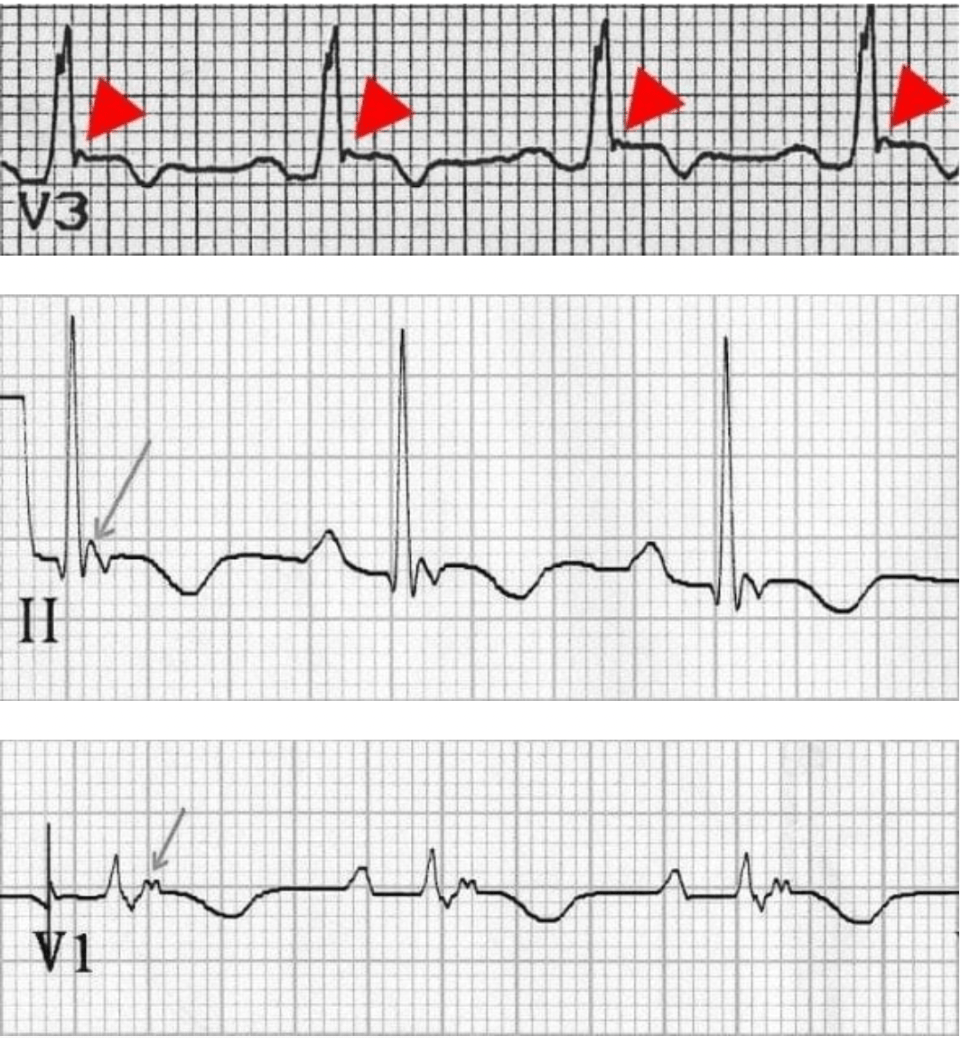
A healthy 3 week old presents with fussiness. This is his EKG. This is his diagnosis.
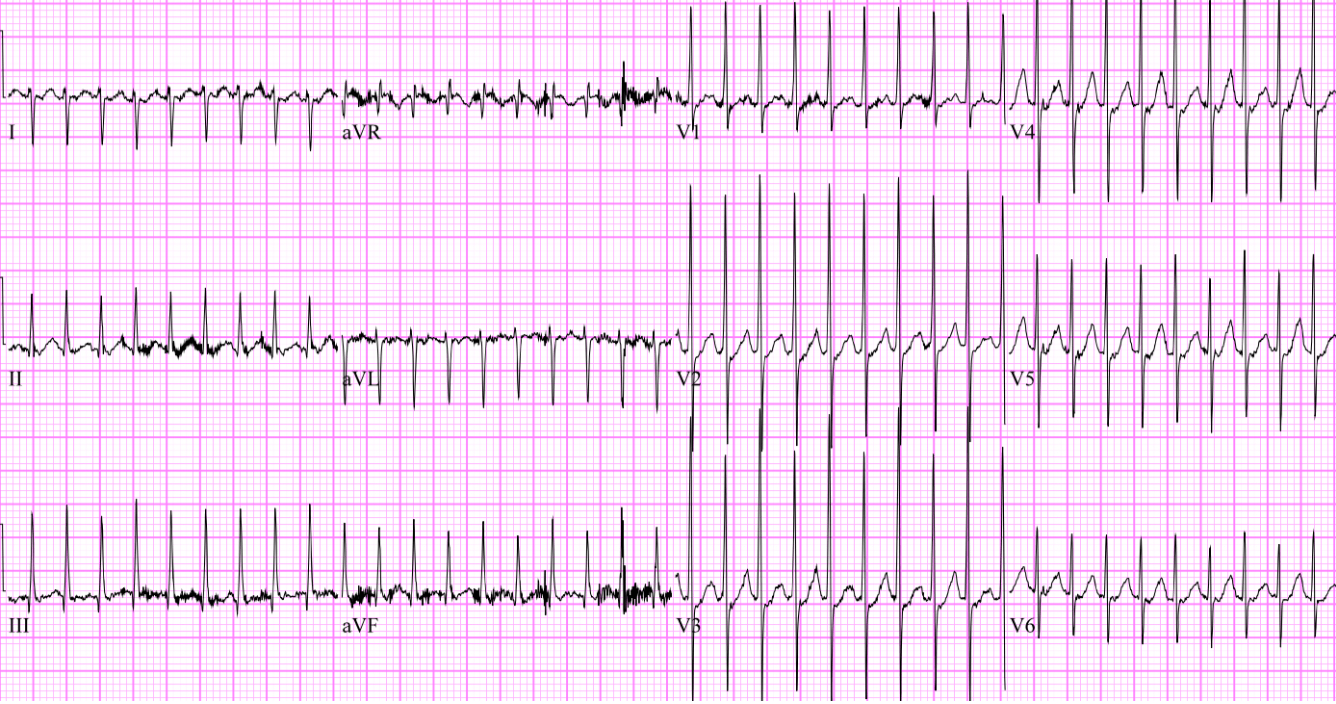
What is supraventricular tachycardia (SVT) ?
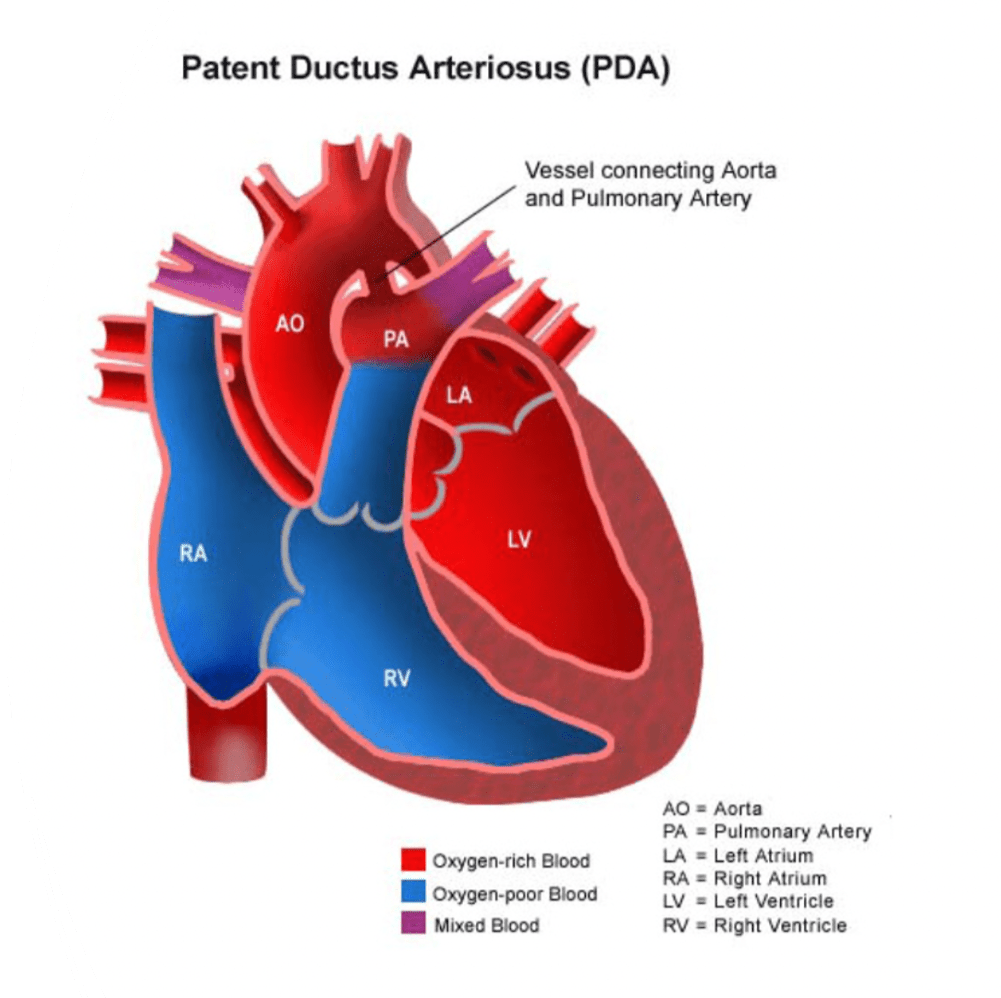
This is the age that PDAs close (functionally) in full-term healthy babies. In addition, this is the typical age that PDAs permanently close in term babies.
Functional closure within 24 hours and permanent closure within 2-3 weeks of life (this happens later in pre-term babies.)
A 13-year-old previously healthy boy presents with intermittent episodes of sharp, stabbing chest pain over the left precordium. The pain lasts for a few seconds to a couple of minutes, occurs at rest, and is not associated with exertion, shortness of breath, palpitations, or syncope. He says the pain worsens with deep inspiration and resolves spontaneously. Physical exam and vitals are normal. ECG is unremarkable. This is the diagnosis.
