Adequate rate control in a patient with AF is defined as:
a. Resting HR<80, maximal HR <110 during a 6-minute walk
b. Resting HR<60, maximal HR <110 during a 6-minute walk
c. Resting HR <80, maximal HR < 140 during a 6-minute walk
d. Resting HR <60, maximal HR < 140 during a 6-minute walk
e. Resting HR < 100, maximal HR < 140 during a 6-minute walk
Answer a.
Adequate rate control in patients with AF is defined as a resting HR <80 bpm and maximal HR <110 bpm during a 6-minute walk. Rate control can be achieved with a variety of medications. Digoxin alone is often insufficient to control HR during exercise.
Q65
Functional assessment of an intermediate coronary lesion can be performed by all of the following except:
a. Measurement of coronary flow reserve
b. Measurement of fractional flow reserve
c. Quantitative coronary angiography
Answer c.
Angiography only gives a visual estimate of stenosis and does not yield direct func-tional significance of an intermediate lesion
Q16
What percentage of heart failure patients have a normal EF?
a. 20%
b. 40% to 50%
c. 60%
d. 70%
Answer b.
Approximately half of the patients with heart failure have a normal EF. These patients are typically older, have a history of HTN, and are more often female. Morbidity and mortality is similar to those patients with HF EF. It is exceedingly difficult to dis tinguish patients with heart failure and reduced or normal EF based solely on clinical grounds. One needs additional testing, such as echocardiography or left heart catheterization, for hemodynamic assessment.
Q45
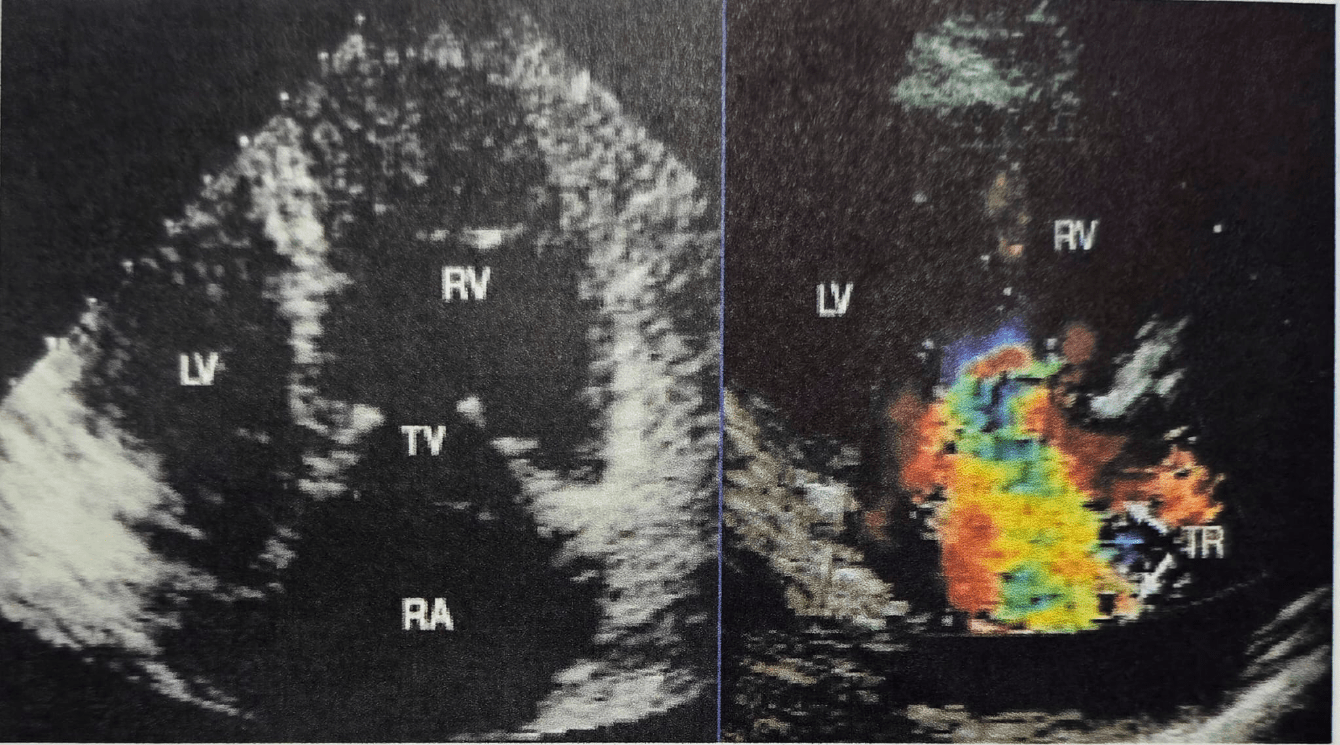 A 54-four-year old woman presents with a 6-month history of progressive symp-toms of right heart failure. On physical examination the JVP is 16cm with prominent V wave. There is also a loud holosystolic murmur with respiratory variation. The liver is enlarged and pulsatile. There is bilateral lower extremity edema and evidence of ascites.
