The bladder is supplied by the superior and inferior vesical arteries. These are branches of what artery?
Internal iliac
Clinicians should encourage bladder cancer patients to adopt healthy lifestyle habits including exercise, a healthy diet, and what?
Smoking cessation
Bladder cancer is the second most common tobacco-related malignancy. Successful cancer treatment can be significantly compromised by continued tobacco use. A bladder cancer diagnosis is an opportunity to promote smoking cessation. Clinicians can and should play an integral role in affecting patterns of tobacco use by patients with bladder cancer.
A 43-year-old man has a 4 cm micropapillary urothelial carcinoma that extensively invades the lamina propria near the bladder dome. Muscularis propria is present and uninvolved. The next step is
A. restaging TURBT.
B. partial cystectomy.
C. neoadjuvant chemotherapy followed by radical cystectomy.
D. radical cystectomy.
E. chemotherapy
ANSWER=D
T1 tumors with aggressive features (tumor size > 3 cm, micropapillary histology, and lymphovascular invasion) have an increased risk of progression and should undergo definitive cystectomy that is highly effective for early stage tumors. While intravesical BCG is an option for the treatment of T1 bladder cancer, the high risk features of this tumor leave the patient at a very high risk of relapse and progression. This is inappropriate given his young age and excellent health. Partial cystectomy is not the best choice for tumor control given the high risk of multifocal recurrences within the remaining bladder. Prophylactic radiotherapy and systemic chemotherapy have not been shown to reduce the risk of recurrence in individuals with 11 disease. Micropapillary urothelial carcinoma is unlikely to respond to intravesical therapies. The use of neoadjuvant chemotherapy in non-muscle invasive disease is unproven, so immediate cystectomy is most appropriate.
A 54-year-old man has chemoradiation for a cT2 urothelial carcinoma of the bladder. After two cycles of cisplatin and 40 Gy XRT, he has a mid-treatment TURBT. Pathology reveals high-grade T1 urothelial cancer. The next step is:
A. repeat TURBT.
B. complete planned chemoradiation.
C. change to dose dense M-VAC chemotherapy.
D. induction BCG.
E. radical cystoprostatectomy.
ANSWER=E
Bladder preservation strategies with use of either radical TURBT and chemotherapy or tri-modality therapy with TURBT, chemotherapy, and radiation therapy, have been utilized in many clinical scenarios, usually reserved for elderly patients with more comorbidities and limited life expectancy. However, these strategies are being increasingly utilized in the healthier population as the outcomes for bladder preservation in certain subsets appear favorable. Additionally, various strategies of types of chemotherapy and radiation doses have been utilized. The RTOG (Radiation Therapy Oncology Group) has defined various protocols for chemoradiation and bladder preservation. Typically, patients receive two cycles of chemotherapy with concomitant radiation therapy, and then undergo a mid-cycle transurethral resection for response assessment. If there is persistent disease, then the recommendation for cystectomy is given at that time. If there appears to be an adequate response, then completion of chemoradiation therapy is recommended. In this case, persistent T1 disease at the mid-cycle evaluation indicates an inadequate response to induction therapy and salvage radical cystoprostatectomy is indicated. Repeat transurethral resection after finding T1 disease at mid-cycle is not recommended, nor is changing chemotherapy or increasing planned radiation therapy dosing. Completing standard chemoradiation therapy protocols in the setting of active invasive disease would result in delayed treatment of resistant disease. BCG has been used to treat delayed recurrence of non-muscle invasive bladder cancer after trimodal therapy, but not when this occurs at the mid-treatment evaluation.
Squamous metaplasia
The distal ileum is supplied by the ileal branch of this artery and direct intestinal branches of another artery which anastomose in the region of the distal ileum. Name both.
Who should be offered adjuvant chemotherapy after radical cystectomy?
Patients who have not received cisplatin-based neoadjuvant chemotherapy and have non-organ confined (pT3/T4and/or N+) disease at cystectomy should be offered adjuvant cisplatin- based chemotherapy.