What is precordial catch syndrome?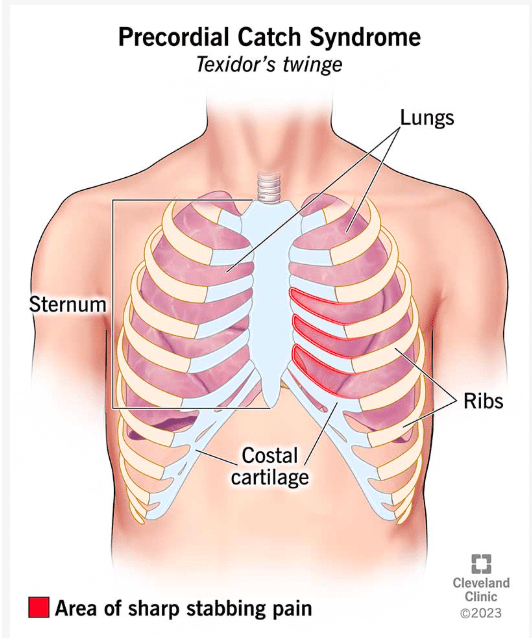
Strong emotions, such as anger, surprise, or excitement, can trigger syncope in individuals with this inherited cardiac condition.
Congenital prolonged QT syndrome
This is the recommended epinephrine dosing in patients in cardiac arrest, including the maximum dose.
0.01mg/kg with a max dose of 1mg.
(patients max out if they are 100kg or 220lbs.)
This is the most common EKG finding in patients with pulmonary embolism.
Sinus tachycardia
This diagnosis is in a 10 year old with chest pain.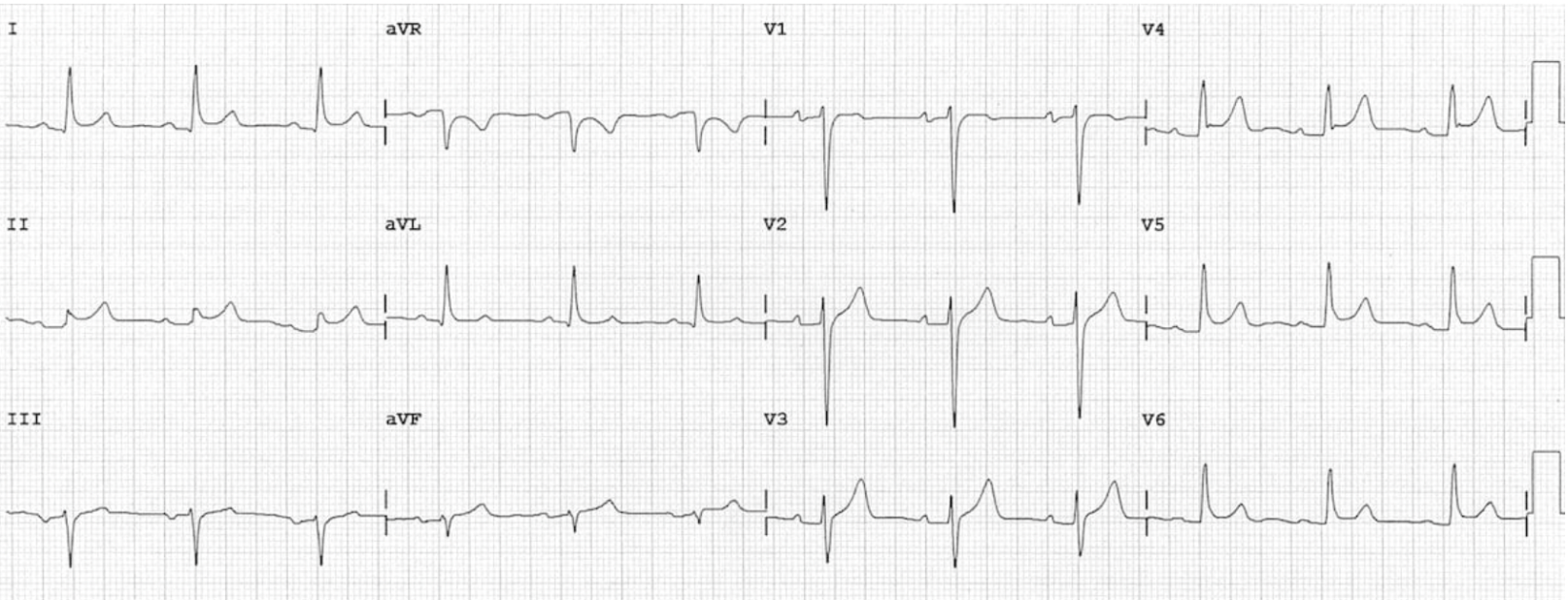
What is pericarditis?
- Widespread concave ST elevation and PR depression is present throughout the precordial (V2-6) and limb leads (I, II, aVL, aVF).
- There is reciprocal ST depression and PR elevation in aVR.
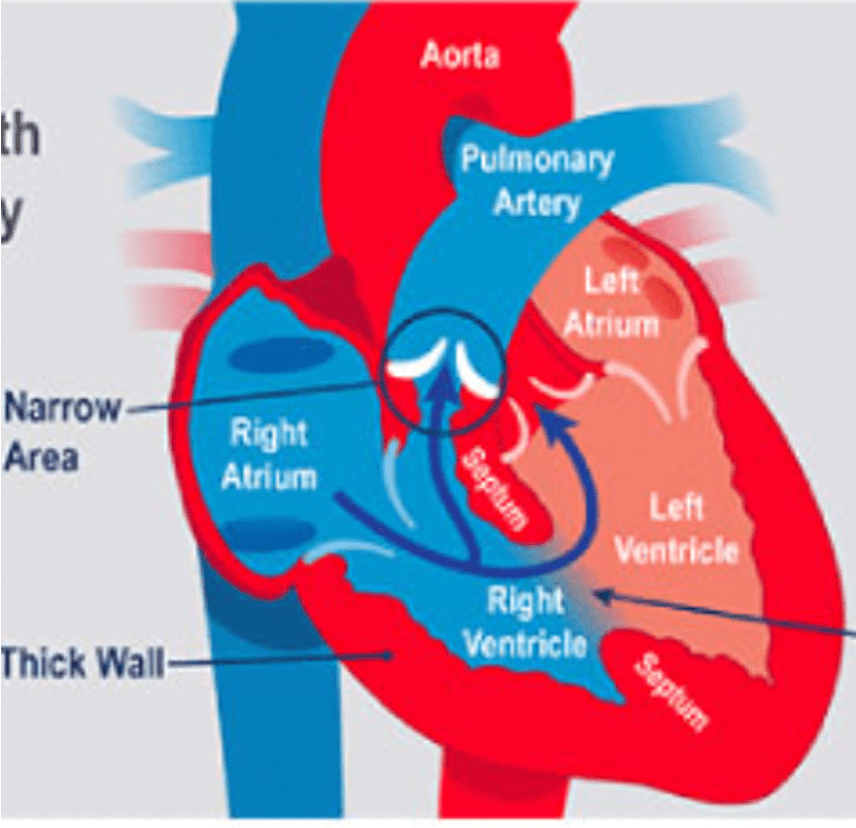
An 8 month old with trisomy 21 is in the ED and is crying and cyanotic. Mom knows of a history "hole in the heart" and cyanotic episodes in the patient. This is the best next step in management.
Knees-to-chest maneuver. You want to increase SVR to help shunt blood from systemic circulation (left-side of heart) into pulmonary circulation (right side of heart.) oxygen is a helpful tool for vasodilation. Morphine, versed fentanyl, or other medications for pain are also helpful. Can also give fluid as these patients are pre-load dependent.
Most common cause of chest pain in pediatrics.
What is musculoskeletal pain?
This patient syncopized prior to arrival. She has some suicidal ideation and unclear history. Below is her EKG. This is her diagnosis.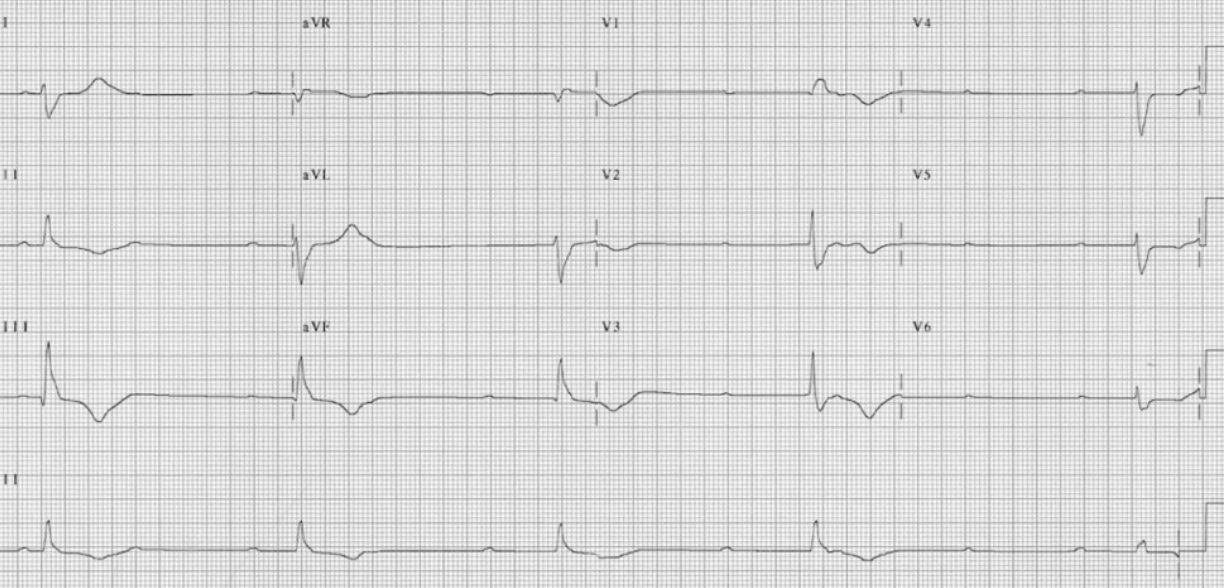
Third-degree heart block. Beware in calcium channel blocker and beta blocker ingestions.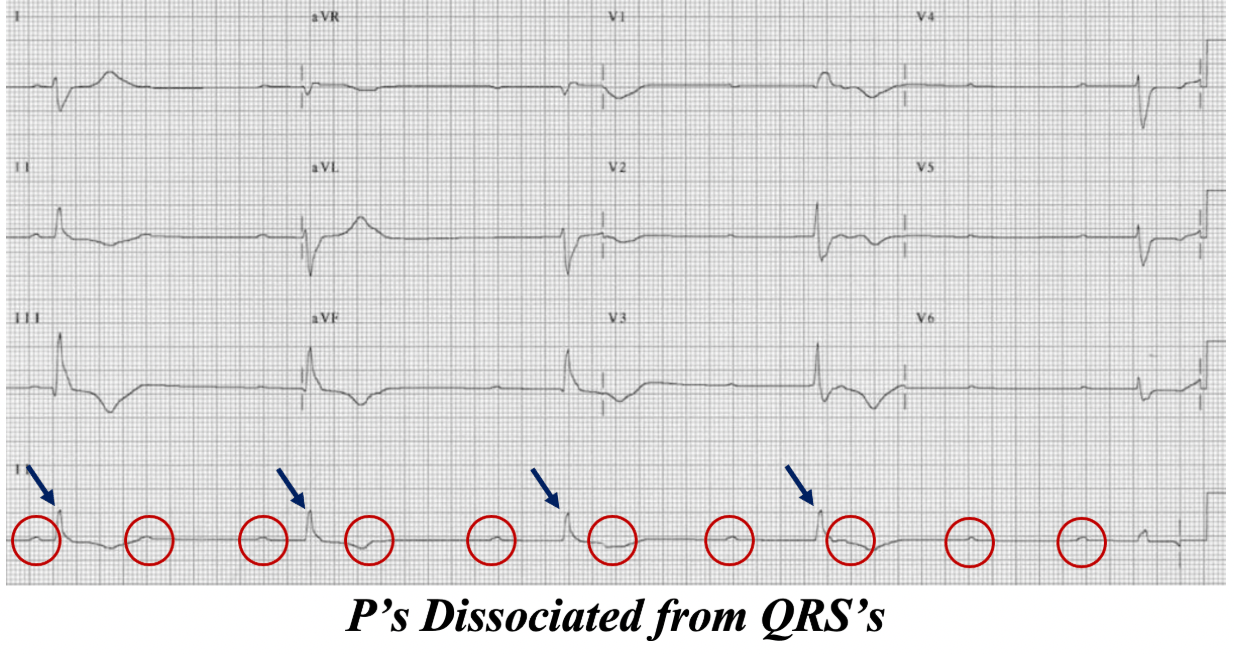
Per the cardiac arrest algorithm, these are the two shockable rhythms.
