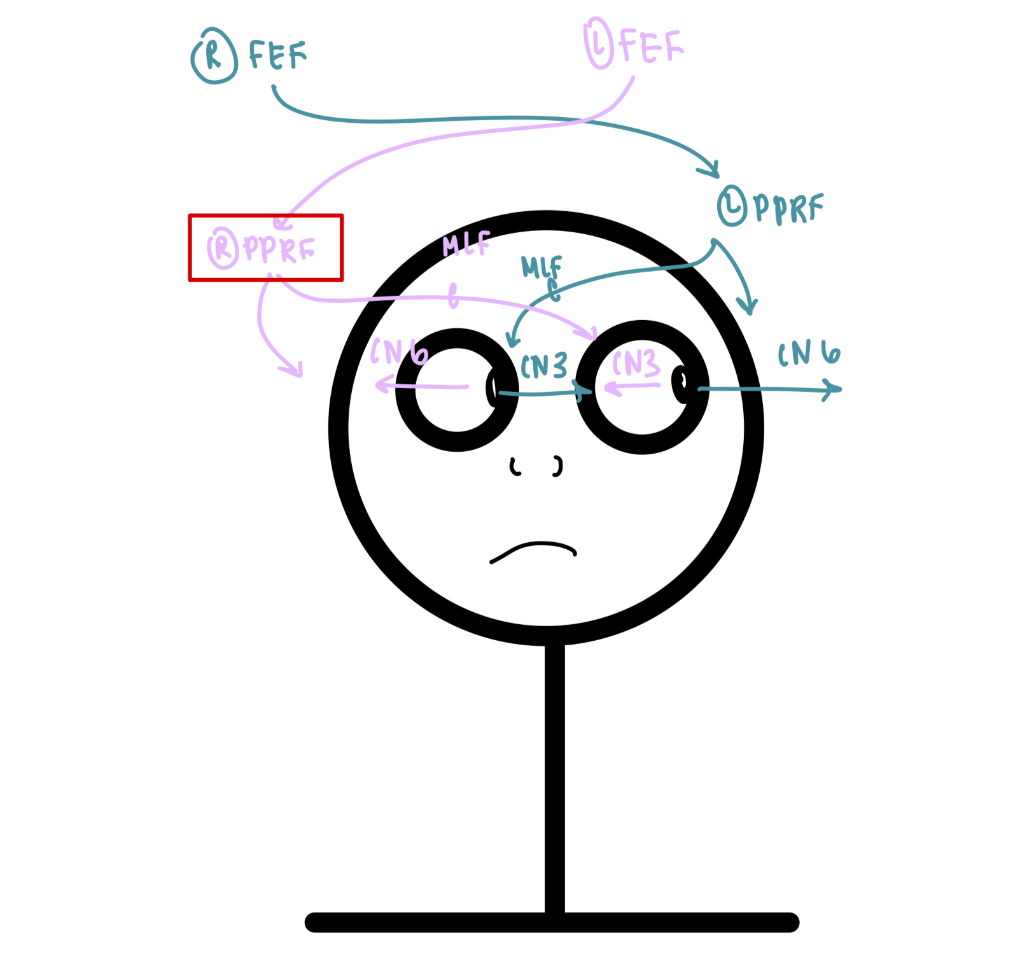
Patient presents for difficulty seeing. Patient has fixed, leftward gaze deviation. Pupillary reflexes are intact, and the remainder of the neurologic exam is normal. Where is the lesion?
What differentiates schizotypal personality disorder from avoidant personality disorder?
Patients with schizotypal personality disorder possess pervasive patterns of social & interpersonal deficits marked by discomfort with and reduced capacity for close relationships.
Patients with avoidant personality disorder, on the other hand, exhibit pervasive patterns of social inhibition secondary to feelings of inadequacy and hypersensitivity to negative evaluation.
In summary, both isolate themselves, but only one likes it that way (schizotypal).
Which set of clinical findings are characteristic of transtentorial (uncal) herniation syndrome?
Uncal herniation is often characterized as having false localization. The medial temporal lobe compresses CN3, leading to ipsilateral blown pupil, ipsilateral CN3 palsy, contralateral weakness, and subsequently ipsilateral weakness if pressure compresses contralateral midbrain against Kernohan's notch.

What are the mechanisms of action of the two most common treatments for Alzheimer disease?
