What areas are typically spared in this condition?
Face, palms, soles usually spared
Pityriasis rosea: onset ~10-35 yo; typically lasts 6-8 wks but can be >5 mo.
Herald patch ~2-4 cm but ranges 1-10 cm that may occur as first sign or simultaneously with widespread eruption on the trunk > neck or extremities.
+/- mild prodrome w/ HA, fever, arthralgias, general malaise. Prototypic paraviral exanthem; HHV-6/7; HHV8, H1N1 influenza, covid. May have modest seasonal variation (peak spring and fall; or rainy season).
Lesions oriented w/ long axis along Langer cleavage lines on posterior trunk and proximal extremities (Christmas tree pattern).
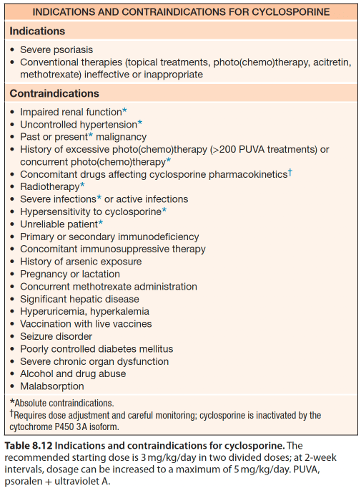
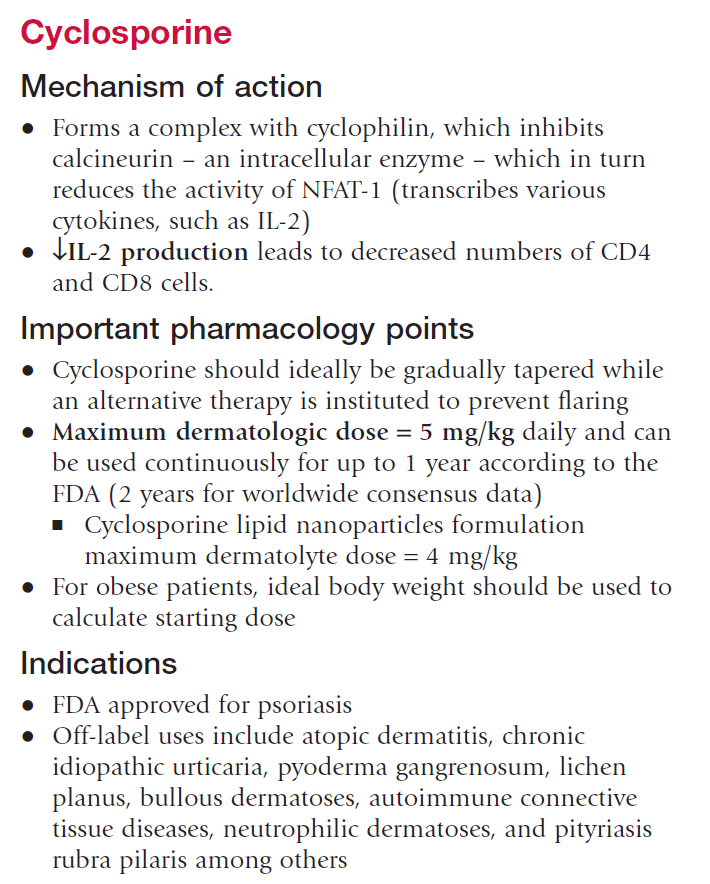
Name two contraindications to cyclosporine
Common CI: impaired renal function, uncontrolled hypertension, malignancy, history of excessive UV exposure (>200 PUVA treatments), immunosuppression, active infection, concurrent methotrexate administration
Give several month course to <1 year and alternate w/ other therapies or intermittent short courses.
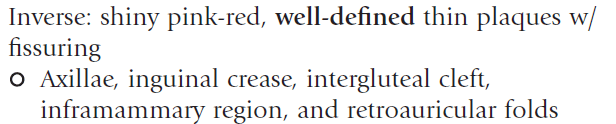
Name this variant:
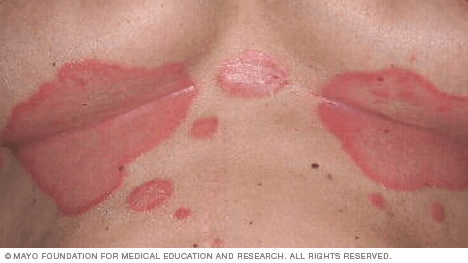
Inverse psoriasis
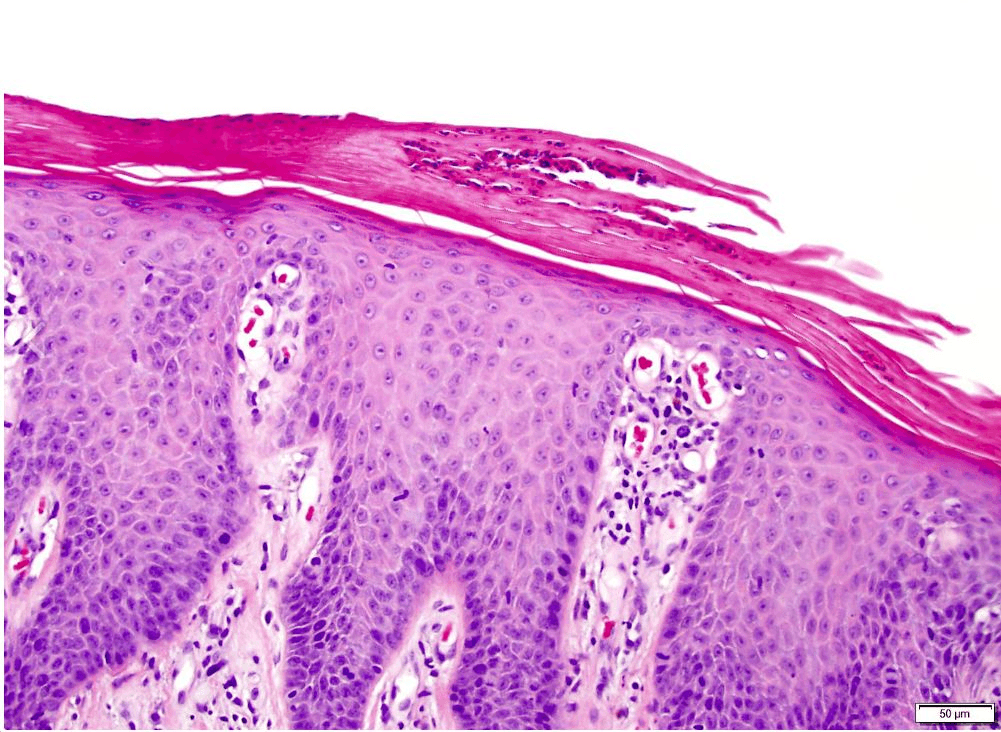
Describe the Auspitz sign
Pinpoint bleeding after removal of white/micaceous scale due to dilated capillaries and suprapapillary plate thinning
Strongest HLA association in psoriasis?
HLA-Cw6
---------------------------------------------------------
- Presence of HLA-Cw6 confers a RR of 13 for developing psoriasis in the Caucasian population and 25 in the Japanese
- Strongly linked to the age of onset of psoriasis
- More strongly associated with psoriasis type I (early onset, positive FH).
- Type II psoriasis: late onset, no FH
- In one case series, expressed in 90% of early-onset psoriasis, in 50% of of late-onset psoriasis; only in 7% of a control population
- Interacts synergistically with the ERAP1 gene (aminopeptidase involved in MHC class I antigen processing)
Name this condition:

Small plaque parapsoriasis: digitate dermatosis