What is ventricular fibrillation and V-tach WITHOUT a pulse?
Cutoff for prolonged QT in boys/girls (teens.)
> 450msec
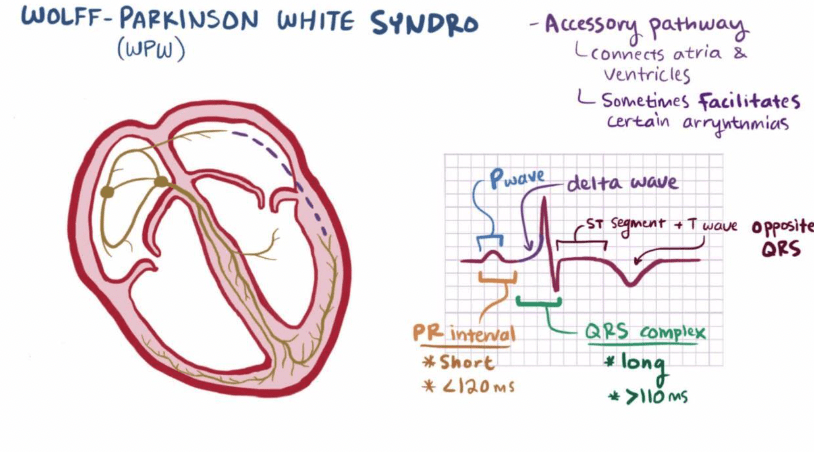
These are 3 EKG findings that are specific for the diagnosis below (you must name at least two.)
Wolff-Parkinson-White Syndrome
- Delta wave
- Shortened PR interval
- Prolonged QRS
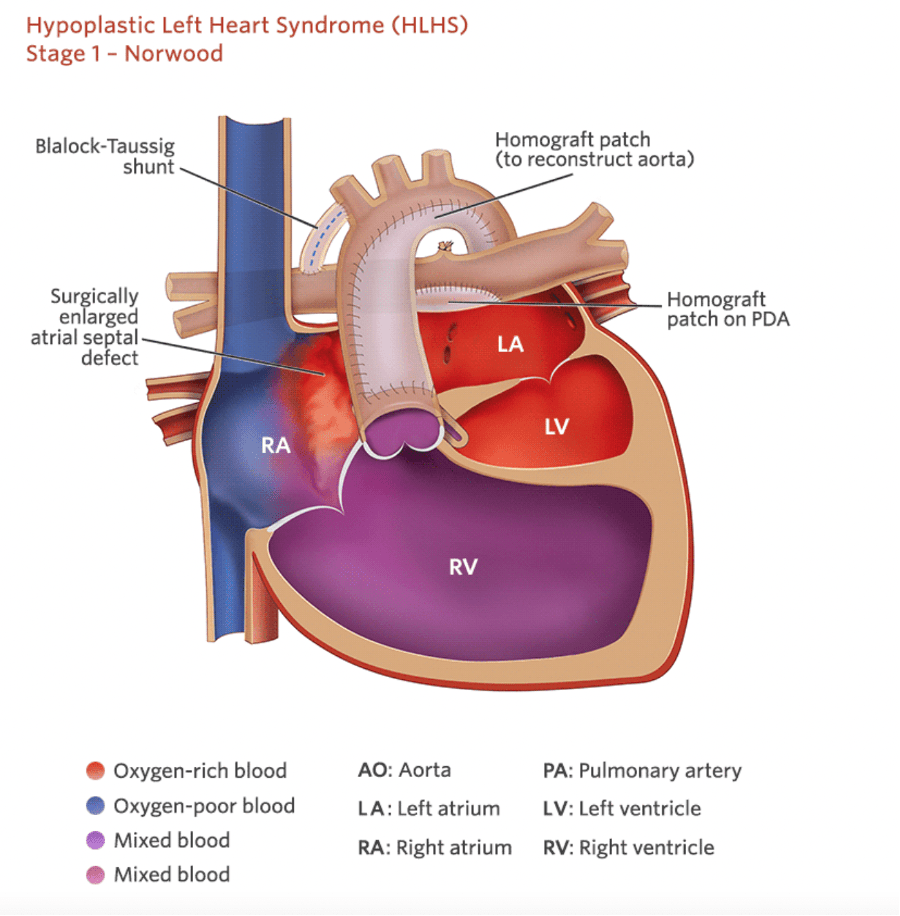
Patient has a history of HLHS s/p Norwood/Sano. This is the reason that we do not want her oxygen saturations greater than 85%.
Ovarsaturation in patients following Norwood/Sano (stage 1) of palliation are at risk of pulmonary over-circulation due to dilation of pulmonary vasculature induced by oxygen. This can cause inadequate blood-flow in systemic circulation.