Acetylcholinesterase inhibitors (donepezil, rivastigmine, galantamine)
NMDA antagonists (memantine)
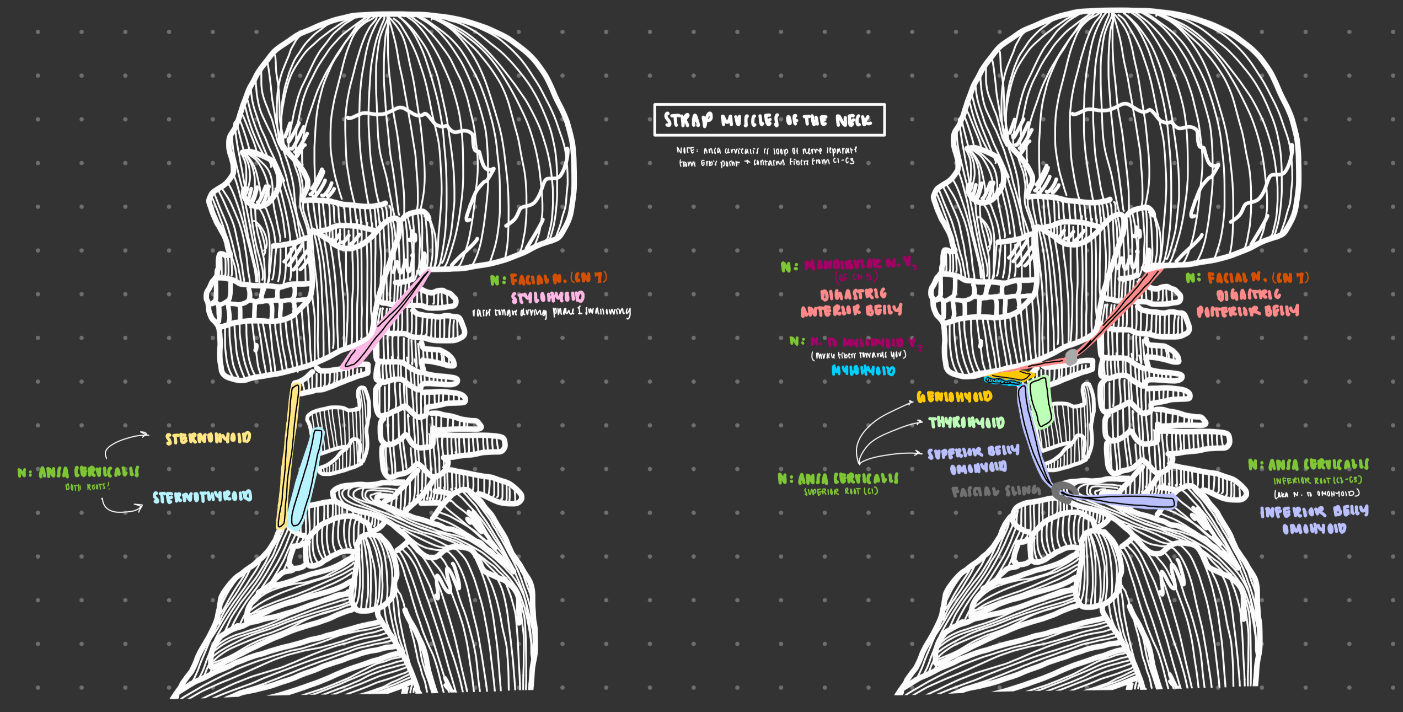
What are the roots of the nerve that supplies both the sternohyoid and the sternothyroid muscles?
Ansa cervicalis contains fibers from C1-C3 and all supply sternohyoid and sternothyroid.
The superior root of ansa cervicalis contains fibers from C1 and supplies geniohyoid, thyrohyoid, and the superior belly of the omohyoid.
The inferior root of ansa cervicalis contains fibers from C2-C3 and is iften called the nerve to omohyoid. This supplies only the inferior belly of omohyoid.
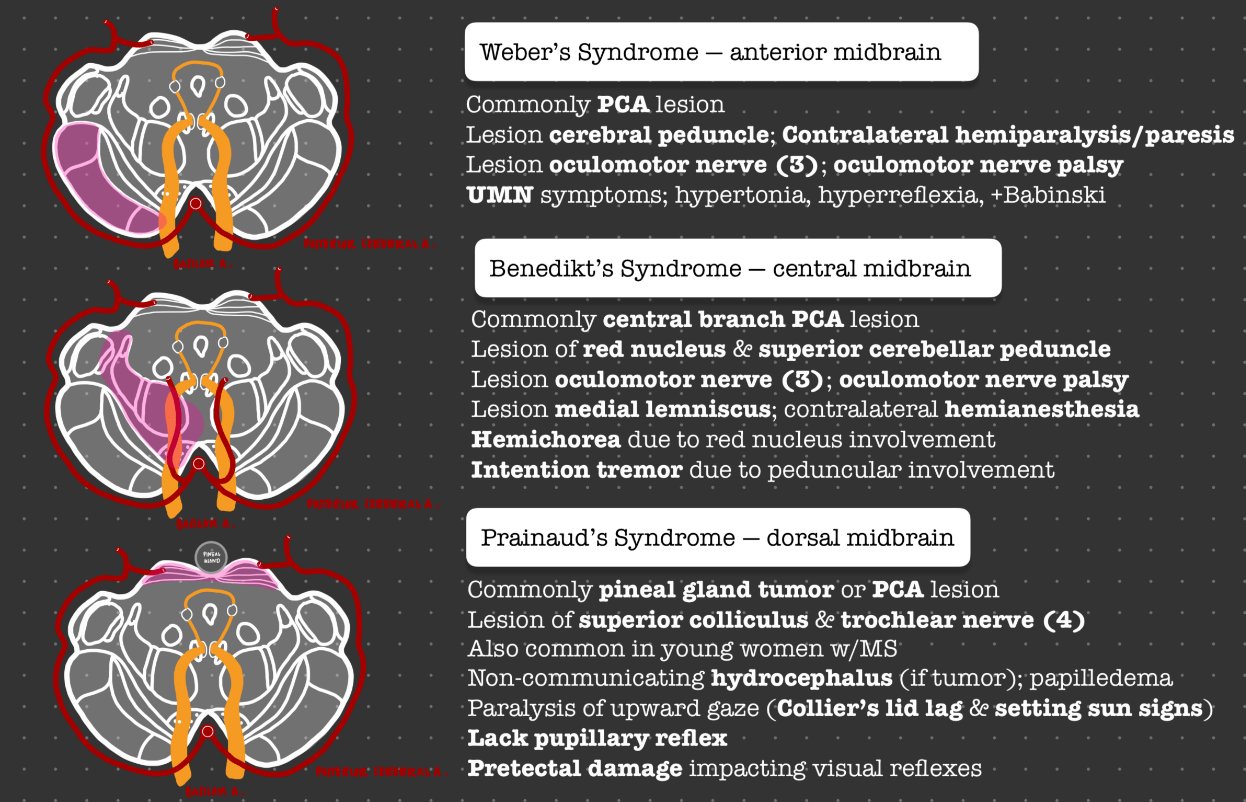