Middle aged and elderly patients. Peaks in fifth decade. 3:1 M:F predominance.
Elongated finger-like pink-brown to yellow-brown patches symmetrically distributed on the flanks. +/- yellow hue (“xanthoerythrodermia perstans”)
SPP: <5cm lesions; LPP: >5cm lesions
Predominantly CD4 T cell infiltrates. Unclear if they are true entities, versus a condition on the spectrum of clonal dermatitis. Generally believed to be benign condition that carries no malignant potential, but there is controversy over whether it carries a risk of progressing into MF: LPP >SPP.
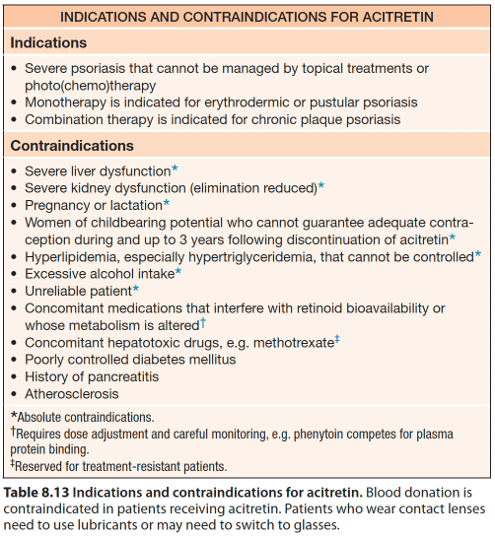
Monotherapy of which systemic agent is effective in treatment of erythrodermic and pustular psoriasis?
Acitretin (soriatane): 2nd gen retinoid; free metabolite of etretinate with half life of 3 years. Typically see improvement at 4-6 weeks and maximum benefit may take 3-4 months.
SE: Can cause pseudotumor cerebri if used in conjxn with tetracyclines, pancreatitis from hypertriglyceridemia); hyperostosis (diffuse idiopathic skeletal hyperostosis; systemic bone-forming condition characterized by the presence of at least three bony bridges at the anterolateral spine)
Do not use if:
PREGNANT
Severely impaired liver or kidney function
Chronically elevated blood lipids
In combo with tetracyclines or MTX
What are the four phenotypes of generalized pustular psoriasis?
•Von Zumbusch pattern: abrupt generalized eruption w/ erythema and pustulation leading to extensive scaling. +fever, pain, malaise. May have recurring episodes over years.
•Annular pattern: erythema and scaling with pustulation at advancing edge. Enlarge by centrifugal expansion over hours to days. Heals centrally.
•Exanthematic type: acute eruption of small pustules, with abrupt onset, and resolves over few days. Follows infection or result of medication (i.e. lithium). Usually no systemic sx. May have overlap w/ pustular drug eruptions.
•“Localized” pattern: pustules within or at edge of existing psoriatic plaques (unstable phase of chronic plaque psoriasis, or 2/2 topical irritants like tar, anthralin).