A 54-four-year old woman presents with a 6-month history of progressive symp-toms of right heart failure. On physical examination the JVP is 16cm with prominent V wave. There is also a loud holosystolic murmur with respiratory variation. The liver is enlarged and pulsatile. There is bilateral lower extremity edema and evidence of ascites.
Upon reviewing her TTE, which is the next best diagnostic step
a. Coronary angiography and right heart catheterization
b. Urine cytology. c. Thyroid function studies
d. 5-HIAA. e. Blood cultures
Answer d.
The echocardiogram clearly shows thickened and retracted tricuspid leaflets. Color images and physical exam were consistent with severe TR. The valve leaflet morphol-ogy suggests a drug related (ie, erogotamines or diet drugs, which usually affect left valves more than right valves) or a systemic illness such as hypereosinophillia or car-cinoid. This illness seems to be targeting the right-sided valves; this is classically car-cinoid syndrome and the diagnosis can be clinched by measuring urinary 5-HIAA
Q9
All of the following are effects of loop diuretics, eg, furosemide, except which of the following?
a. Hypomagnesemia
b. Ototoxicity
c. Hypercalcemia
d. Venodilation
e. Loop diuretics are the most effective diuretic agents
Answer c.
Loop diuretics may cause hypocalcemia but not bypercalcemia. Early venodilatory effects of loop diuretics are likely prostaglandin-dependent.
Q13
Which of the following situations can result in SVT with a wide QRS in the absence of a preexisting or rate-related bundle branch block?
a. Orthodromic AVRT
b. Antidromic AVRT
c. Atypical AVNRT
d. Typical AVNRT
Answer b.
In antidromic AVRT, antegrade conduction is through an accessory pathway, with retrograde conduction through the AV node (anti-against the normal AV node con-duction). An important exception to other forms of SVT is that a bystander accessory pathway, not involved in the tachycardia, may conduct to the ventricle and cause pre-excited wide QRS
Q82
The major cell type of the normal coronary artery intima is the:
a. Macrophage
b. Smooth muscle cell
c. Lymphocyte
d. Endothelial cell
e. Foam cell
B
Q6
In which of the following scenarios is IV inotropic support most appropriate?
a. In acute hemodynamically unstable heart failure
b. In a patient awaiting transplantation who is hemodynamically unstable while receiving maximal oral therapy
c. As palliative therapy to allow dismissal of the patient with refractory heart failure receiving oral therapy who is not a candidate for transplantation or other surgical therapy
d. All of the above
Answer d.
IV inotropic support has a limited (and understudied) role in the management of heart failure. All the above scenarios represent appropriate and reimbursable uses of inotropic therapy.
Q49
What is the structure identified with an asterisk on this apical two chamber TTE performed for the evaluation of chest pain?
a. Dilated left lower pulmonary vein
b. IVC
c. Aneurysm of the LCX artery
d. Dilated CS
e. Left atrial appendage
Answer e.
The clip demonstrates a dilated left atrial appendage in the setting of a dilated LA, likely reflecting a chronic elevation in left atrial pressures.
Q1
Which antiarrhythmic agent is best employed to treat digoxin-induced rhythm disturbances?
a. Magnesium
b. Potassium
c. Lidocaine
d. Amiodarone
e. Quinidine
Answer c.