All of the AC trials were terminated early, and therefore are underpowered to provide sufficient evidence to state definitively the benefit of AC in MIBC. However, meta-analyses have suggested a possible benefit, albeit based on data of variable quality. Thus, the Panel advocates that cisplatin-eligible patients with high-risk pathologic features who do not receive NAC be offered adjuvant therapy following radical cystectomy
A 73-year-old woman with high-grade muscle invasive bladder cancer in the bladder neck and dome of the bladder as well as CIS desires an orthotopic urinary diversion. The strongest relative contraindication to this type of diversion would be:
A. age.
B. multifocal disease.
C. presence of CIS.
D. preoperative unilateral hydronephrosis.
E. bladder neck involvement.
ANSWER=E
The incidence of tumor involving the urethra in women undergoing cystectomy for bladder urothelial carcinoma is approximately 12%. The urethral recurrence rate in properly selected patients is low at less than 4%. Bladder neck tumor involvement in women, however, may be seen in approximately 22% of patients and is a risk for a urethral tumor in about half (12%). Preoperative involvement of the bladder neck with tumor in women is not an absolute contraindication as long as full-thickness, intraoperative, frozen section analysis reveals no tumor involvement of the proximal urethra (distal surgical margin). Age, tumor grade and pathological stage do not appear to be significant risk factors or contraindications to orthotopic diversion in women. CIS and multifocality also increase the risk of urethral occurrence, but not to the same degree as bladder neck involvement.
A 70-year-old man is undergoing radical cystectomy and orthotopic urinary diversion for muscle-invasive high-grade urothelial carcinoma. During lymphadenectomy, an unexpected 1.5 cm external iliac lymph node is confirmed to be a metastasis. The next step is:
A. abort surgery and treat with chemotherapy and XRT.
B. abort surgery and treat with chemotherapy followed by cystectomy.
C. perform lymphadenectomy and treat with chemotherapy and XRT.
D. complete surgery and perform ileal conduit.
E. complete surgery as planned.
ANSWER=E
At the time of radical cystectomy, suspicious lymph nodes can be encountered. Approximately 25% of patients will ultimately have positive lymph nodes at the time of radical cystectomy. If the suspicious node(s) can be safely resected and the volume of suspicious lymph nodes is limited, it is reasonable to continue the cystectomy and orthotopic urinary diversion. The patient will benefit from the local control of the lymphadenectomy and cystectomy. There is no evidence that stopping surgery and treating with chemotherapy or chemotherapy and XRT is superior to completing the cystectomy. Positive lymph nodes are not a contraindication to orthotopic urinary diversion.

Cystitis cystica et glandularis
A large nerve courses next to the bladder and can be stimulated during TURBT. What is its function?
Daily double: Name 2 techniques that can reduce the risk of stimulating this nerve during TURBT.
Motor innervation of hip adductors. Sensory innervation of the medial thigh.
DD: bladder underdistension, bipolar energy (maybe), staccato resection, neuromuscular blockade (general or spinal with an obturator block)
2 perioperative medications have a "strong" recommendation at the time of radical cystectomy. Name both.
VTE prophylaxis and peripherally active µ-opioid receptor antagonists
Delayed return of bowel function is a common event following radical cystectomy and a source of morbidity and prolonged hospital stay. The use of peripherally active µ-opioid receptor antagonists has been shown to enhance the recovery of bowel function and decrease hospital length of stay in patients undergoing radical cystectomy and other abdominal surgical procedures.
Given the significant risk of morbidity and mortality, and the strong evidence to support the efficacy of prophylaxis, the Panel recommends the use of combined mechanical and pharmacologic prophylaxis in patients undergoing radical cystectomy. Strong consideration should be given to initiating pharmacologic prophylaxis just prior to induction of anesthesia. Increasing evidence suggests that a preoperative dose may decrease venous thromboembolism risk. Perioperative coverage with up to four weeks of treatment following surgery may be beneficial.