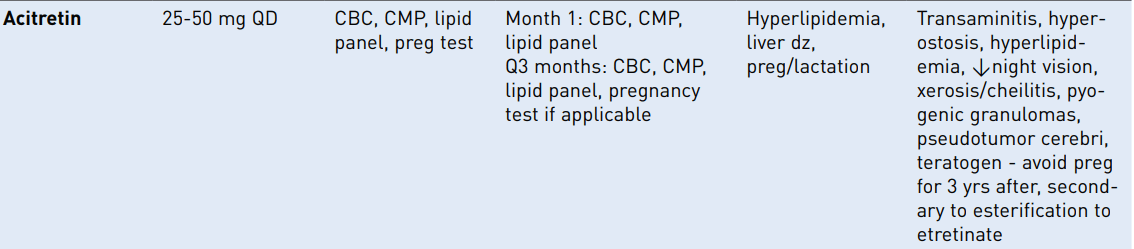
Differential diagnosis for neutrophils in the stratum corneum (name 4 of 6)
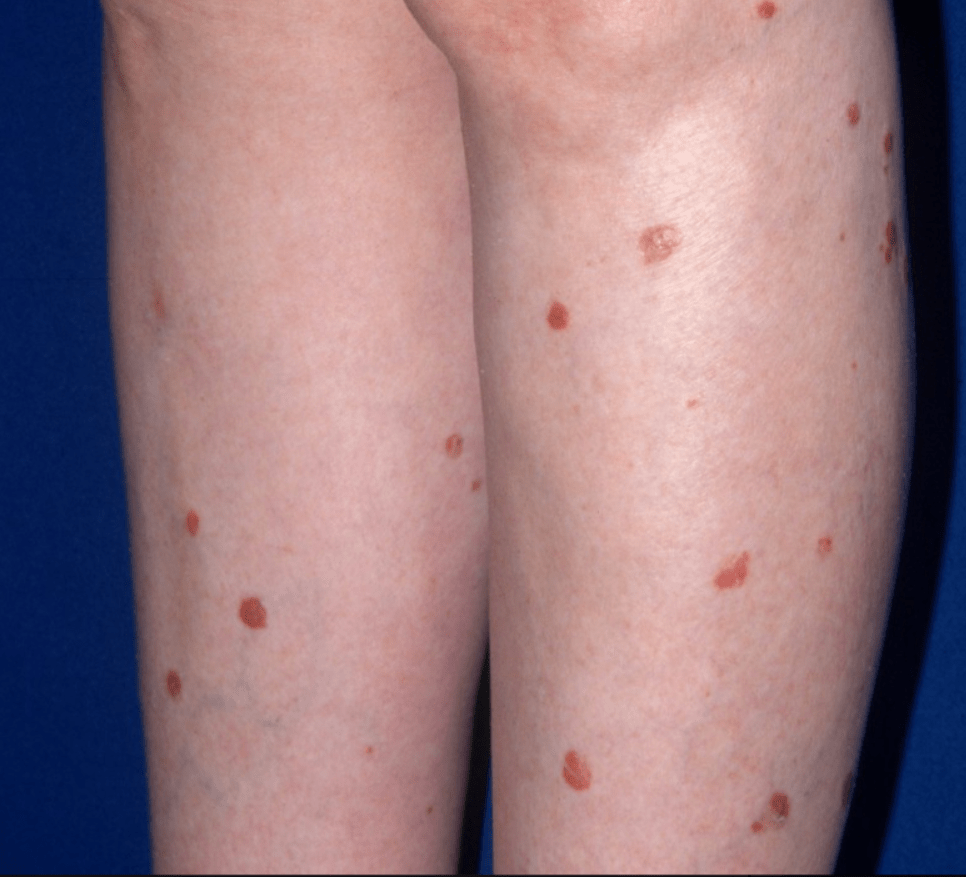
Name this condition:

Pityriasis rotunda (tinea/pityriasis circinata)
- Third decade of life, children. Slight F>M.
- Patient population: east asian (Japan, China), mediterranean (Morocco, Italy, Israel), african ancestry
No clear unifying cause; absent profilaggrin N terminal domain ~ decreased expression of FLG-2 in some patients.