Patient has had fatigue and chest pain over the last 2 days. Had a cold one week ago. Has a gallop on exam. This is the most sensitive EKG finding for this diagnosis.
Sinus tachycardia which is still only present in 46 - 58% of EKGs. Other findings include:
- Non-specific ST-T wave changes (next most common)
-ST segment elevation or depression
- T-wave inversions
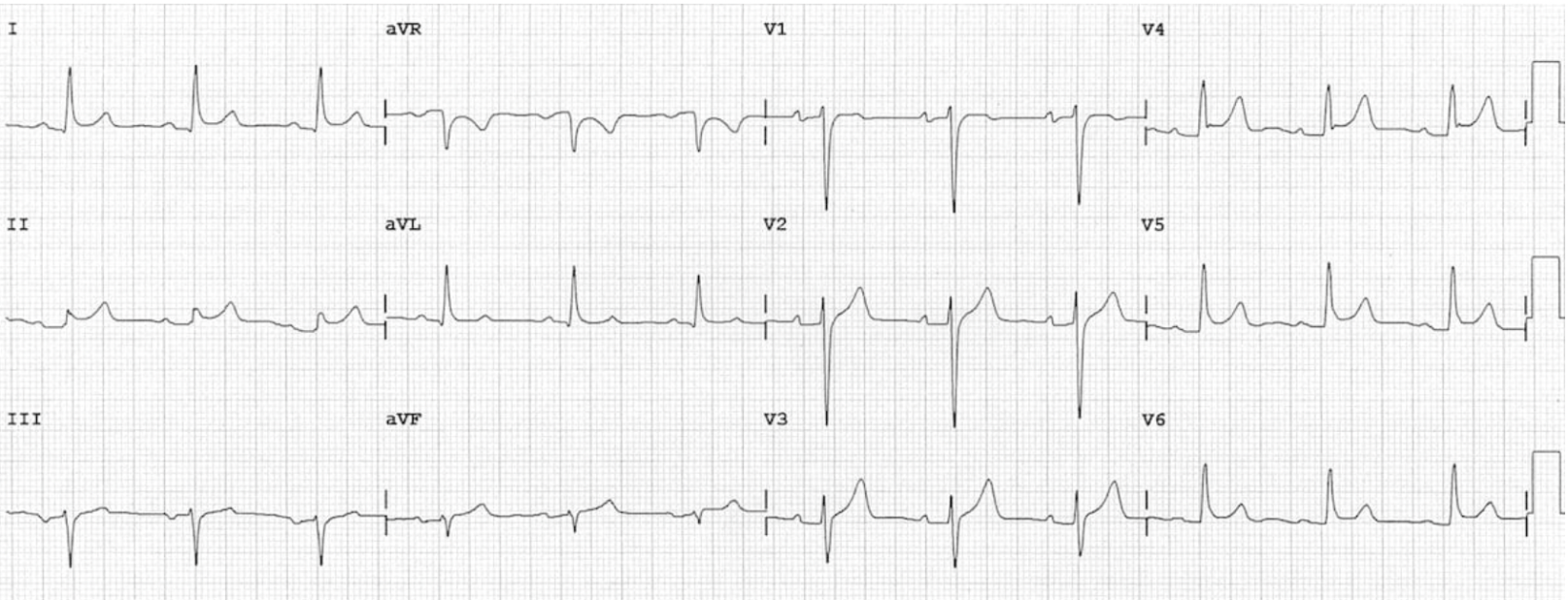
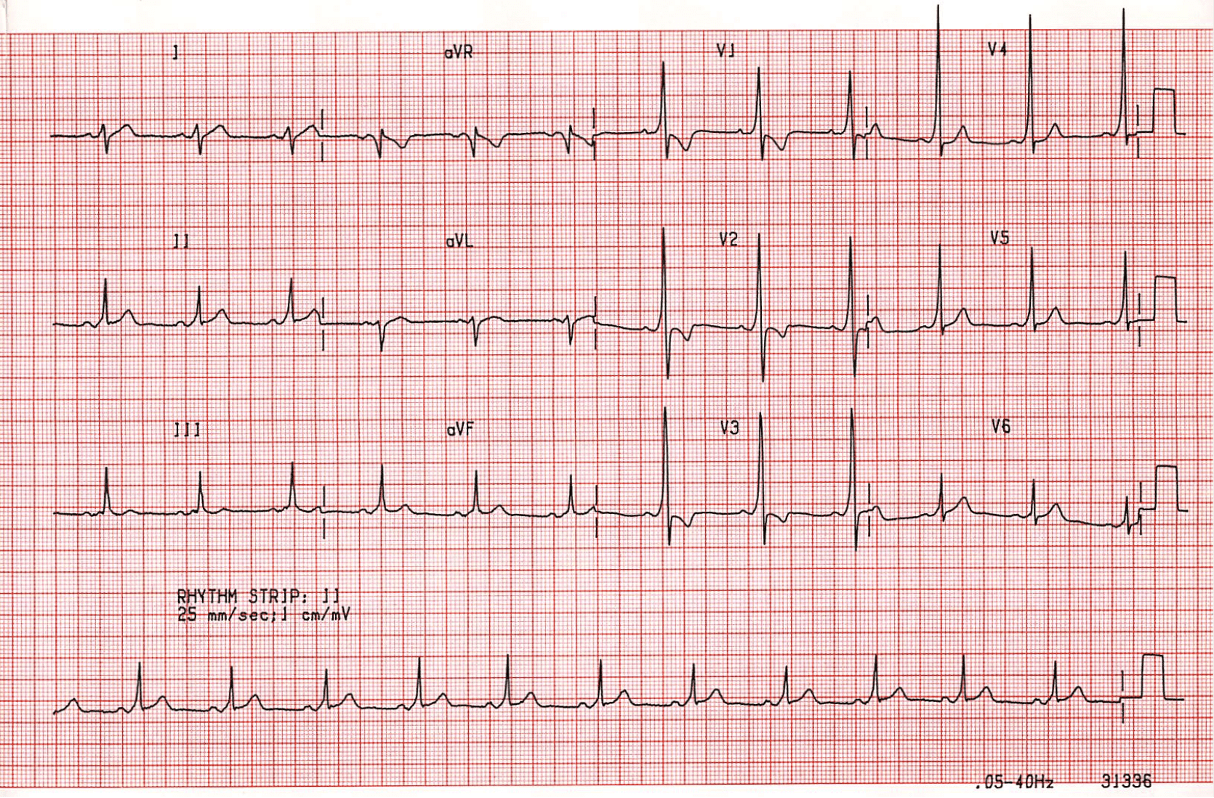
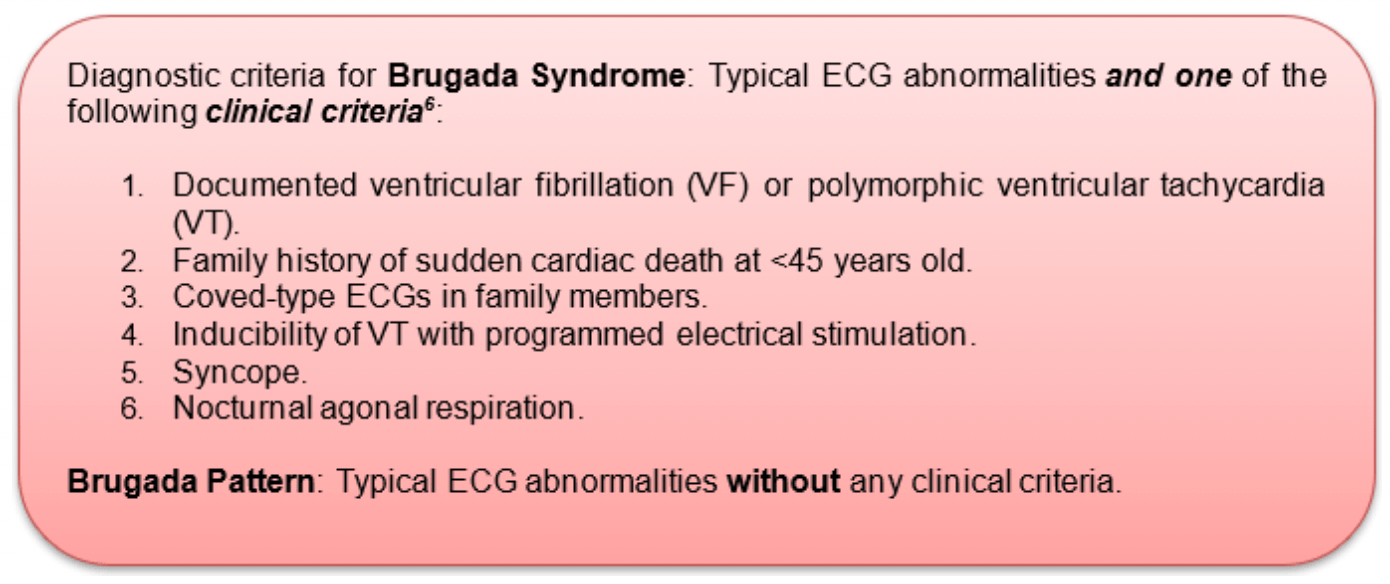
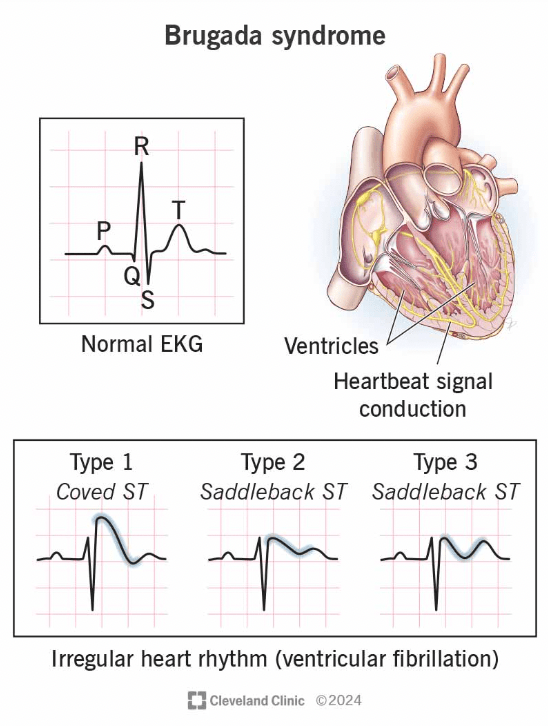
This patient presents for a syncopal episode. This is the diagnosis.
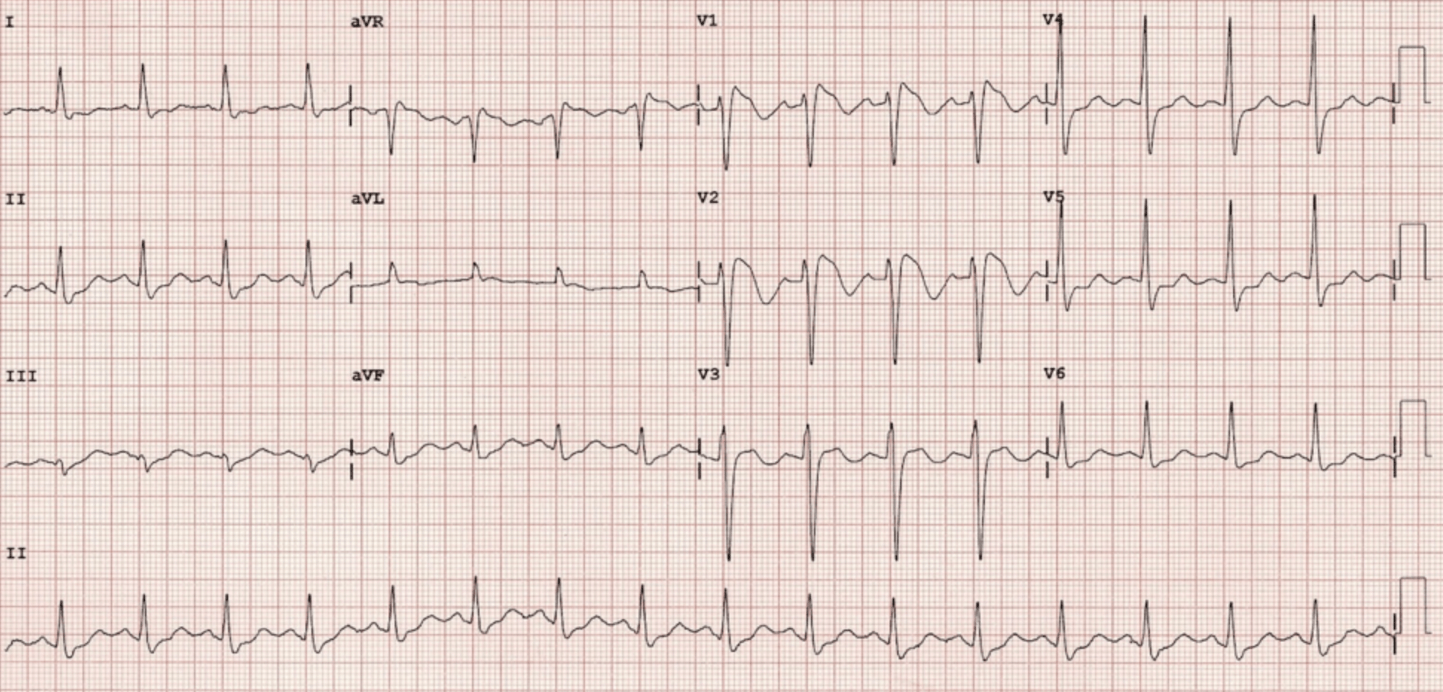
What is Brugada Syndrome?