While antiarrhythmics, amiodarone and quinidine may both potentially exacerbate arrhythmias caused by digitalis toxicity.
Q56
The arrhythmic substrate least likely to be definitely ruled out with a negative EP study is:
1. Sinus node dysfunction
2. Severe His Purkinje disease
3. Accessory bypass tract
4. VT in a patient with cardiomyopathy
5. AVNRT
Answer : 1
The sensitivity of EP testing for sinus node disease is < 50%. For all other diagnosis listed, detection rates of EP tests are typically > 90%.
Q34
Which of the following factors is the most important in terms of reducing the incidence of late stent thrombosis with DESs?
a. Pretreatment with abciximab
b. Optimal stent deployment (complete apposition of stent with vessel wall)
c. The introduction of more potent antiplatelet agents (eg, ticlopidine, clopidogrel)
d. Aggressive anticoagulation with warfarin and aspirin
Answer b.
With the recent widespread implementation of DESs, late thrombosis data started appearing 1 yr after placement. In May, 2007, Cook et al. (Circulation 115:2426-2434) published an IVUS study on 13 patients with late stent thrombosis with a mean of 630 days 166 after DES implantation. They found incomplete stent apposition in 77% of these patients versus 12% of controls (IVUS done at 8 mos and no stent throm bosis > 2yrs post implant). Whether the incomplete apposition was due to technical limitation or the positive remodeling by local inflammation is unknown. They also found that patients with thrombosis had longer lesions, longer stents, more stents-per-lesion, and more stent overlap.
Q48
Which of the following is most accurate regarding current survival following cardiac transplantation?
a. One-year overall survival of 65% to 70%
b. Survival statistics are uniform from center-to-center
c. Highly dependent on recipient age
d. Posttransplant outcome is independent of donor heart ischemic time
Answer c.
National average data demonstrate that the one-year overall survival is 85%, but results are variable from center to center. Posttransplant survival is worse in the elderly population (thus cardiac transplantation is an absolute contraindication if age ≥70 years) and if the donor heart ischemic time is prolonged (ie, >240 minutes).
Q22
An elevation in which pressure is most likely to be associated with pulmonary congestion and clinical symptoms?
a. LA mean pressure
b. LV developed pressure
c. LA A-wave pressure
d. LVEDP
c. PA mean pressure
Answer a.
Pulmonary congestion correlates best with mean LA pressure. An elevation in LVEDP is frequently associated with an elevation in mean LA pressure, however would not be associated with pulmonary congestion in the absence of elevation in LA pressure.
Q11
Hepatic clearance is important for all of the following, except:
a. Sotalol
b. Propranolol
c. Metoprolol
d. Labetalol
e. Amiodarone
Answer a.
Sotalol is cleared renally and hence should be used with extreme caution when there is the potential for renal insufficiency.
Q58
Pacemaker syndrome is a hemodynamic abnormality that results from which of the following abnormalities?
a. The delay between the right and LV pacing leads is too long to allow a syn-chronous contraction
b. Ventricular pacing is uncoupled from the atrial contraction
c. Cross talk that results in inappropriate inhibition of the pacing stimulus
d. Endless-loop tachycardia that results from retrograde P waves that trigger another ventricular stimulation
Answer b.
Pacemaker syndrome results from inappropriate ventricular pacing or when the ventricular pacing is uncoupled from the atrial contraction. Patients may experience a variety of symptoms that include general malaise, a sensation of fullness in the head and neck, syncope, cough, dyspnea, heart failure, or weakness. They may have cannon A waves on exam and a lower BP when paced. The syndrome is most common when the VVI mode is used and the underlying rhythm is sinus.
Q113
Rotational atherectomy is contraindicated in which settings:
a. Bifurcation lesions
b. Saphenous vein grafts
c. Heavily calcified lesions
d. Insulin-dependent diabetes
Answer b.
Because of the higher likelihood of a saphenous vein graft to contain thrombus and subsequent microembolization with no reflow, this is considered to be a contraindication to rotational atherectomy. The location of a vein graft can make perforation particularly catastrophic as well. Debulking heavily calcified lesions prior to stent deployment is a useful application of rotational atherectomy.