Most patients are healthy; potential exacerbating factors include malnutrition, mycobacterial dz (TB, leprosy), malignancies (HCC, gastric carcinoma, multiple myeloma), hepatic cirrhosis
Favors trunk/extremities, with large circular and polycyclic lesions, often 10 cm (up to 30 cm) in dm w/ associated fine scale and moderately hyperpigmention w/ a sharp margin. Asymptomatic typically. +/- hypopigmented halo or entirety of lesions hypopigmented
Type I = black or asian patients w/ hyperpigmented lesions associated with malnutrition or internal malignancy, no family history
Type II = younger white patients w/ >30 lesions, sometimes family history, no association with other diseases
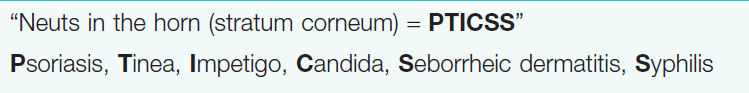
Name this condition:
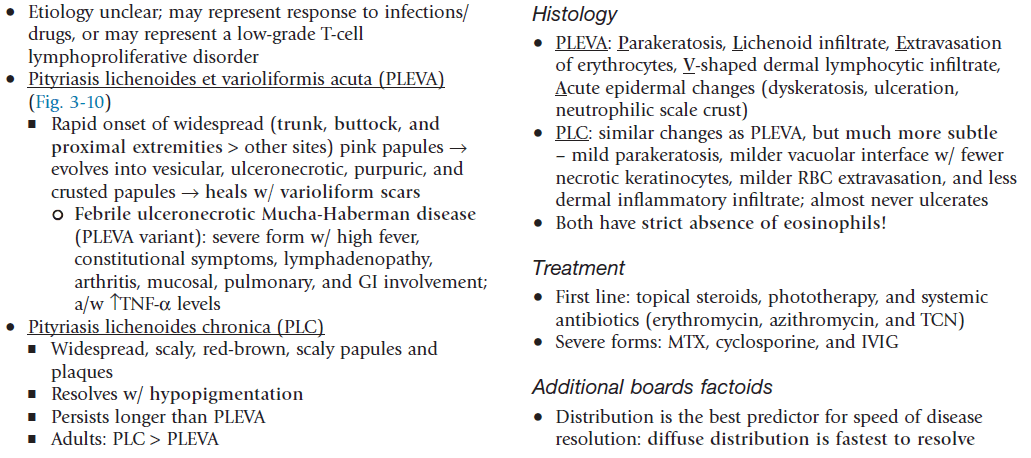
PLC - pityriasis lichenoides chronica
PLEVA (acute) and PLC (chronic) represent two ends of a disease spectrum; both are characterized by recurrent crops of self-resolving lesions
Widespread, scaly, red-brown scaly papules and plaques. Resolves with hypopigmentation
- Lasts longer than PLEVA
- More common in adults > children.
- Distribution is important: diffuse distribution = shorter avg duration (11 mo); peripheral distribution = longest avg duration (33 mo); central distribution = intermediate duration.
Which psoriasis treatment is known to paradoxically induce psoriasis?
TNF inhibitors; may cause plaque psoriasis and/or palmoplantar pustulosis
Name the laser wavelength that can best treat small areas of psoriasis.
308nm
Name the differential for this finding:
What disease is associated with the following skin findings along with fever and arthralgias?

Febrile ulceronecrotic Mucha-Habermann disease (FUMHD):
- Marked by larger, more ulcerative, and necrotic lesions along with fever and arthralgia.
- There may be gastrointestinal, pulmonary, and central nervous system (CNS) involvement.
- No consensus about first-line therapy, but wide variety of treatment modalities have been suggested to be effective, including systemic steroids, MTX, cyclosporine, dapsone, and IVIG.
What is this disorder?
Sneddon-Wilkinson / Subcorneal pustular dermatosis
-crops of sterile subcorneal vesicles/pustules with erythematous base, often annular, on flexural skin
-different from pustular psoriasis! *Has subcorneal pustules in the ABSENCE of spongiform pustules and epidermal changes of psoriasis
-*great response to dapsone
Biopsy: subcorneal pustule with neutrophils. Normal surrounding epidermis
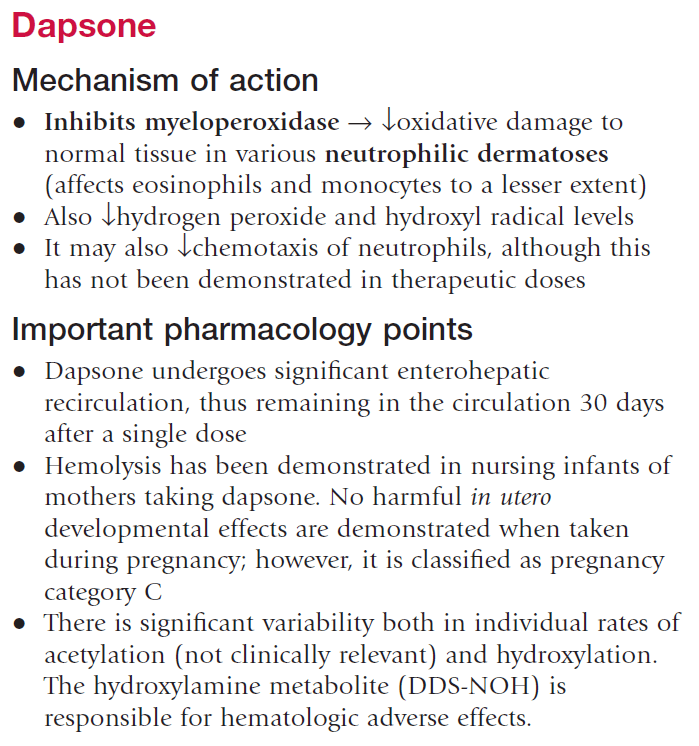
DAPSONE -resolution usually within 4 weeks, then taper
What is the mechanism of action of spesolimab-sbzo, and what condition is it approved to treat?
Monoclonbal IL-36R antibody; generalized pustular psoriasis
Spesolimab-sbzo (Spevigo) is a humanized IgG1 monoclonal antibody that blocks IL-36R, inhibiting downtream inflammatory signaling.