A 60-year-old man is diagnosed with a single focus of CIS of the bladder. He is treated with six doses of intravesical BCG. A month after his last dose, his cystoscopy is normal and his cytology is negative. The next step is:
A. bladder biopsy to confirm complete response.
B. observation with regular surveillance cystoscopy and cytology.
C. maintenance BCG with the first of three weekly doses at three months.
D. maintenance BCG with the first of three weekly doses at six months.
E. maintenance BCG single monthly dose for one year.
ANSWER=C
BCG maintenance therapy is indicated for patients with CIS, even if focal, who achieve a complete response. The Southwest Oncology Group (SWOG) reported the most significant impact of maintenance therapy. Patients received a six-week induction course followed by three weekly instillations at three and six months and every six months, thereafter, for three years. This patient is at the three month point and should receive the first set of maintenance treatments as the next step. Estimated median recurrence-free survival was 76.8 months in the maintenance arm and 35.7 months in the control arm (P = .0001). Bladder biopsy is not necessary if the patient's cystoscopy and cytology are negative. Observation alone is not optimal therapy unless the patient has a contraindication or serious complication from BCG. Monthly BCG has been described and is commonly used, but has not been tested against the maintenance schedule proven to be effective in the large published SWOG trial.
A 62-year-old man undergoes a TURBT for a lesion at the bladder dome. Final pathology reveals muscle-invasive small cell carcinoma. Metastatic work-up is negative. The next step is:
A. repeat TURBT.
B. neoadjuvant chemotherapy.
C. XRT.
D. partial cystectomy.
E. radical cystoprostatectomy.
ANSWER=B
Small cell carcinoma of the bladder is a relatively rare tumor that may arise in combination with
urothelial carcinoma. ft is usually biologically aggressive with early vascular and muscular invasion. These malignancies usually respond to but are not cured by chemotherapy regimens. Neither partial or initial radical cystectomy nor intravesical chemotherapy is appropriate in this
setting. Radiation or extirpative surgery alone may result in cure rates of 5-20%. However, neoadjuvant chemotherapy followed by surgery or radiation therapy results in cure rates of 40- 65%. Therefore, the best treatment is chemotherapy followed by local treatment such as surgery or radiation if the patient does not progress.

Bladder leiomyoma
The urothelium is comprised of 3 cell types. Basal cells, intermediate cells, and umbrella cells.
Non muscle bladder cancer is thought to arise from which cell type?
Daily double: CIS?
CIS, MIBC: basal cells
In a patient with NMIBC, a clinician may use biomarkers in 2 clinical situations. What are these cases?
Daily double: Name the 2 biomarkers
Answer: assess response to intravesical BCG (UroVysion® FISH) and adjudicate equivocal cytology (UroVysion® FISH and ImmunoCyt™)
The presence of significant inflammation immediately post BCG instillation can affect the accuracy of urine cytology. Urinary markers may be used to assess response to intravesical BCG therapy. In examining the change in UroVysion ® FISH results before and after an induction or induction + maintenance course of BCG, several studies have noted a correlation between response to BCG and likelihood of disease progression. Based on these studies, it appears that the presence of a persistently positive UroVysion ® FISH following completion of induction BCG predicts a poor response to BCG therapy with a higher likelihood of recurrence and progression. Based on these data, clinicians can use UroVysion ® FISH as an early guide to predict response to intravesical BCG therapy. The utility of protein-based markers in this setting has not been well tested, but as with cytology, inflammation may also negatively impact their ability to predict response.
Equivocal urine cytology can occur in as high as 21% of patients being evaluated for hematuria. Performance of a complete diagnostic workup to rule out cancer is typically the default approach in many of these patients with atypical cytology readings and is one reason why its routine use is no longer advocated for hematuria evaluations. Even in patients with high-grade cancers, cytology may be read as suspicious or atypical. Thus, utilization of another test to arbitrate an atypical or equivocal cytology reading may be helpful in reducing the need for unnecessary diagnostic evaluations in intermediate- and high-risk bladder cancer patients. Several studies have used ImmunoCyt ™and UroVysion ® FISH in this context. Both of these urine markers have been found to help distinguish between patients with malignancy versus no recurrence.