A young child presents to the ED due to AMS and inability to look upwards. A CT scan is obtained, and it is determined that patient has signs of increased ICP, including enlarged ventricles and posterior scleral flattening. Patient also lacks pupillary reflexes. What lesion is characteristic of this condition?
This is a pineal gland tumor causing Prainaud syndrome, or lesion of dorsal midbrain.
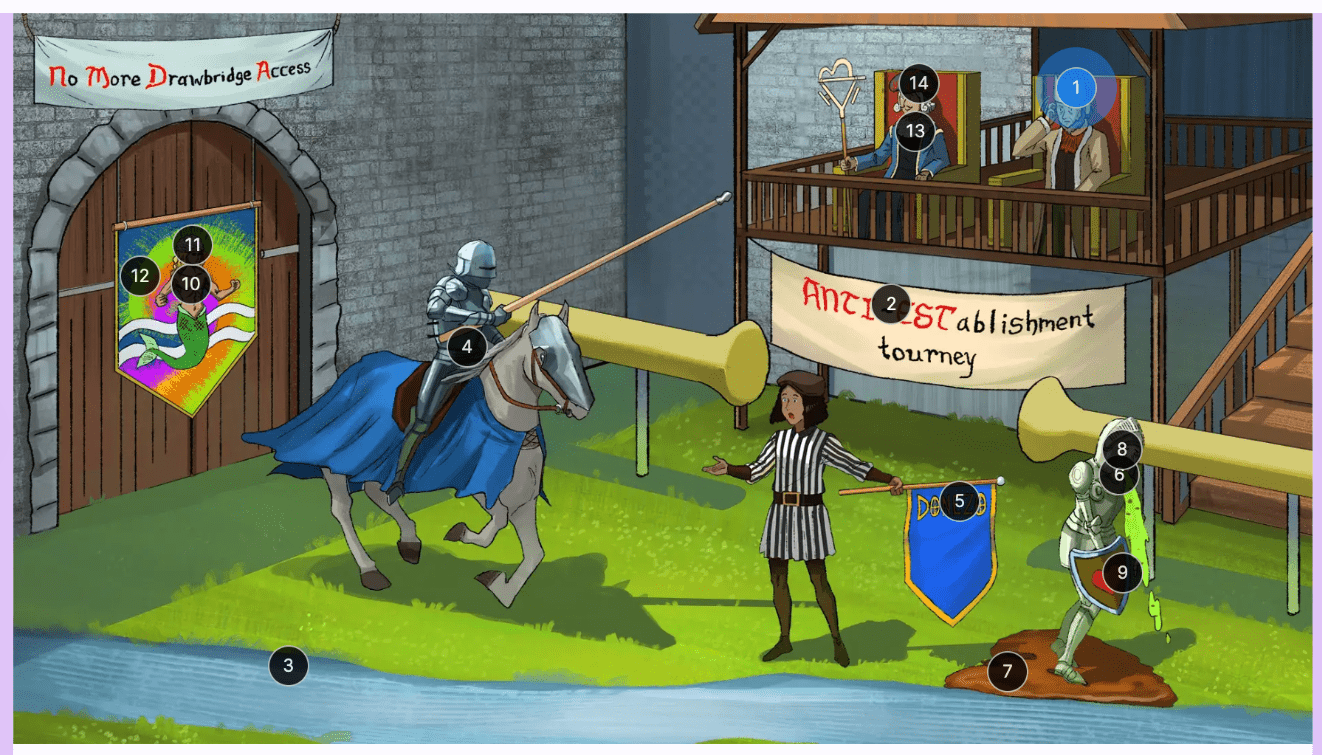
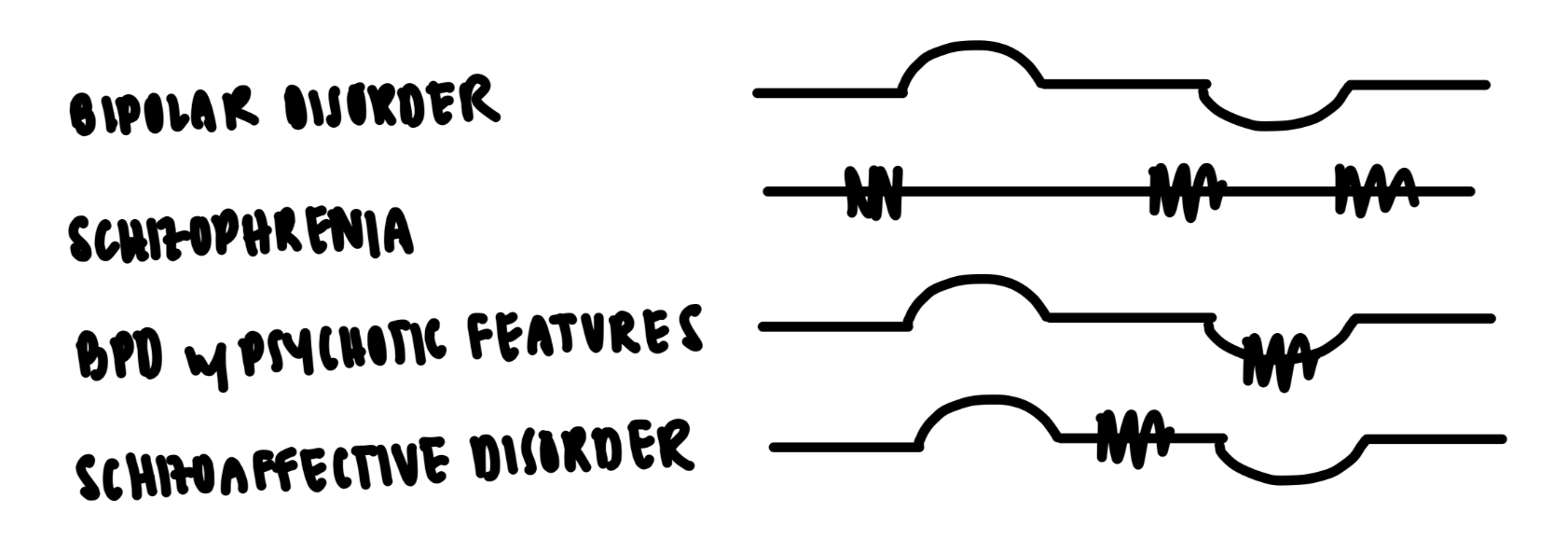
Please draw Griffith's lines for the following:
bipolar disorder
schizophrenia
bipolar disorder with psychotic features
schizoaffective disorder
One CNS tumor grows particularly quickly in pregnancy. What is the gene/mutation and histologic finding are associated with this lesion?
Meningiomas often have progesterone receptors and grow rapidly in pregnancy. These tumors characteristically have loss of c22q encoding NF2 protein. They have psammoma bodies on histology.
In which mental health ailment are benzodiazepines contraindicated? Why?
In which mental health ailment are SSRIs contraindicated? Why?
Benzos are contraindicated in persons with PTSD due to increased risk of suicidality.
SSRIs are contraindicated in patients with bipolar disorder due to risk of precipitating mania.