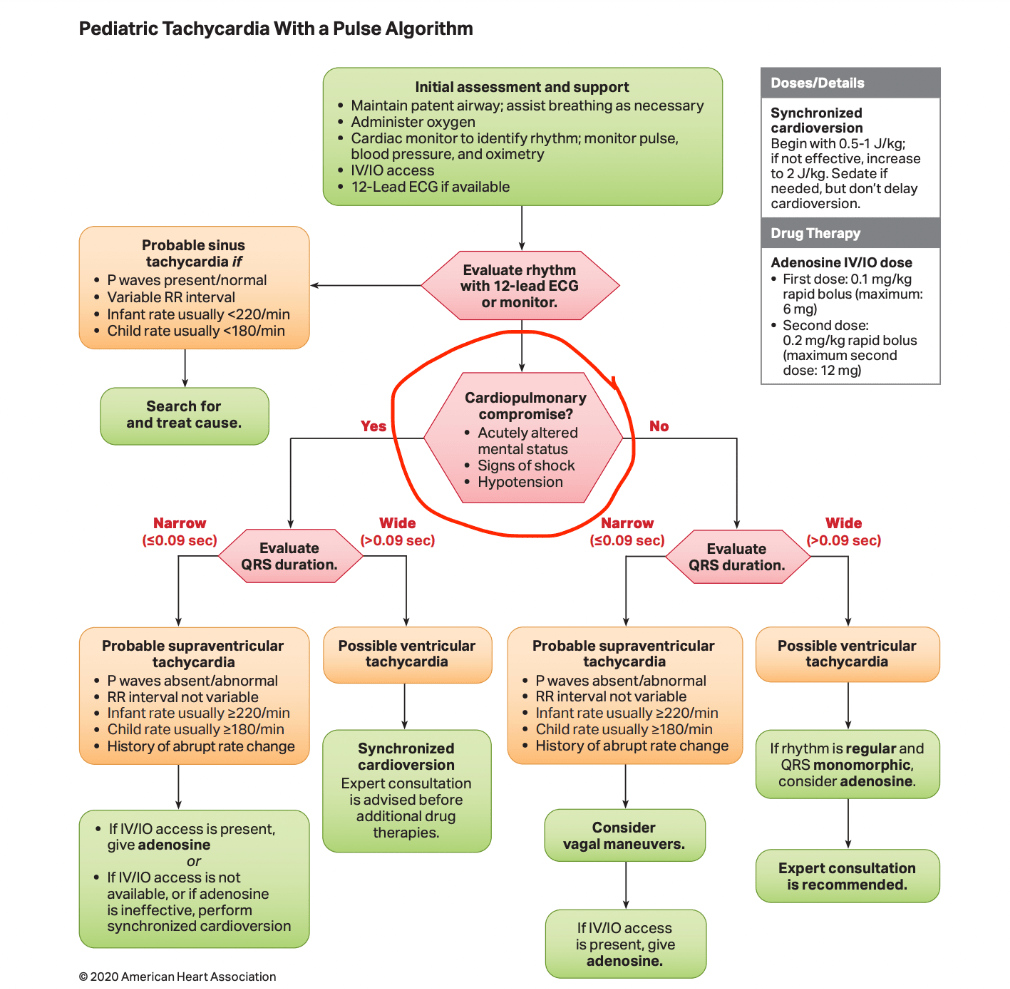
Your patient is a 6 year old with a heart rate of 200 that is unchanged with activity. You cannot visualize p waves. These are 3 things about the patient’s examination that you need to know to determine the best next step in management (AKA how you know if someone is hemodynamically stable.)
Altered mental status?
Hypotension?
Signs of shock?
This is the pathophysiology of WPW.
Accessory pathway is present connecting the atria to the ventricles leading to pre-excitation pf the ventricles. It bypasses the AV node.
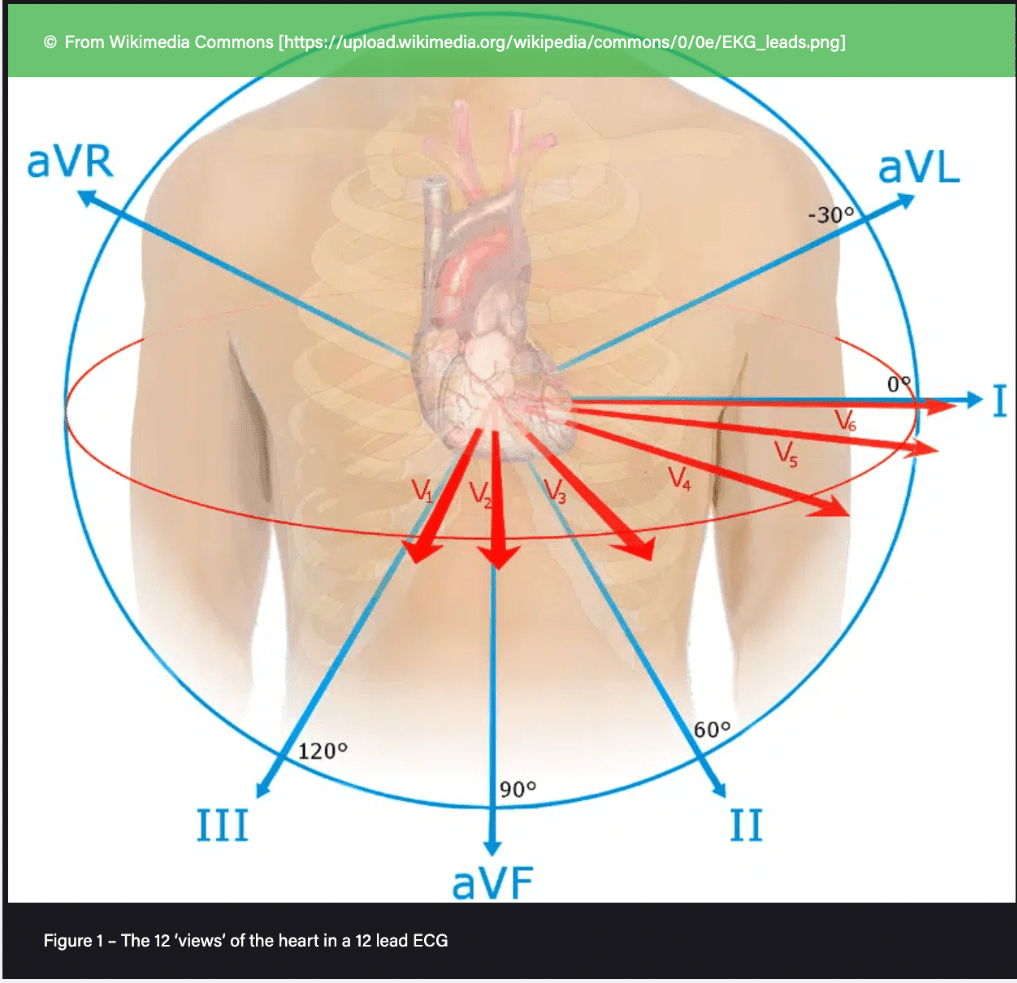
These are the anterior/septal leads, the precordial, the inferior leads, and the lateral leads respectively.
septal / anterior leads: V1 - V4
inferior leads: II, III, aVF
lateral leads: I, aVL, V5- V6
Full-term baby was born at home and EMS was called because she is cyanotic Sat 35% on RA. STarted on NRBR. This is the best next step in treatment.
Prostaglandin drip, 0.05mc/kg/min. Cyanosis with signs of heart faiure right after birth --> ductal dependent lesion.
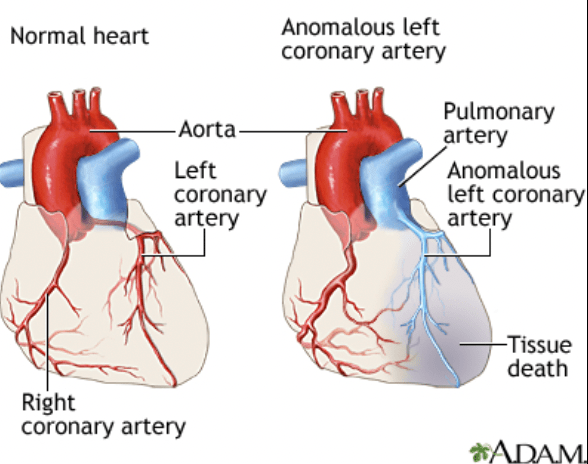
A 7-year-old boy presents with intermittent chest pain that occurs during physical activity. He says the pain is a "tight feeling" in the center of his chest and is occasionally accompanied by shortness of breath and fatigue. His parents report that he gets tired faster than his peers and has had a few episodes of dizziness after running. There is no family history of cardiac disease or sudden death. On exam, he is well-appearing, with normal vitals and a soft systolic murmur at the apex. ECG shows deep Q waves in leads I and aVL, and chest X-ray shows mild cardiomegaly.