Q28
Administration of recombinant BNP to a patient with heart failure should result in which one of the following changes?
a. Natriuresis
b. Reduced filling pressures
c. Decreased CO
d. a, b, and c
e. a and b
Answer c.
Administration of recombinant BNP (ie, Nesiritide) to patients with heart failure has been well studied. While the natriuretic response to natriuretic peptide infusion is blunted in patients with heart failure as compared to control subjects, the natri-uretic peptides are still natriuretic when administered to patients with heart failure. They have potent effects on venous capacitance, resulting in reduction in venous return and reduced filling pressures. Administration of natriuretic peptides to normal subjects results in decreases in CO (mediated by the decrease in venous return) and reflex increases in systemic vascular resistance. However, in heart failure patients, administration of natriuretic peptides decreases systemic vascular resistance and increases CO.
Q23
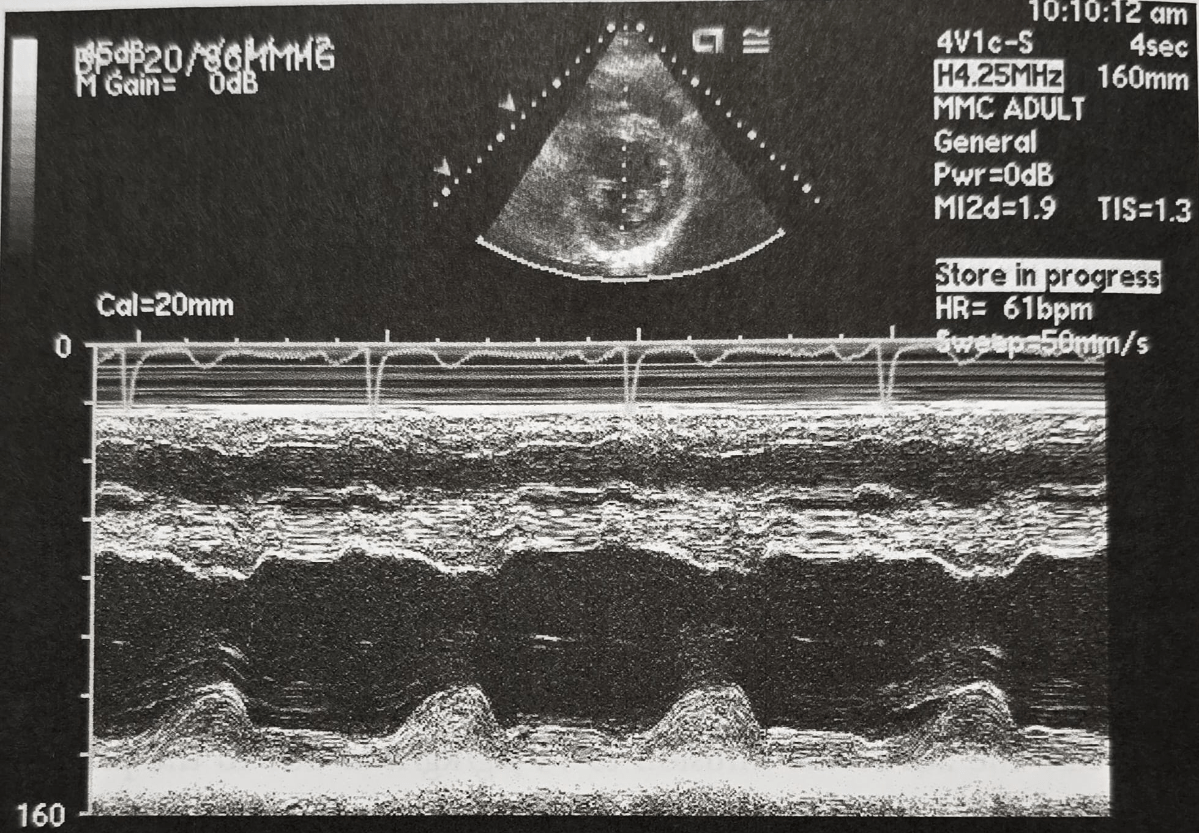 A 45-year-old male with fatigue presents for an echocardiogram. The LV end diastolic dimension is 60mm and the end systolic dimension is 40 mm. What is the EF?