A 54-year-old woman is diagnosed with CIS of the bladder. She is currently taking methotrexate and prednisone for severe rheumatoid arthritis. The next step is:
A. intravesical BCG.
B. intravesical valrubicin.
C. intravesical gemcitabine.
D. taper off methotrexate and prednisone then administer BCG.
E. radical cystectomy.
ANSWER=A
Immunocompromised patients are generally considered to be contraindicated to receive intravesical BCG therapy due to the theoretical concerns of loss of efficacy and increase in toxicity. However, there exists little evidence to support or refute such claims. A recent report from Herr and Dalbagni demonstrate the safety and efficacy of intravesical BCG in immunocompromised patients including patients with autoimmune disease, transplant patients, and patients undergoing systemic chemotherapy. The authors demonstrated that intravesical BCG is safe and effective in immunologically compromised patients with bladder cancer with the majority of patients (91%) having an initial complete response. Transplant patients fared worse but still demonstrated a response to BCG with acceptable tolerability. Therefore, an initial trial of BCG therapy can be considered in this patient following appropriate counseling about risks, benefits, and safety issues. Valrubicin was approved by the FDA in 1998 for the treatment of BCG refractory CIS of the bladder in patients who are medically unfit or refuse a cystectomy, with modest efficacy observed in this setting. It is not indicated in this setting and its role in the immunocompromised patient is uncertain. Although thiotepa is the only intravesical chemotherapeutic agent FDA-approved for papillary bladder cancer, it may result in significant myelosuppression which would be of particular concern in the immunocompromised patient. Furthermore, its efficacy in CIS is limited and it has not been studied in this setting. Intravesical gemcitabine has been shown to have activity in non-muscle invasive bladder cancer in high-risk patients. Although early results are promising in the second line or salvage setting, the limited patient population evaluated supports the need for additional phase II and phase Ill studies. Moreover, its efficacy in the immunocompromised patient is unknown. Radical cystectomy is a reasonable option, but may be too aggressive for this patient as a first line option with untreated CIS.