FDA approved in 2022 for treatment of GPP in adults. Additionally approved for pediatric patients ≥12 years of age and weighing at least 40 kg.
Administered as a single 900 mg intravenous infusion over 90 minutes. A second 900 mg IV dose may be administered one week later if flare symptoms persist. More recently, a subcutaneous formulation has been approved for maintenance therapy in eligible patients, allowing ongoing control between flares.
Most common adverse reactions reported in ≥5% of patients treated with SPEVIGO in the clinical trial leading to FDA approval were asthenia and fatigue, nausea and vomiting, headache, pruritus and prurigo, infusion site hematoma and bruising, and urinary tract infection (UTI).
Specific adverse reactions include increased infections (UTI, HSV, cellulitis), DRESS, Guillan-Barre syndrome
What is name of this variant?
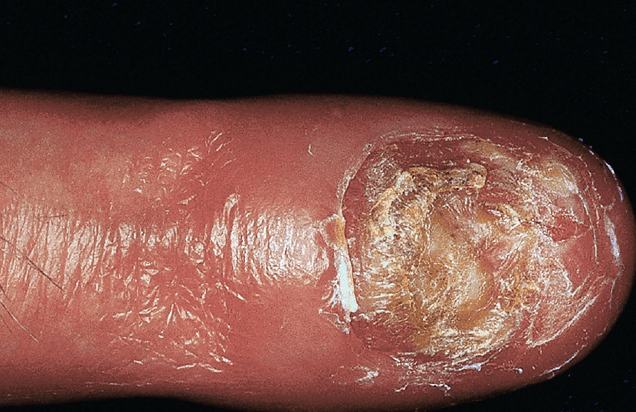
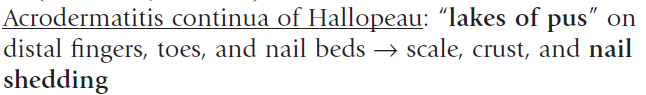
- Distal fingers w/ pustules > toes, pustules in nail bed (beneath nail plate), +/- shedding of nail plates
- Pustulation results in scaling and crust formation
+/- annulas migrans of the tongue (migratory annular erythematous lesions w/ hydrated white scale)

Name the disease
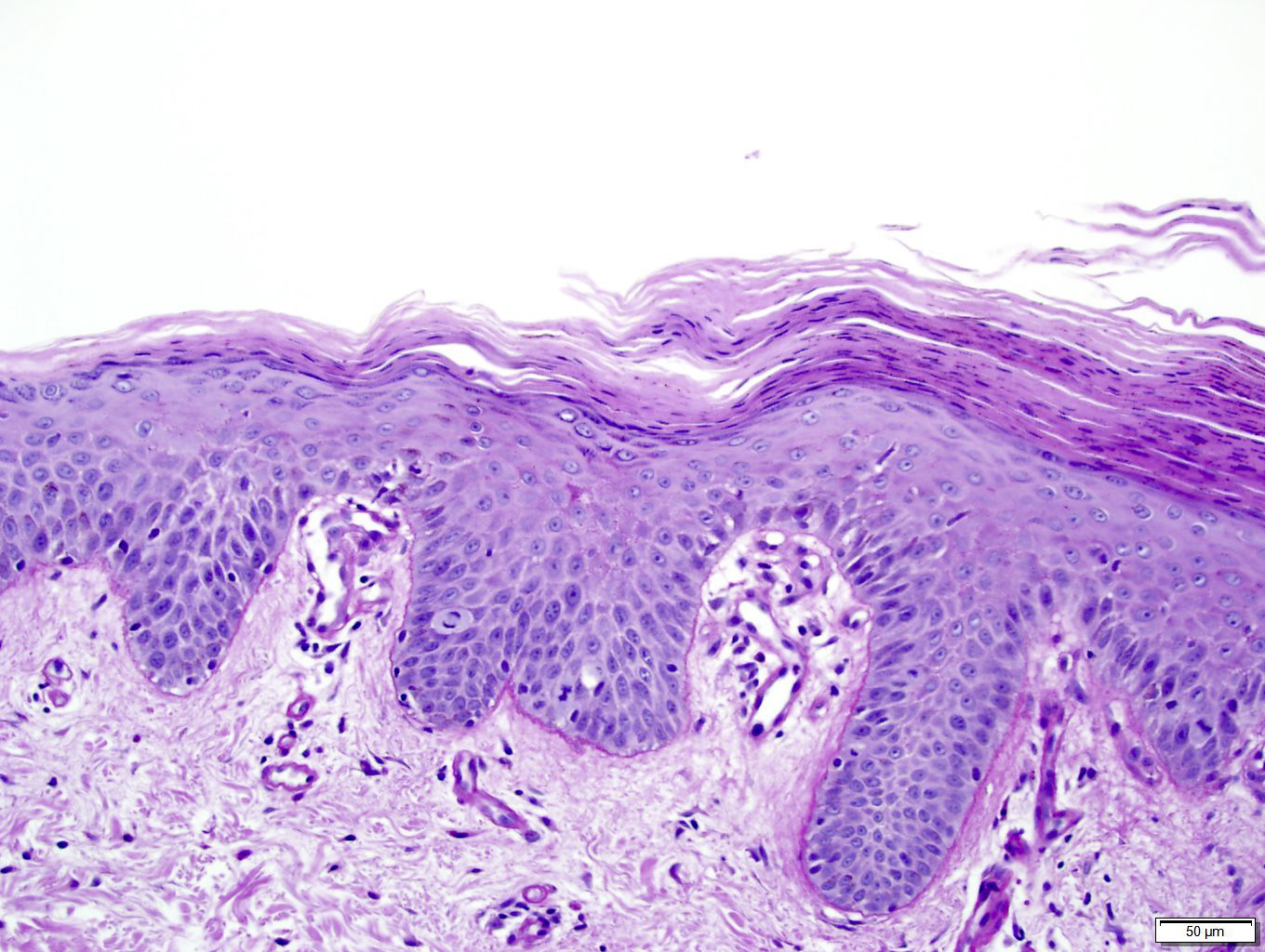

PRP
Checkerboard alternating ortho and para
Follicular hyperkeratosis with parakeratosis in shoulder of follicular plug
Which cytokine has reduced levels of expression in psoriasis?