Anomalous Left Coronary Artery from the Pulmonary Artery (ALCAPA)
ALCAPA is a rare but critical congenital coronary anomaly. The left coronary artery arises from the pulmonary artery instead of the aorta, leading to:
Myocardial ischemia, especially under stress/exercise
May present in infancy with heart failure (early form)
But some kids survive to school age or later with collateral formation
Classic signs in older kids:
Exertional chest pain
Fatigue, dizziness, or syncope with activity
Abnormal ECG: deep Q waves in I, aVL, V5–V6 due to chronic ischemia
Cardiomegaly on CXR, maybe MR from papillary muscle dysfunction
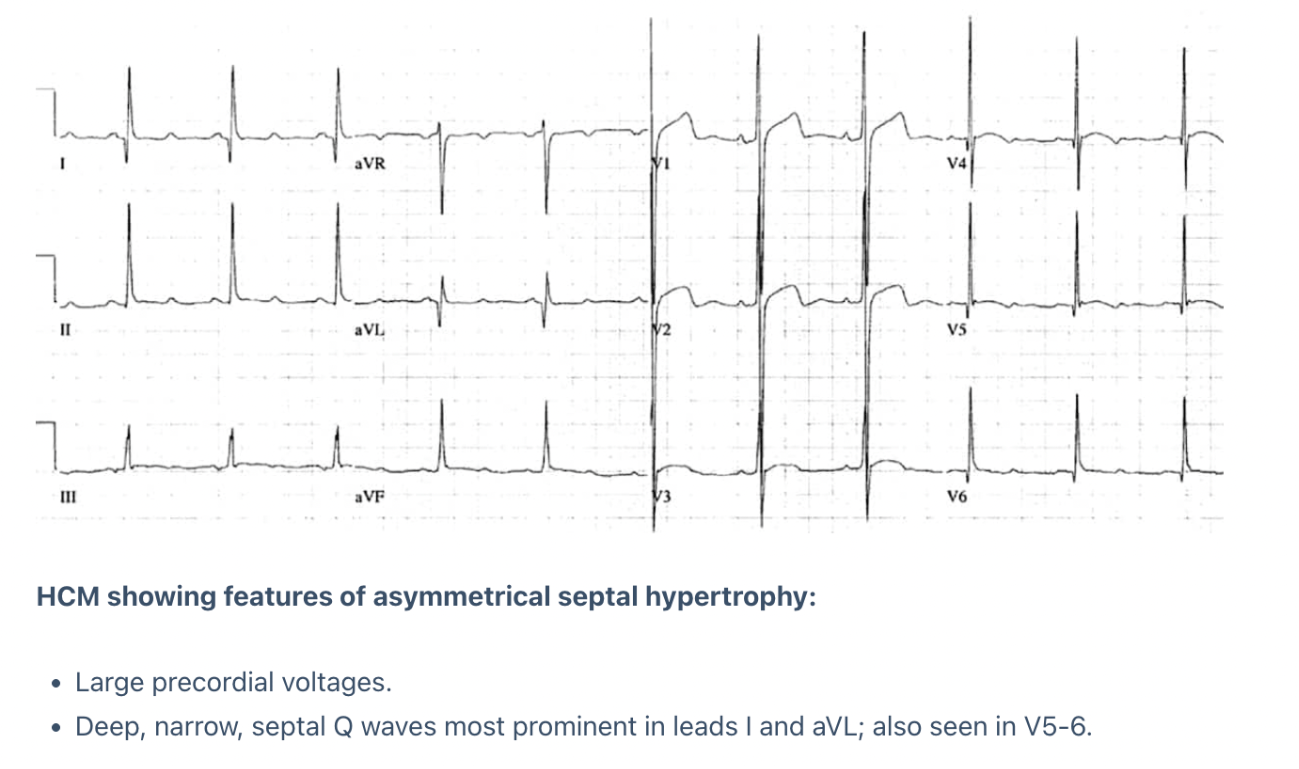
These 2 EKG findings clinch the diagnosis below.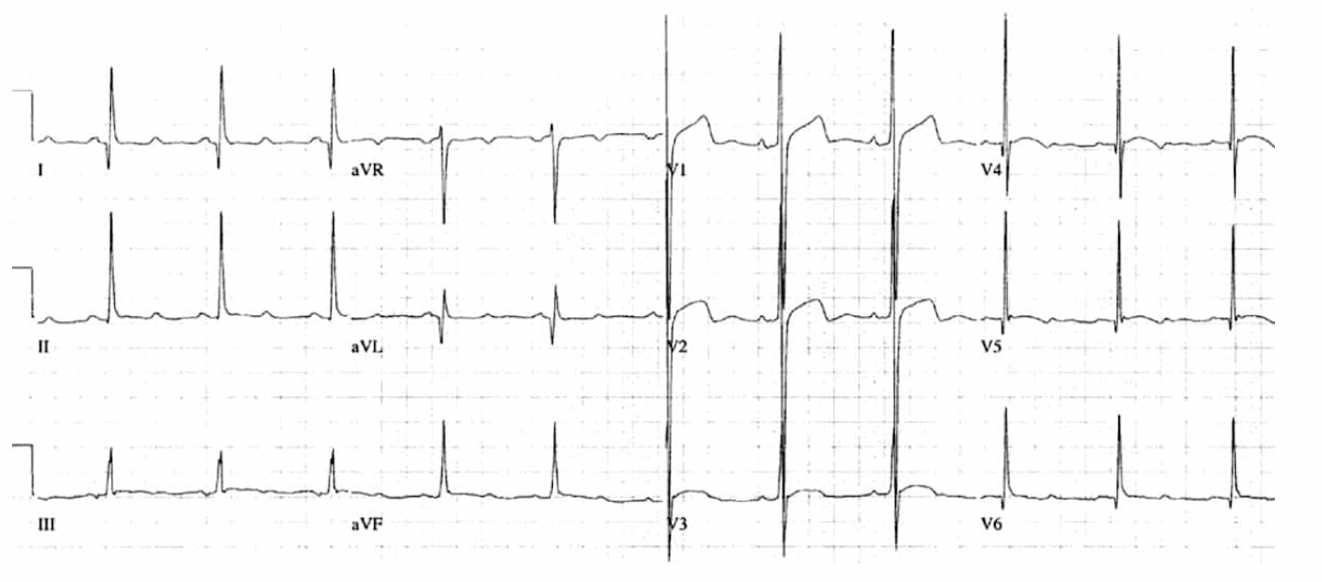
Increased voltages in precordial leads
Deep and narrow "dagger-like" Q waves, < 40msec (< 1 tiny box)
 Number one cause of sudden cardiac death in young people.
Number one cause of sudden cardiac death in young people.
16 year old poly-ingestion presents to the ED. This is her EKG. Blood pressure is 97/60. She is protecting her airway with a pulse but not at her neurologic baseline. This is the diagnosis AND the best next step.
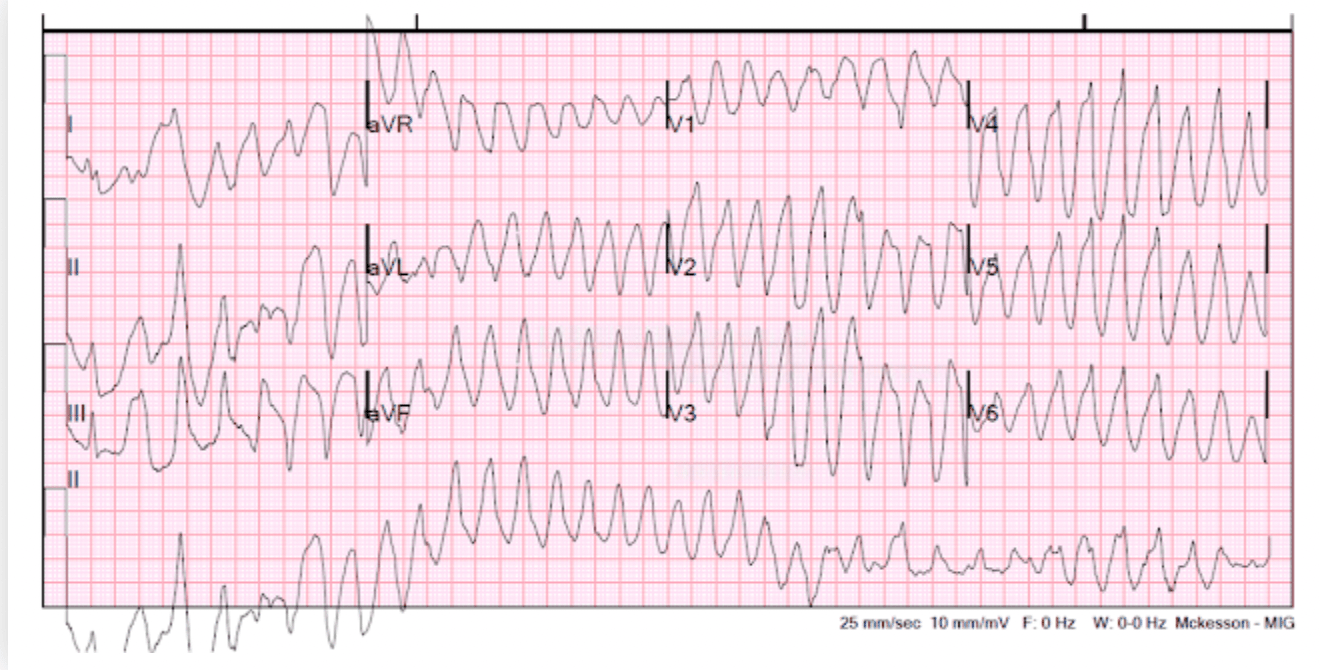
Polymorphic ventricular tachycardia
Synchronized cardioversion since patient is unstable
Start at 0.5-1 joules/kg and increase to 2 joules / kg if first dose is ineffective.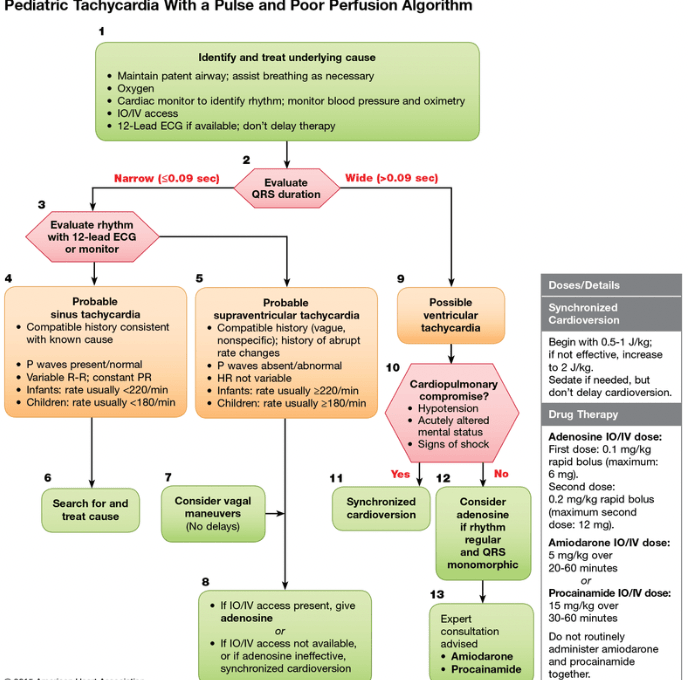
PR elevation in this specific lead can indicate pericarditis.
aVR - indicates right atrial inflammation
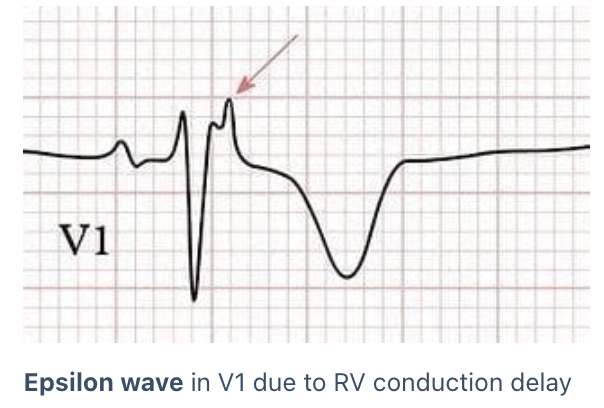
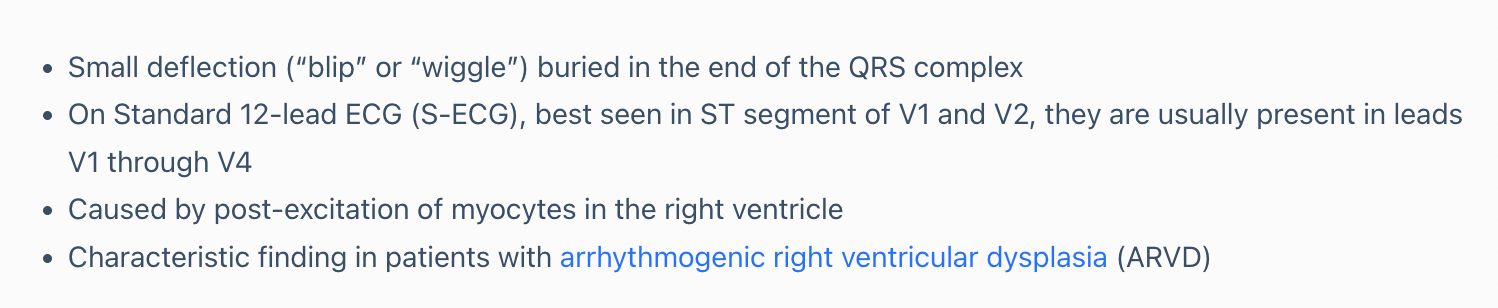
This EKG finding is most specific for a condition that's pathophysiology involves cardiac myocytes that are replaced by fat.