The most important clinical or pathologic parameter associated with progression of non-muscle-invasive bladder cancer is:
A. tumor stage.
B. early recurrence.
C. location.
D. presence of mutant p53.
E. age.
ANSWER=A
Several useful prognostic parameters exist for tumor progression in patients with Ta/Tis/T1 bladder cancer. The most important of these are tumor stage, grade, and presence of CIS. Tumor size and multiplicity are other factors that may predict progression. Early recurrence is not associated with progression of the disease, except in patients with BCG treatment failure. The relationship between p53 status and tumor progression remains unclear. Age and tumor location do not impact progression risk.

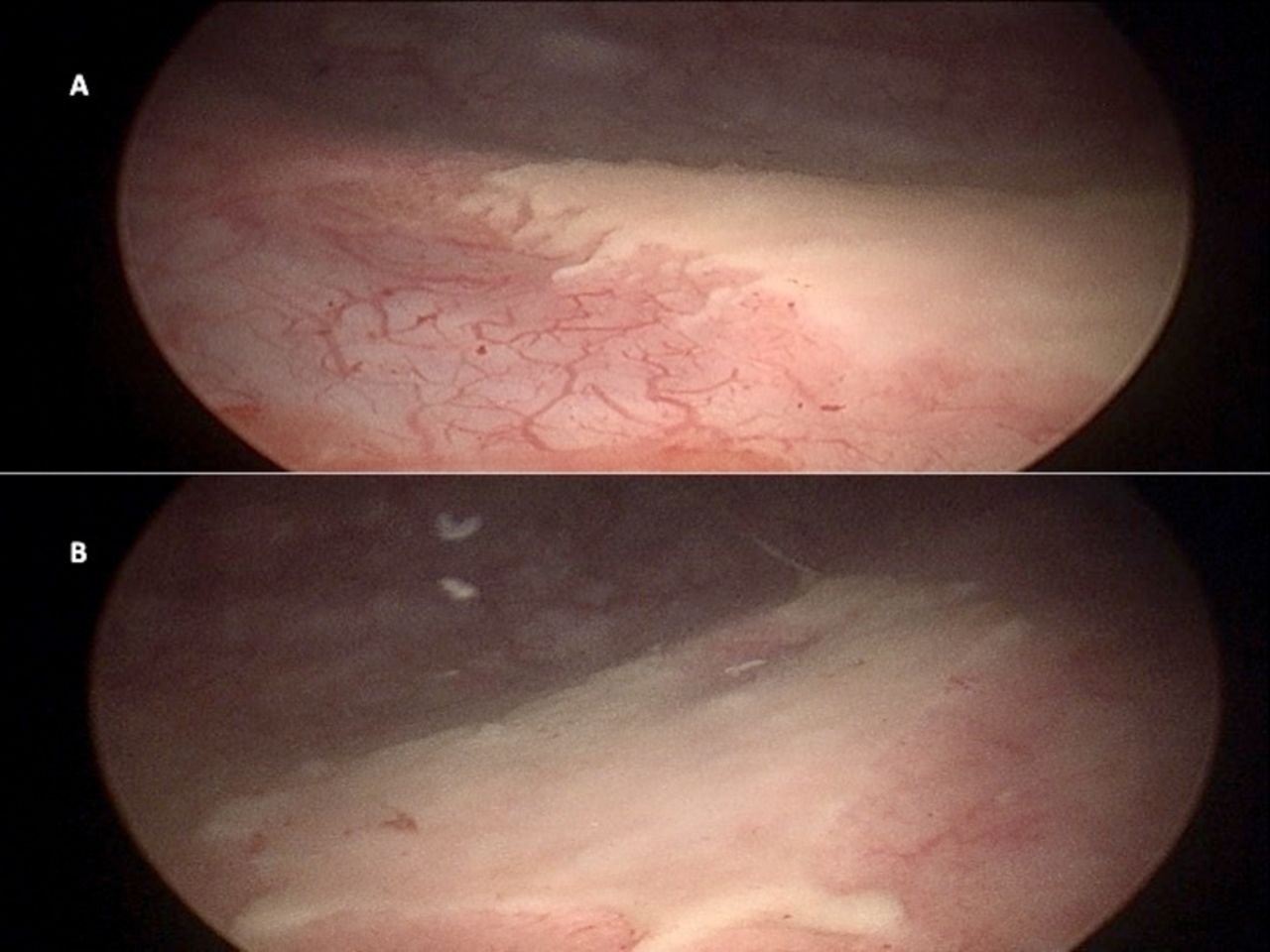
Hunner's ulcer/IC
A patient undergoes radical cystectomy and extended pelvic lymph node dissection for muscle invasive bladder cancer. Preoperative MRI showed a 2 cm VIRADS 3 lesion and CT scans of the chest abdomen and pelvis showed no suspicious LAD or other lesions. His final pathology shows urothelial carcinoma in the posterior bladder invading the prostatic stroma. There is microscopic metastatic urothelial carcinoma is found in 3 external iliac nodes and 2 para-aortic nodes. What is his TNM stage?
Daily double: What is the significance of VIRADS 3
pT4aN2M1

VIRADS
VIRADS 1: muscle invasion highly unlikely
VIRADS 2: muscle-invasion unlikely
VIRADS 3: muscle-invasion equivocal
VIRADS 4: muscle-invasion likely
VIRADS 5: invasion beyond bladder is very likely
A patient with high-grade T1 disease after a single course of induction intravesical BCG should next be offered what therapy?
Radical cystectomy
Data have demonstrated adverse cancer-specific survival among patients with NMIBC recurrence after BCG who undergo delayed versus early cystectomy. Patients initially with NMIBC who progress to muscle invasion have been found to have a worse prognosis than patients initially presenting with muscle-invasive disease. In a retrospective comparative analysis, patients with T1 recurrence after BCG treated with radical cystectomy were noted to have a decreased five-year cumulative incidence of death from disease (31%) compared to patients with T1 recurrence after BCG treated with repeat resection and BCG (48%).