IL-10
Increase in Th1 (IFNg, IL-2), Th17 (IL-17 A and F) and Th22 (IL-22) cytokines
Reduction in anti-inflammatory IL-10
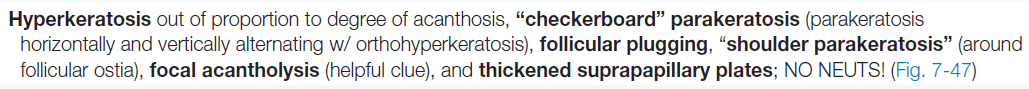
This patient had erythrodermic psoriasis and then developed this finding. What was the medication?
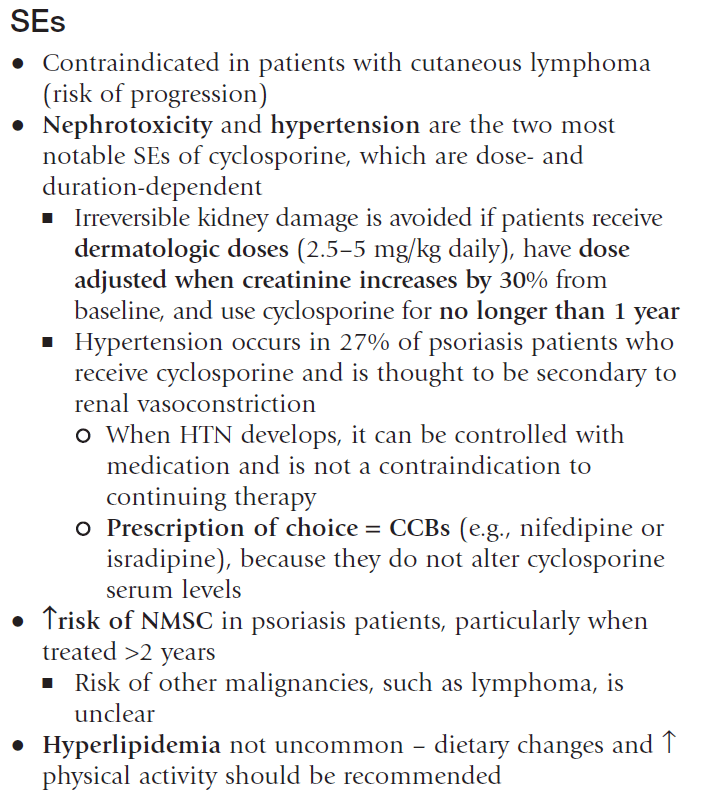
Cyclosporine
-------------------------------------------------
Cyclic undecapeptide isolated from fungus Tolypocladium inflatum
Common SE: nephrotoxicity (reduced GFR, tubular atrophy); risk for renal impairement and HTN increased; increased risk SCCs; GI discomfort, hypertrichosis, paresthesias, gingival hyperplasia, HA, vertigo, muscle cramps, tremor
Metabolic SE: hyperkalemia, hypomagnesemia, hyperuricemia (decr clearance uric acid), hypercholesterolemia and triglyceridemia
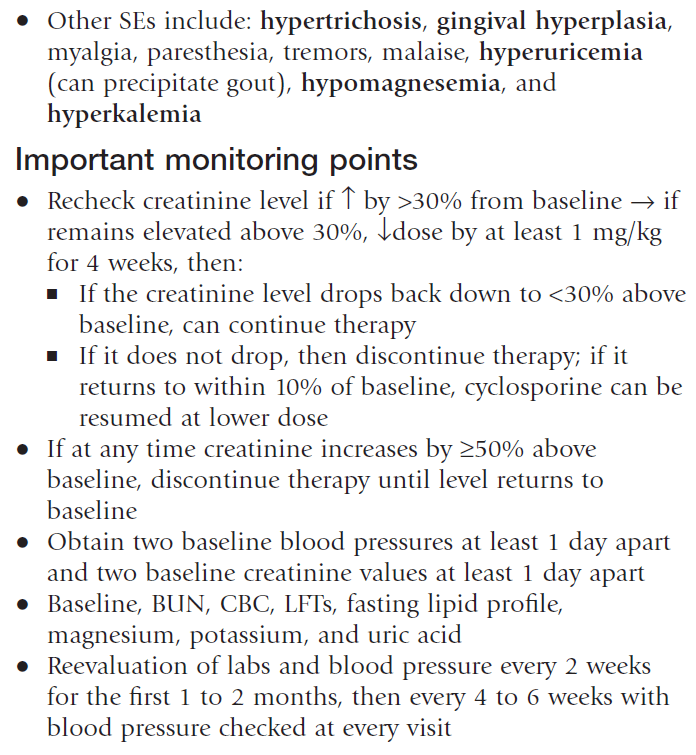
Name three triggers (i.e. external, infectious, endocrinologic, medication-induced) for psoriasis.