Epsilon waves
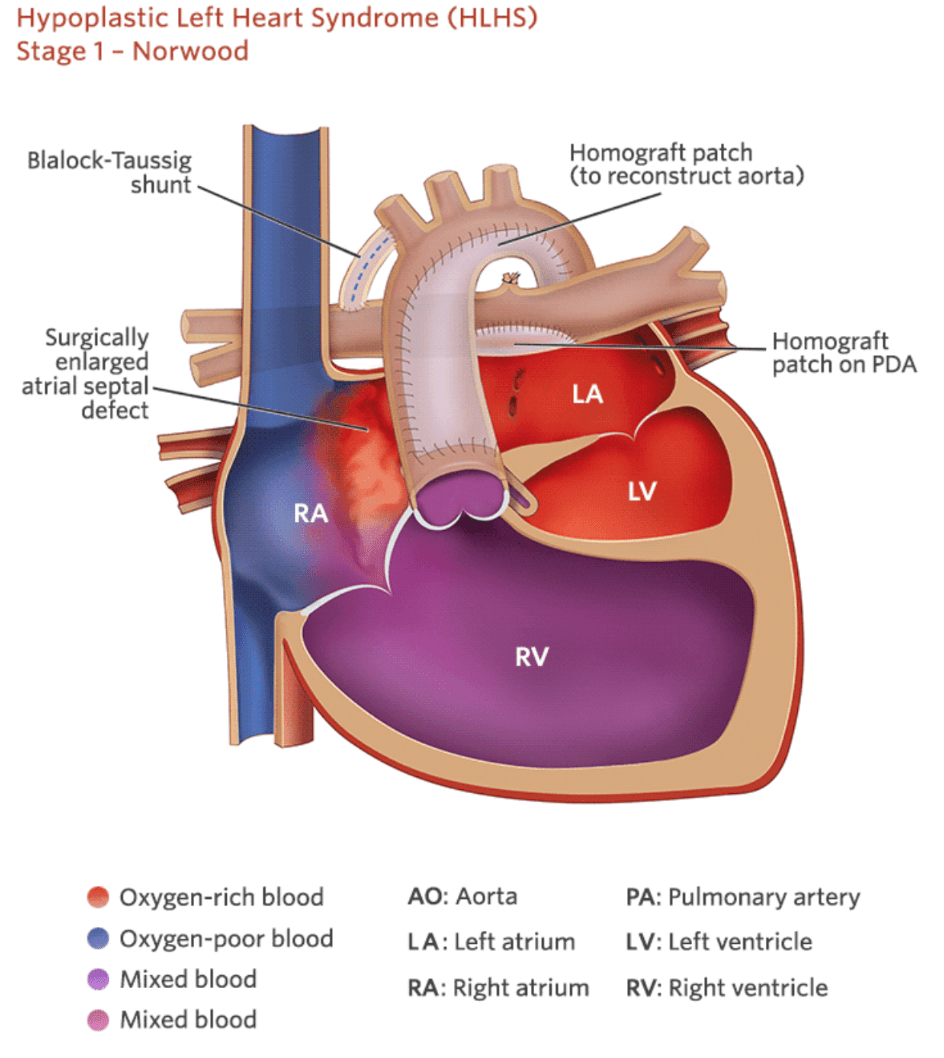
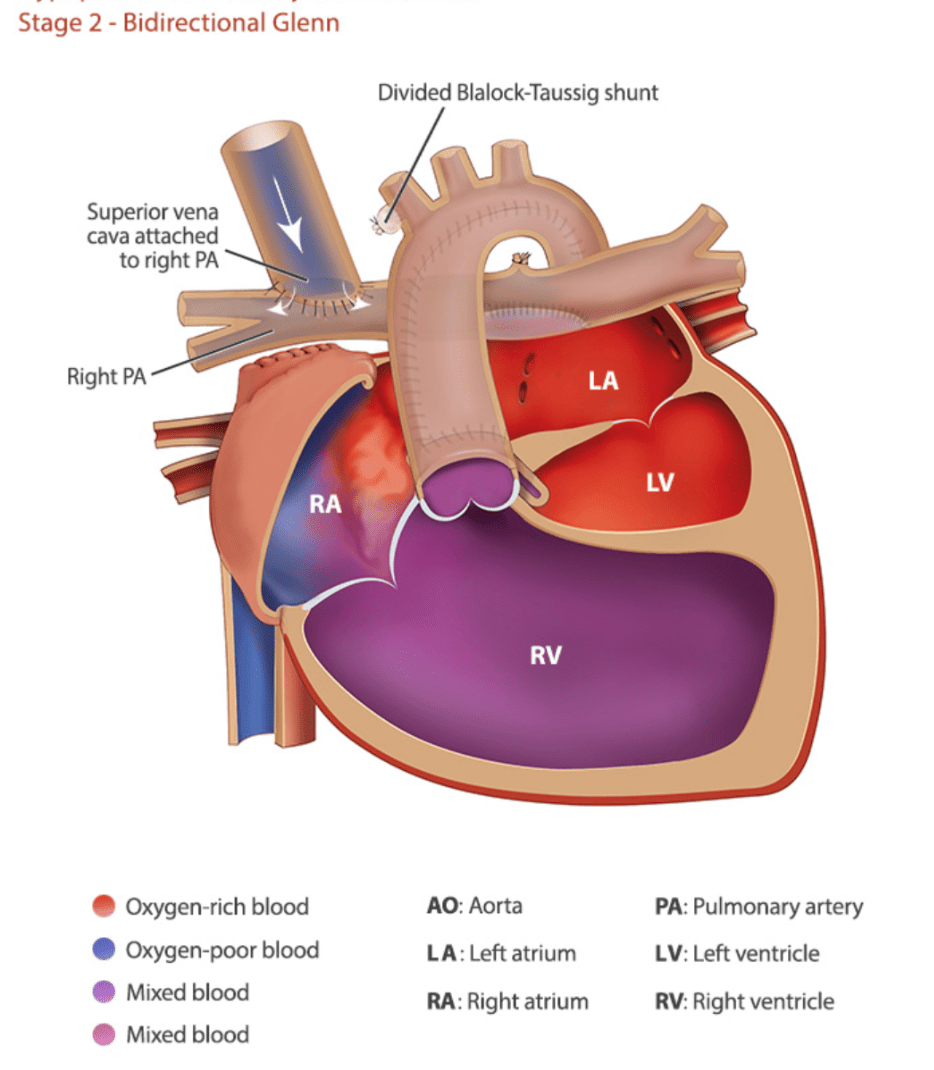
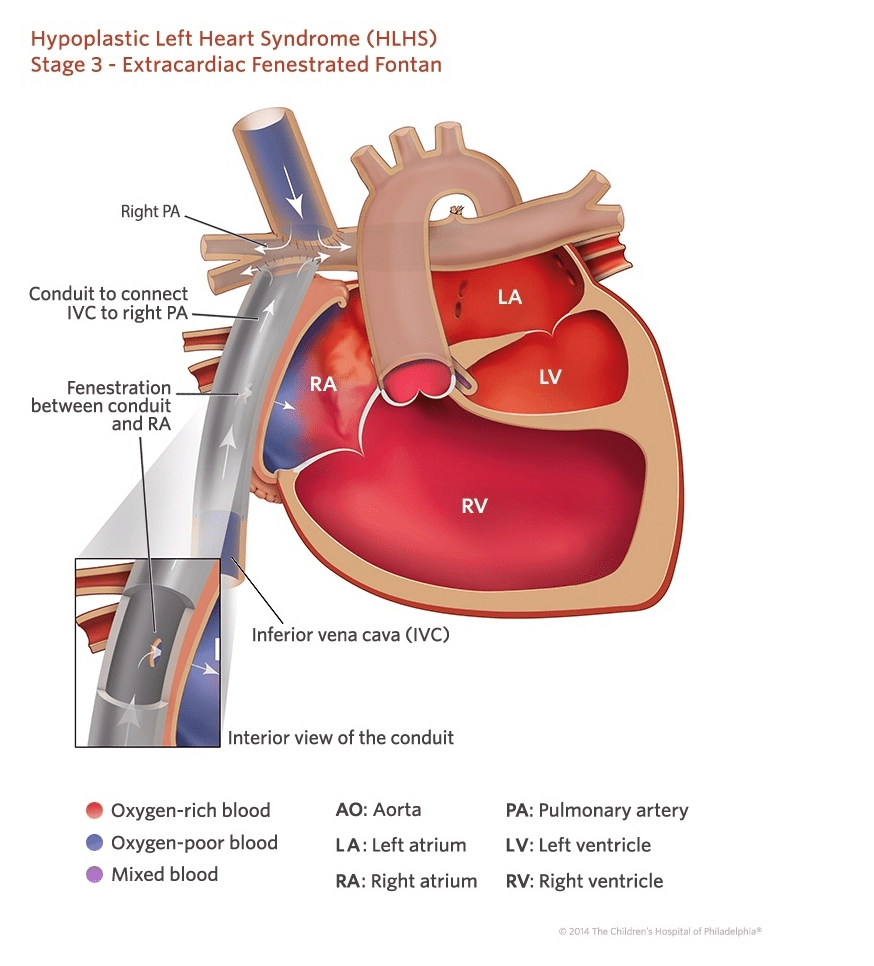
These are the names and descriptions of the three stages of surgical correction of hypoplastic left heart syndrome.