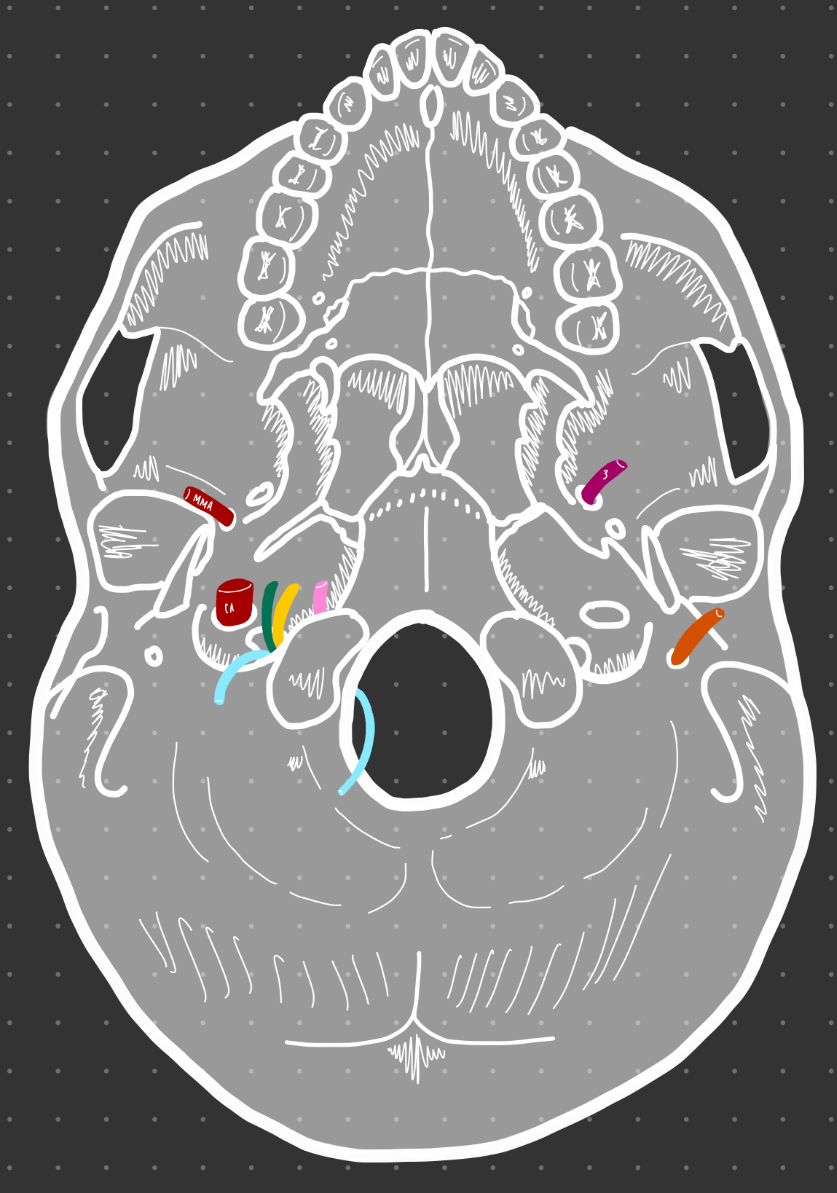
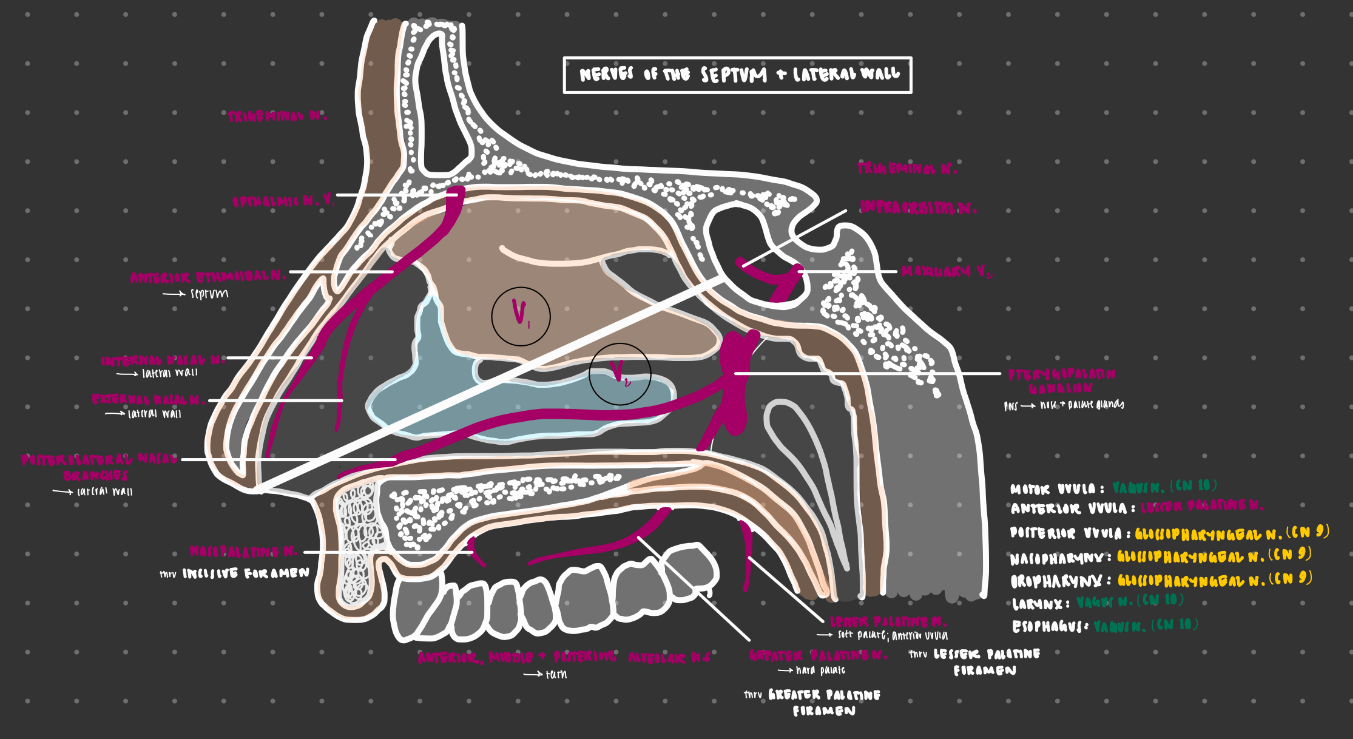
What are all the muscles innervated by the nerve that travels through foramen ovale?