Common triggers:
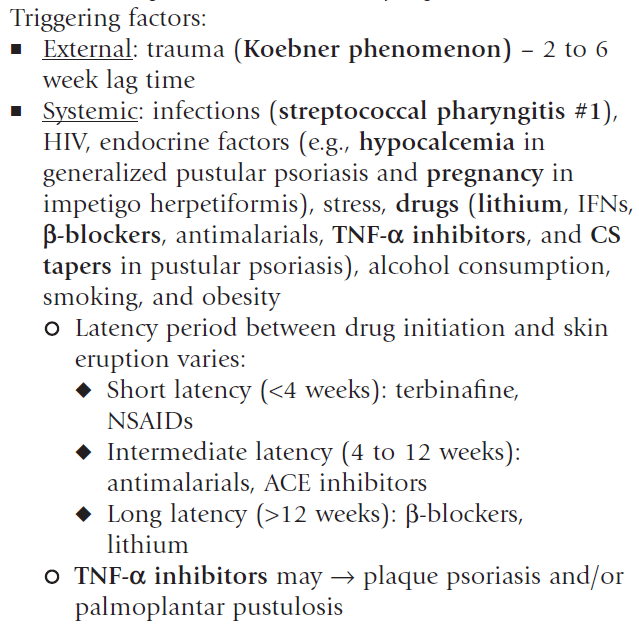
•Rapid taper of systemic steroids can induce pustular psoriasis & flares of plaque psoriasis
•TNF inhibitors can cause new onset or worsening of psoriasis (including palmoplantar)
•Dupixent for atopic dermatitis may cause psoriasiform lesions (shifting from TH2 --> TH1 response)
What is this finding called?

Woronoff's ring:
- Usually sharply demarcated
- Surrounding pale blanching ring around regressing psoriatic lesions.
What is this disease?
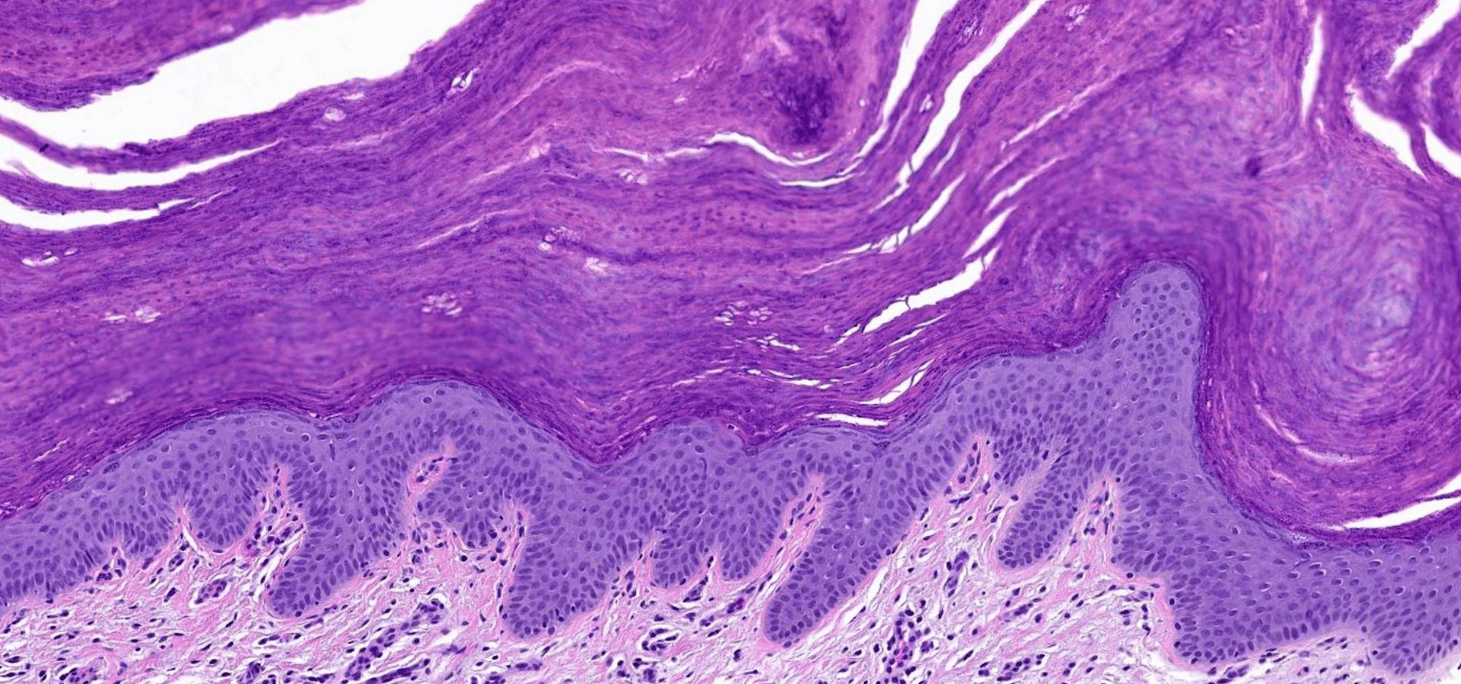
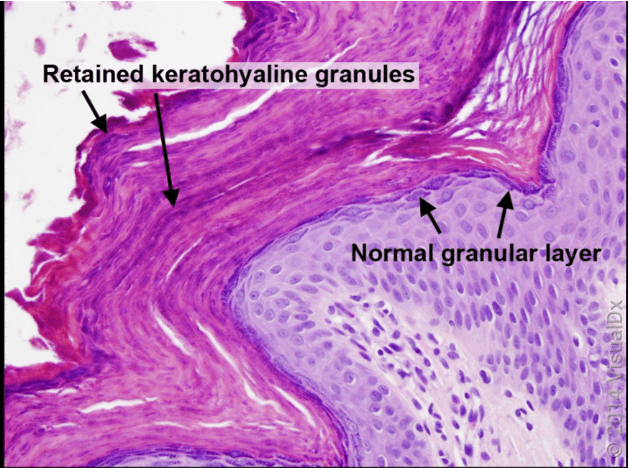
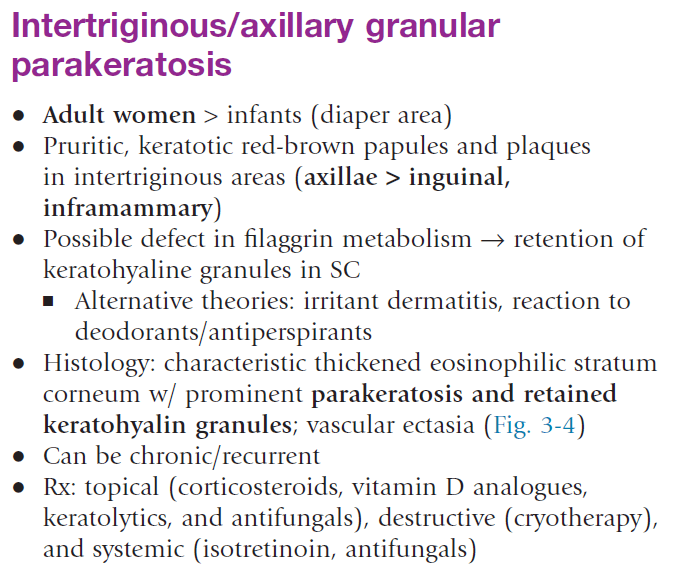
•Keratotic, brownish red papules; can be conical; may coalesce into larger, well demarcated plaques with various degrees of maceration (2/2 local occlusion)
•Coalescing brown papules w/ hyperkeratosis and slight maceration
•Associated with various personal hygiene products (deodorant, antiperspirant), occlusion from diapers (infants), or chemical irritation from benzalkonium chloride (laundry rinse aids)

What is this condition? Which subtype specifically?

