# burns annually
almost 1/2 million people
Rx burns depends on
´How the injury occurred
´Causative agent (flame or scalding liquid)
´Temperature of agent
´Duration of contact with the agent
´Thickness of the skin at the injury
Emergent or resuscitative
Onset of injury to completion of fluid resuscitation
BURN triage: assess
´Prevent injury to rescuer
´Stop injury: extinguish flames, cool the burn, irrigate chemical burns
´ABCs: Establish airway, breathing, and circulation
´Start oxygen and large-bore IVs
´Remove restrictive objects and cover the wound
fluids resuscitation
´½ of calculated total volume needs to be infused within 8 hours of time of injury (not ETA of ED)
´Second half over next 16 hours
burns affect which age group ('s)?
kids and older adults, primarily occur at home
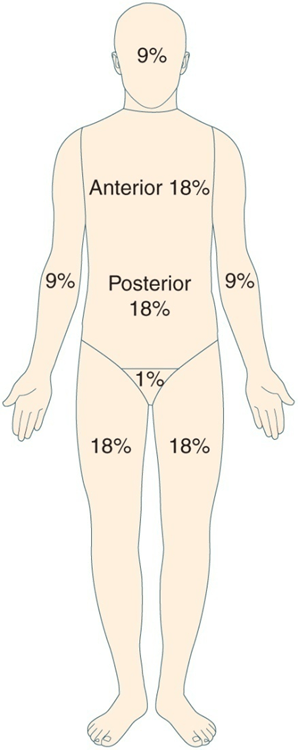
rule of nines, TBSA, based on percentage
Based on anatomic regions Head (9 %)
chest (Ant 18% Post 18%), legs (9% each leg) arms (9% each), groin 1 %
Acute or intermediate phase
From beginning of diuresis to wound closure
48-72 hours post burn
patient with falls and electrical injuries
: Treat patient for potential cervical spine injury
Potential Complications- resp
ARDS
high mortality rate
burns greater than 35% of body
rule of nines
Rehab phase
From wound closure to return to optimal physical and psychosocial adjustment. Long process includes rehab
Emergent phase algorhithm
transport to emergency department
Fluid resuscitation is begun
Foley catheter is inserted
´Patient with burns exceeding 20% to 25% should have an NG tube inserted and placed to suction
´Patient is stabilized and condition is continually monitored
´Patients with electrical burns should have ECG
´Address pain; only IV medication should be administered
´Psychosocial consideration and emotional support should be given to patient and family
complication: FVD (fluid vol deficit)
´Distributive shock- shift in intravascular fluid
outer layer of skin, sunburn
first degree/superficial
burns -which produce local and systemic response -
Major burns
Patho of burns
Loss of plasma volume, Heart workload increase with O2 demands. CO decreased; BP low
“Burn shock”
Emergent phase fluid and electrolyte shift
Hyperkalemia, hyponatremia
complication cont
Compartment syndrome-
Fasciotomy
Involve entire epidermis and varying portions of the dermis; painful with blisters
second degree/partial thickness
major burn effects
intravascular fluid shift K++ and Na ++
fluid volume deficit, edema
Greatest fluid leak with burns
first 24-36 hrs peaks in 6-8 hr.
acid base balance HCO3 low, pH low
Metabolic acidosis
complication bowel
´Paralytic ileus- bowel is dying
Total destruction of the epidermis, dermis, and underlying tissue, lack of sensation
third degree/full thickness
most people die from????
smoke inhalation, damage to pulmonary system not seen on outside
Diuresis
If body can compensate, diuresis occurs over next 2 weeks Homeostasis
Fluid Volume deficit how to treat
Isotonic fluids Ringer's lactate (had electrolytes)
complication
Paralytic ileus give: PPI omeprazole, pantoprazole
burns into muscle and deep tissue, necrosis
fourth degree
best way to treat burns
Prevent them from occurring
edema
If burns greater than 30% shift of intravascular fluid, protein and electrolytes (NA++ and K++)
RX- severe edema is fasciotomy to relieve pressure
Compartment syndrome
manage burn shock
Maintain systolic BP of greater than 100 mm Hg
urine output of 30 to 50 mL/hr;
maintain serum sodium at near-normal(135-145)
more complications
Heart failure and pulmonary edema (fluid in lung tissue)
´Sepsis
´Acute respiratory failure
´Visceral damage (electrical burns)