V3 travels through foramen ovale
1) temporalis
2) masseter
3) lateral pterygoid
4) medial pterygoid
5) mylohyoid
6) anterior belly of digastric
7) tensor tympani
8) tensor veli palatini
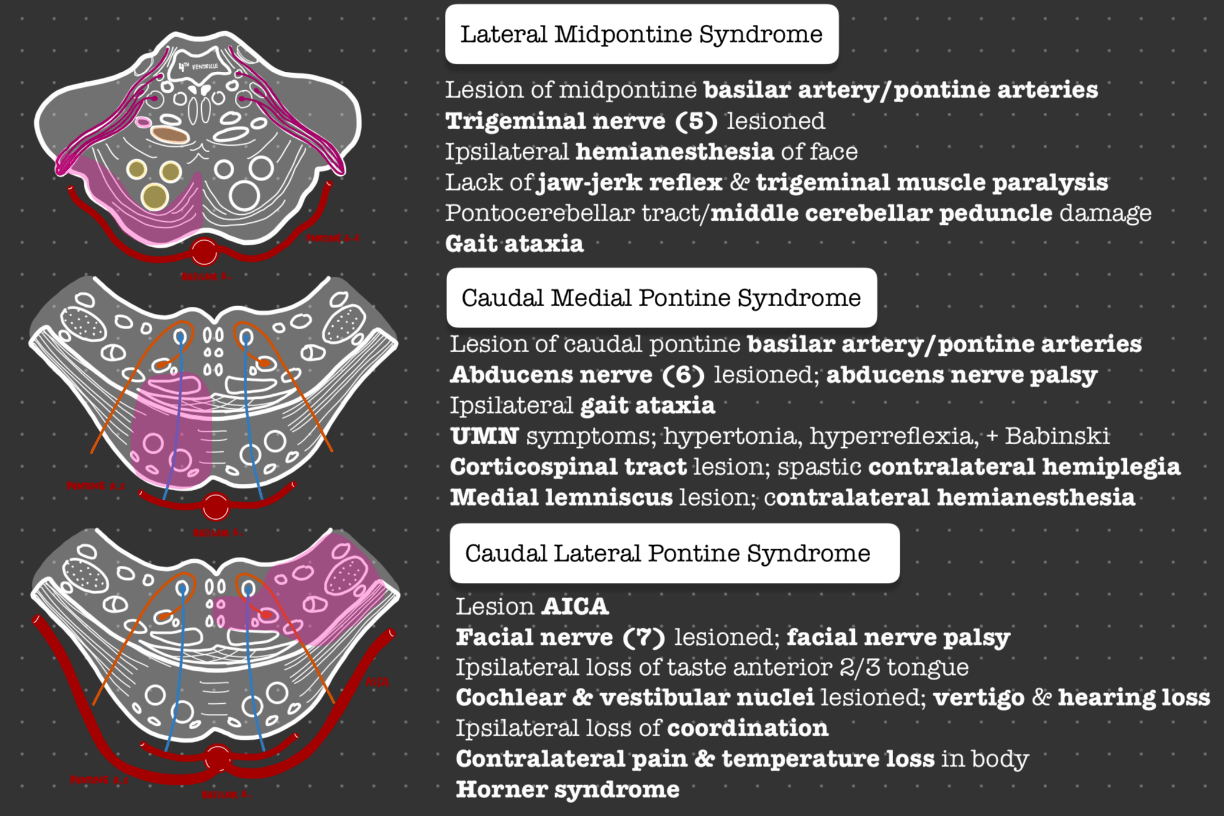
Patient presents to the ED with ataxia, left-sided facial weakness, and diminished ability to taste her favorite sweet little treat (devastating). Upon further examination, patient also has left-sided hearing loss and impaired finger-to-nose testing on the left. Her left pupil is constricted, and ptosis is present on the left as well. Where is the lesion?
AICA. This is caudal lateral pontine syndrome, aka Marie Foix Alajouanine syndrome.
What are the diagnostic criteria for schizophrenia?