Type 4 Pityriasis Rubra Pilaris
------------------------------------
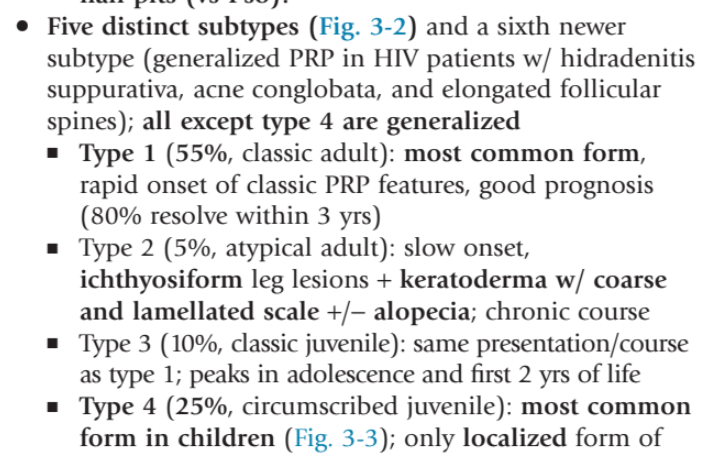
Type I: classic adult: head and neck region that progressively advances caudally. 80% clear within 3 years.
Type II: palmoplantar waxy keratoderma w/ coarse and lamellated scale, more ichthyosiform scaling on lower extremities, occasional alopecia areata; protracted clinical course
Type III: classic juvenile, closely resembles classic adult, clears within 3 years
Type IV: circumscribed, most common juvenile. Focal nature.
Type V: atypical juvenile; often due to CARD14 gof mutations. (CAPE = CARD14 assoc papulosquamous eruption). See features of PRP and psoriasis. Early age, with cheeks/chin/ears involvement; +/- palms/soles. Chronic course w/ variable response to conventional treatments.
Type VI: HIV-associated infection. May respond w/ ART. May resemble PRP type I (coalescing of inflammatory plaques into an erythroderma). May be part of a follicular occlusion tetrad that includes acne conglobata and hidradenitis suppurativa.