1: Norwood/Sano or Norwood/BT-shunt: neo-aorta is created from the right ventricle and connects the atretic aorta to the pulmonary artery and becomes a "New aorta" carrying blood from RV to systemic circulation. Either a sano shunt (connects RV to to PA) or BT shunt (connects aorta to PA) to allow bloodflow to the lungs.
 2: Glenn: SVC connected to the pulmonary arteries.
2: Glenn: SVC connected to the pulmonary arteries.
3: Fontan: IVC connects to the pulmonary arteries.
A 14-year-old male presents with exertional chest pain that occurs during soccer practice and resolves with rest. The pain is described as a pressure-like discomfort in the middle of his chest, sometimes associated with lightheadedness but no syncope. There is no known family history of sudden cardiac death. His physical exam is unremarkable. ECG is normal. Troponin is negative. Echocardiogram shows normal structure and function. An exercise stress test reproduces his symptoms and shows transient ST depressions in the anterior leads. This is the best next step in diagnosis.
A coronary CT angiogram which reveals a myocardial bridge over the mid-left anterior descending (LAD) artery.
A myocardial bridge occurs when a segment of a coronary artery (usually the LAD) tunnels into the myocardium instead of lying on its surface.
During systole, the bridged segment is compressed, which can impair coronary blood flow — especially during tachycardia, when diastole shortens.
Often asymptomatic, but may cause:
Exertional chest pain
Ischemic ECG changes
Rarely, arrhythmias or sudden cardiac death
Key board clue: Chest pain with normal echo and ECG, but symptoms reproduced on exercise testing and confirmed by coronary CT or cath → think myocardial bridge.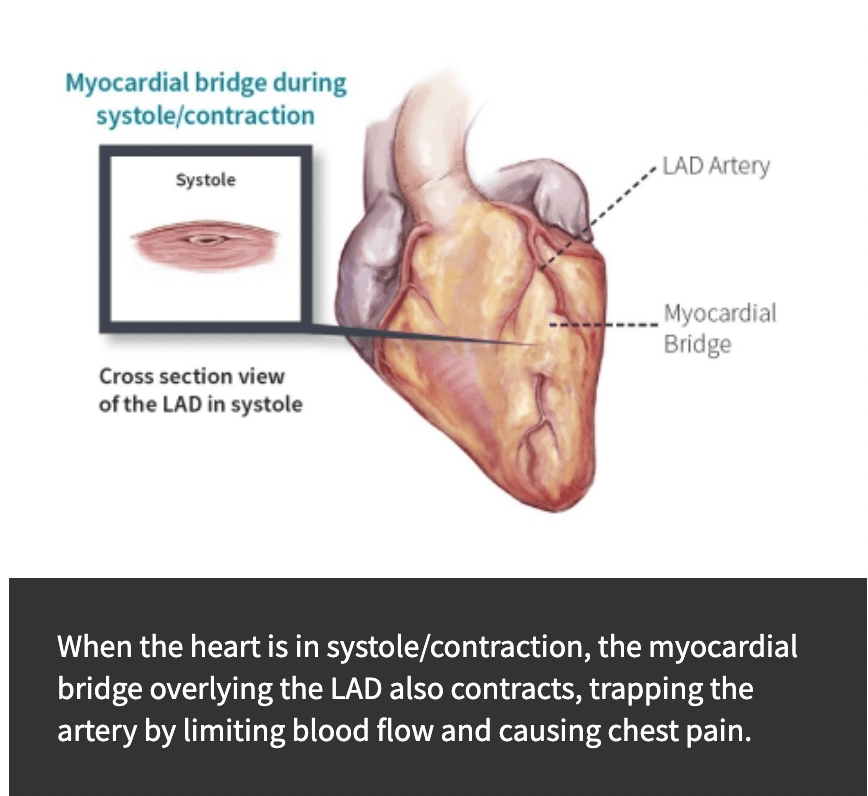
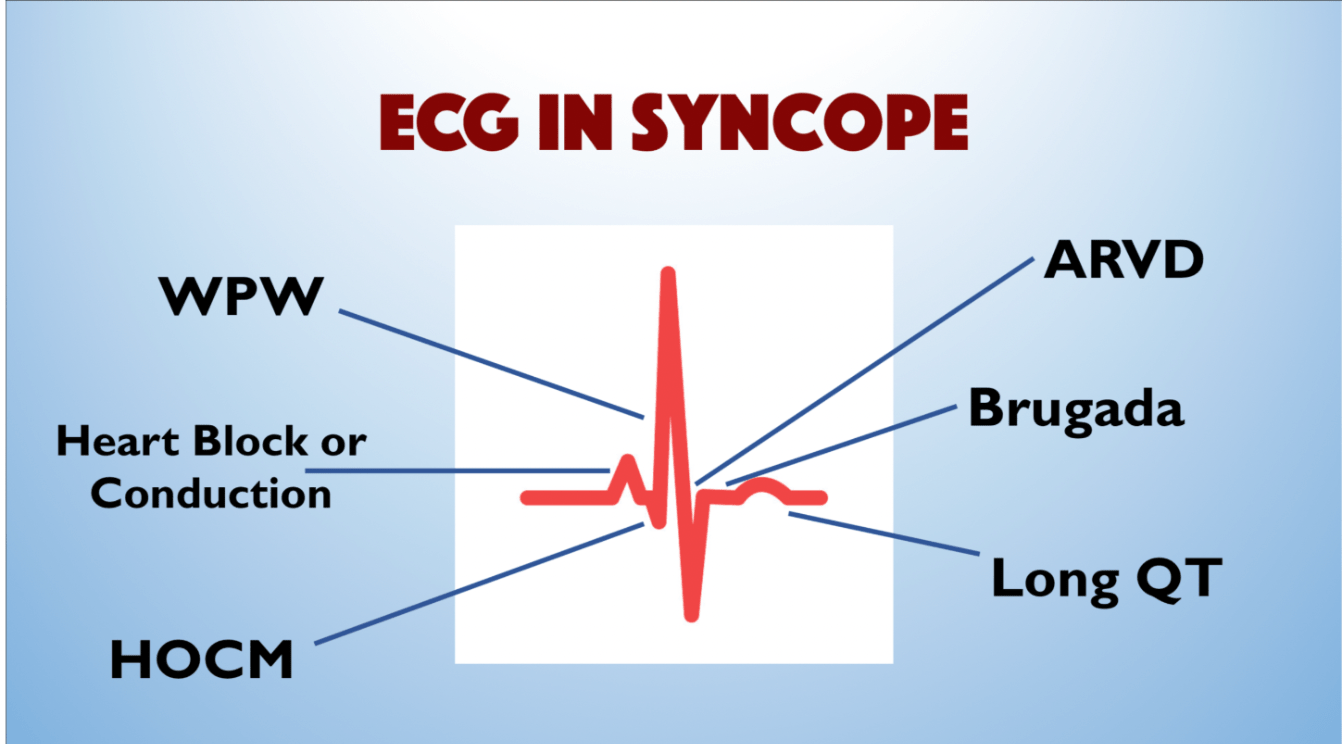
Name at least 4 heart conditions that can be identified on EKG that can cause syncope (extra 200 points if you can name all 6.)
Your patient is in cardiac arrest. Multiple rounds of epinephrine have been given and patient is still pulseless. These two anti-arrhythmics should be considered. Double points if you can name the doses.
Amiodarone: 5mg/kg, IV or IO
lidocaine: 1mg/kg, IV or IO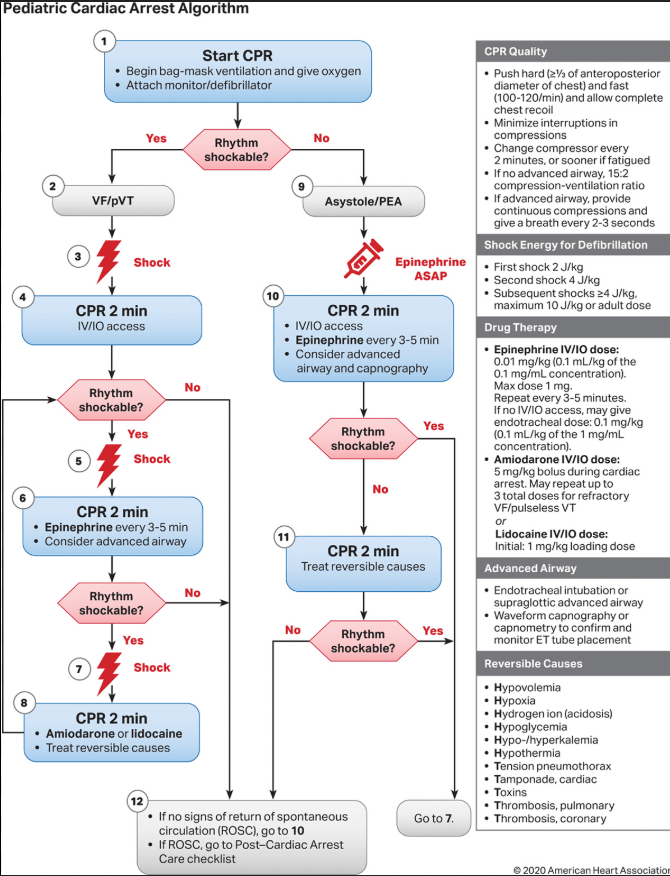
The EKG finding below indicates this diagnosis.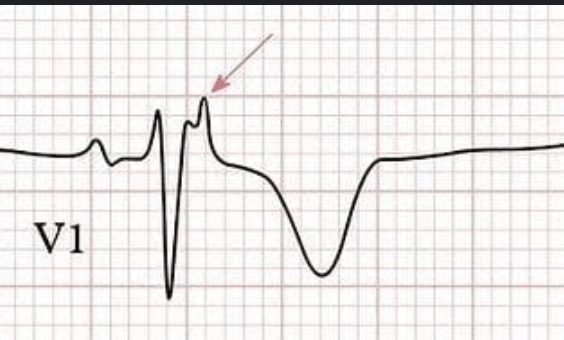
Arrhythmogenic right ventricular dysplasia (ARVD).