Must have all 3:
1) 2+ of the following w/ at least 1 being i-iii:
i. delusions
ii. hallucinations
iii. disorganized speech
-
iv. disorganized or catatonic behavior
v. negative sx (affective flattening, alogia, avolition)
2) disturbance 6+ months w/ at least 1 month #1
3) 1+ areas of life impacted
Patient presents to the ED for inability to move both legs. This began in the feet 5 days ago but has since progressed. On exam, reflexes are 0 in the ankles and 1+ in the knees. Patient recently got over a GI illness but has been otherwise well. What CSF finding is characteristic of the most likely condition?
This is Guillain-Barre syndrome, and albuminocytologic dissociation (high protein and normal WBC count) would be found on CSF sampling. This is due to the absence of infection with a high amount of antibodies produced.
A 35 yo M with PMH schizophrenia presents with AMS and tremors x 2d. VS were as follows: HR 150, BP 132/85, RR 18, Sp 93% RA, T 104F. On exam, patient is rigid, diaphoretic, and hyporeflexic. Patient is unable to participate meaningfully in interview. Per roommate, patient has not experienced any falls or adverse events as of late. What 2 lab findings would confirm your diagnosis, and what is/are the treatment(s) of choice for the most likely condition?
Dantrolene is a skeletal muscle relaxant and bromocriptine is a DMN agonist. Leukocytosis and elevated CK/myoglobinuria would confirm the diagnosis.
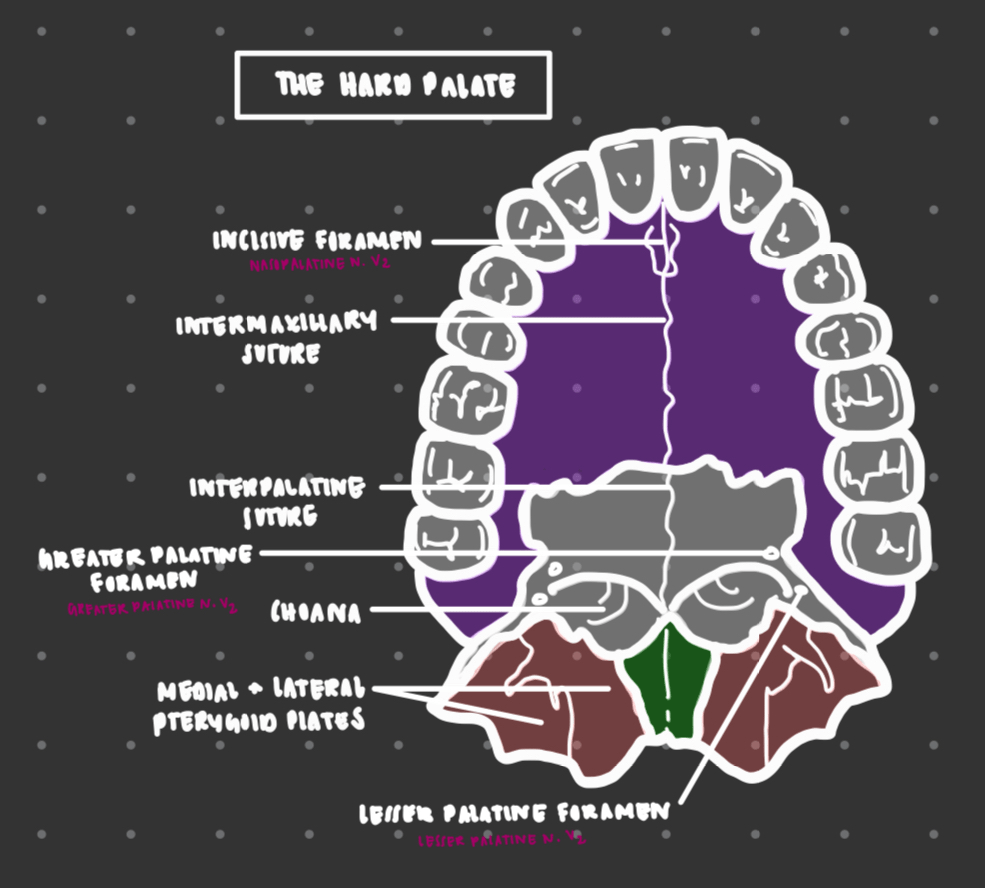
There are 3 foramen that branches of trigeminal nerve must travel through to supply the palate. What are the names of these nerves, and which component(s) of CN V travel through each?
1) Nasopalatine nerve (V2) travels through the incisive foramen to supply the anterior hard palate.
2) Greater palatine nerve (V2) travels through the greater palatine foramen to supply the posterior hard palate.
3) Lesser palatine nerve (V2) travels through the lesser palatine foramen to supply the soft palate and anterior uvula.
Patient presented to the ED because he was bumping into objects in the left field of his vision. On further examination, patient was also noted to have deficits in perception of emotional endowment of speech. Which artery is impacted? Be specific!
inferior division R MCA
Language is on the left, emotional endowment of speech and perception thereof on the right.