A 45-year-old man with a T6 spinal cord injury managed with an indwelling urethral catheter is diagnosed with a 6 cm T2 high grade urothelial carcinoma with squamous differentiation. The tumor is located near the dome and random biopsies are negative. The metastatic evaluation is negative. The next step is:
ANSWER=B
A recent secondary analysis of the SWOG neoadjuvant chemotherapy trial testing M-VAC followed by cystectomy vs. cystectomy alone for muscle invasive bladder cancer showed that the survival benefit to chemotherapy in patients with mixed histology including squamous or glandular differentiation was actually superior to that seen in patients with pure urothelial cancer. Partial cystectomy is not appropriate for large urothelial carcinomas regardless of their location. Radical cystoprostatectomy and ileal conduit will be appropriate after chemotherapy or if the patient cannot safely have chemotherapy due to comorbidities or other constraints such as poor renal function. Adriamycin-based chemotherapy is used for pure squamous cell carcinoma of other primary sites but has no role in urothelial carcinoma. Chemotherapy and XRT are not preferred in a patient that is otherwise a surgical candidate. If the patient had pure squamous cell carcinoma, immediate radical cystoprostatectomy would be appropriate.
An 81-year-old man has muscle-invasive urothelial carcinoma of the bladder with multifocal CIS. Metastatic evaluation is negative. GFR is 48 mL/min. The next step is:
A. chemoradiation therapy.
B. cisplatin-based chemotherapy followed by radical cystectomy.
C. carboplatin-based chemotherapy followed by radical cystectomy.
D. radical cystectomy.
E. radical cystectomy followed by adjuvant chemotherapy.
Daily double: List 3 clinical factors that can be used to consider a patient a candidate for TMT.
ANSWER=D
The patient presents with muscle-invasive bladder cancer (cT2) with a notable history of renal insufficiency and advanced age. Nevertheless, he remains a candidate for radical cystectomy and this should be the primary recommendation. Comorbidities, not age, should be used when deciding on radical cystectomy, and surgery can and should be considered for this patient as multiple series have demonstrated benefits of radical cystectomy in elderly patients with invasive disease. Multifocal CIS is a contraindication for chemoradiation therapy alone. Neoadjuvant chemotherapy Is intended for patients with operable clinical stage T2 to T4a muscle-invasive disease. Although the data available supports the use of either M-VAC (Methotrexate, Vinblastine, Adriamycin, and Cisplatin} or CMV (Cisplatin, Methotrexate, and Vinblastine) as neoadjuvant chemotherapy, it has been estimated that more than 50% of patients are ineligible for cisplatin based chemotherapy because of impaired renal function or medical comorbidities. This patient has impaired renal function that will preclude the use of cisplatin-based neoadjuvant chemotherapy. In patients with compromised renal function, carboplatin + gemcitabine has been utilized. However, the efficacy of carboplatin-based regimens in the neoadjuvant setting is unproven and may contribute to a delay in definitive surgery without a known oncologic benefit. Adjuvant chemotherapy has been advocated for high-risk patients (pT3-4, N+ patients) in an effort to delay recurrence and prolong survival. Unfortunately, the question of the true benefit of adjuvant chemotherapy in high-risk patients with pT3, pT4, and N+ disease is currently unknown. Although this patient may be a candidate for adjuvant chemotherapy, the decision to pursue such an approach will depend on his pathologic staging, and is, therefore, not a foregone conclusion.
Daily double: Urothelial histology; Maximal TURBT; Clinical T2 to T3a disease; Absence of tumor-associated hydronephrosis; Adequate renal function for cisplatin; Absence of extensive CIS; Unifocal tumors <6 cm in maximum diameter;Good bladder function and capacity (ie, a bladder worth sparing)

Bladder cancer