A 45-year-old male with fatigue presents for an echocardiogram. The LV end diastolic dimension is 60mm and the end systolic dimension is 40 mm. What is the EF?
a. 56%. b. 33%. c. 67%. d. 45%. e. 50%
56%. Where LVEDD LV end diastolic diameter, and LVESD LV end systolic diameter, LV EF by M-mode is calculated by:
LV EF = [(LVEDD)² - (LVESD)²]/(LVEDD) × 100
Here LV EF = [(60)2(40)]/(60) × 100 = 56%
Q8
n a patient on warfarin, amiodarone is initiated for AF. You will need to:
a. Increase the amiodarone dose by 50%
b. Increase the warfarin dose by 50%
c. Follow prothrombin time and adjust warfarin dosage
d. Switch warfarin to aspirin
e. Decrease amiodarone dose by 50%
Answer c.
Typically, warfarin doses need to be decreased between 25% and 50% after starting amiodarone, although the response is variable.
Q85
All of the following are contraindications for use of Ibutilide to chemically ter-minate atrial flutter with rapid ventricular rates except:
a. A prolonged QT interval
b. A history of polymorphic VT with class 1 or 3 antiarrhythmic drugs
c. Severe hypokalemia
d. Hemodynamic instability
e. Structural heart disease
Answer c.
Patients with prolonged QT and a history of polymorphic VT with class I or III antiarrhythmic agents should not received ibutilide due to an increased risk of tor-sades de pointes. Likewise, significant hypokalemia can increase the risk of torsades de pointes. In patients with hemodynamic instability, emergency DC cardioversion is necessary. Patients with a structurally normal heart have a very low risk of torsades de pointes (1%) although lack of a normal heart in itself is not a contraindication (risk of torsades de pointes up to 4%).
Q76
Of the three major CABG versus medical therapy trials, which of the following showed an overall survival benefit for CABG?
a. CASS
b. ECSS
c. VA multicenter study
Answer b.
The ECSS trial was published in 1980 and studied 768 patients. The surgical arm, however, actually had better compliance with beta blocker therapy than the medical therapy arm. It could be considered a "surgery versus no surgery" trial. The 5-yr sur-vival was 93% for CABG and 84% without. The VA multicenter study was published in 1977 and did not show an overall survival benefit. There was improved survival (87% vs. 74%) in patients with left main disease
Q53
Which one of the following patients with heart failure would be expected to derive the greatest benefit from cardiac transplantation?
a. 45-year-old man with an EF of 18%, peak oxygen uptake (VO2max) of 16 mL/kg/min, and BNP level of 1,650 pg/mL
b. 59-year-old woman with an EF of 30%, VO2max of 10 mL/kg/min, and BNP of 650 pg/mL
c. 49-year-old woman with an EF of 20%, VO2max of 14 mL/kg/min, and BNP of 1,200 pg/mL
d. 77-year-old man with an EF of 15%, VO2max of 10 mL/kg/min, and BNP of 1,800 pg/mL
Answer b.
The peak oxygen uptake (VO2max) remains the single best predictor for transplanta-tion benefit and need. In general, if patients value have under 14 mL/kg/min, they are good transplant candidates. However, recent data suggest that those patients with severely reduced exercise capacity (VO2max ≤10 mL/kg/min) derive even greater benefit and thus answer b is correct. EF and BNP level provide less accurate predic-tive assessment. Answer d is incorrect since this patient's age (age > 70 years) excludes him from being an acceptable transplant candidate.
Q24
Which of the following mitral annular velocities suggests constrictive pericarditis?
a. 5 cm/sec
b. 7 cm/sec
c. 15 cm/sec
d. 50 cm/sec
e. 1 m/sec
Answer c.
An elevated/high normal velocity of the mitral annulus is typical for patients with con-strictive pericarditis. Velocities greater than 20 cm/sec are not seen in adult patients.
Q25
Which of the following drugs used at therapeutic levels is most likely to increase the pacing threshold?
a. Amiodarone
b. Flecainide
c. Sotalol
d. Procainamide
e. Digoxin
Answer b
Drugs that block sodium channels increase the pacing threshold, whereas potassium channel blockers decrease them.
Q22