Patient presents 5 weeks after having been attacked by an assailant while walking on the street. They have been having distressing dreams and difficulty sleeping since the incident. The patient also takes another route home to avoid the area where they were harmed. She often blames herself for not paying better attention to her surroundings and has not felt happy since the incident. Patient expresses they have been having angry outbursts and startle very easily. What is the diagnosis, and what are the management options? Include specific pharmacotherapy.
This is PTSD, as the patient has exposure with constellation of sx (intrusion, avoidance, cognition, mood, arousal, reactivity) persistent 30d to 6mo afterwards. Tx modalities include CBT, EMDR, and SSRIs (sertraline & paroxetine specifically). Prazosin can also be used for nightmares.
3d-1mo --> acute stress disorder
1-6mo --> PTSD
onset w/i 3 mo of stressor --> adjustment disorder
6+ months --> chronic PTSD
A 73 yo M with PMH diabetes, HTN presents to OP clinic with his daughter. She is concerned that he's "not all there." Per collateral, patient began moving more slowly and developed a tremor approx 6 months ago. The patient now occasionally sees "little people" running around. What mutation is most likely responsible for the most likely diagnosis?
Because the dementia onset was < 1 year from the onset of parkinsonism, this is likely lewy body dementia (LBD) rather than parkinson's disease with dementia (PDD). PDD requires onset of dementia over 1 year after onset of parkinsonism. In either event, an SNCA mutation leads to overexpression of alpha-synuclein proteins, and the misfolded aggregates become toxic to neurons.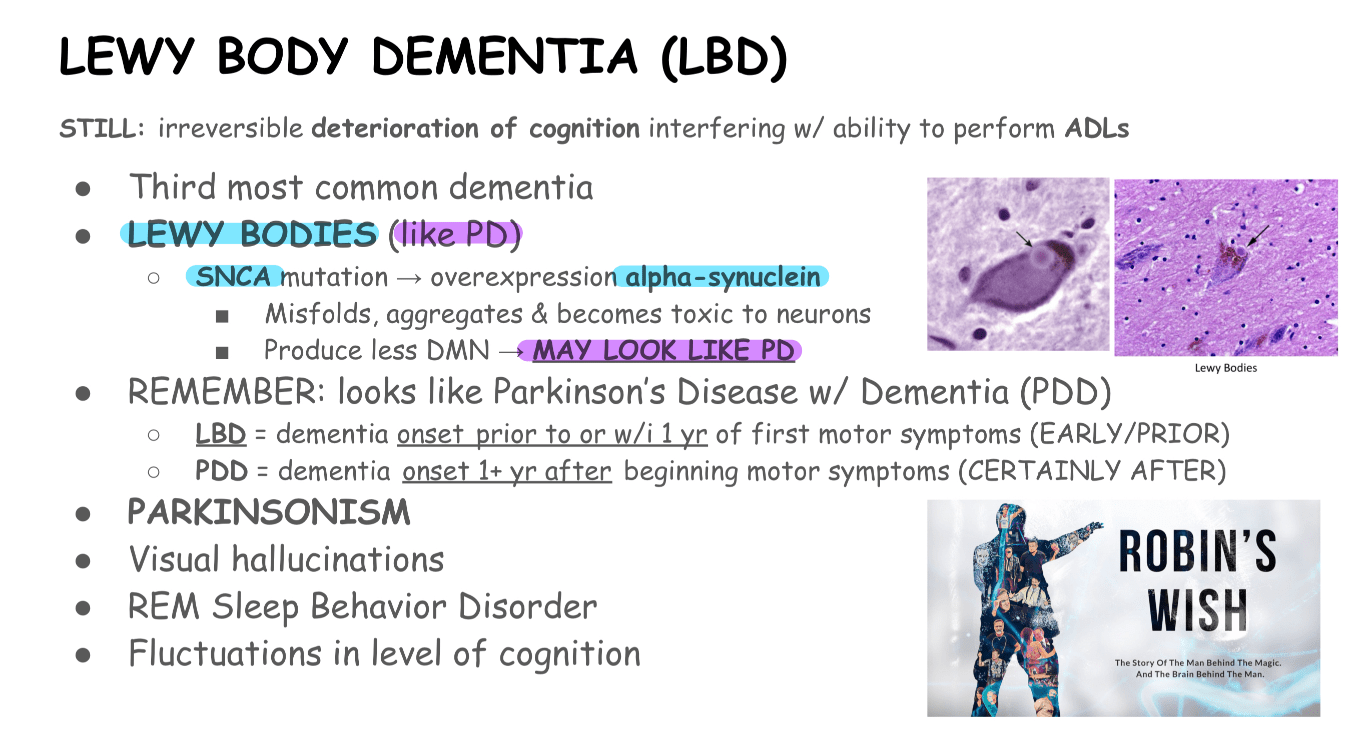
A 54 year old F on wards with PMH bipolar disorder develops rapidly-progressive diarrhea and tremor. Physical exam unremarkable, though she did receive new dx of CHF this week, for which she received diuretics. What is the most likely cause of her current presentation?
Lithium toxicity secondary to thiazide diuretic administration.