A 75-year-old man is evaluated in the emergency department for a 2-day history of left leg pain. The pain started abruptly and has been constant. He has diabetes mellitus, hypertension, peripheral artery disease, and hyperlipidemia. Medications are metformin, chlorthalidone, atorvastatin, cilostazol, and low-dose aspirin.
On physical examination, pulse rate is 108/min and irregular; other vital signs are normal. Cardiac examination reveals an irregularly irregular rhythm. The left lower extremity is cold and mottled. The left popliteal and ankle pulses are absent. Passive range of motion is normal in the left leg, but the patient has significant pain and is unable to actively flex the left knee fully. Left leg sensation is intact. The remainder of the physical examination is unremarkable.
ECG shows atrial fibrillation.
What is the most appropriate next step in management?
Unfractionated heparin
Angiography
Apixaban
Intravenous tenecteplase
Venous duplex ultrasonography
A 49-year-old woman is evaluated during a new patient visit. She has no medical problems or concerning symptoms and takes no medications.
On physical examination, vital signs are normal. The S1 is diminished, and there is an aortic ejection click shortly after the S1. The S2 is normal. There is a grade 2/6, high-pitched, decrescendo early diastolic murmur heard best at the left sternal border. The murmur is accentuated when the patient leans forward.
What is the most appropriate diagnostic test?
Transthoracic echocardiography
Cardiac catheterization
Cardiac magnetic resonance imaging
Stress echocardiography
Transesophageal echocardiography
A 70-year-old woman is evaluated in follow-up for peripheral artery disease. She walks 2 miles daily, and her symptoms force her to stop several times. Medical history is otherwise significant for hypertension and hyperlipidemia. She has a 50-pack-year smoking history but quit 10 years ago. Medications are aspirin, cilostazol, lisinopril, and amlodipine. She was prescribed atorvastatin, but she took the medication for only 1 week after reading that muscle ache is an adverse effect.
What is the most appropriate treatment?
Atorvastatin
Colestipol
Ezetimibe
Icosapent ethyl
A 74-year-old man is evaluated in the hospital for a 6-month history of progressive fatigue and exertional dyspnea, along with increasing peripheral edema and abdominal girth over the past 3 months. He also has coronary artery disease, for which he had a coronary artery bypass graft at age 62 years. Medications are metoprolol, low-dose aspirin, and atorvastatin.
On physical examination, vital signs are normal. Jugular venous distention with prominent waveforms is noted. There is no discernable fall in the central venous pressure during inspiration. An early diastolic sound is present. The liver is enlarged and pulsatile. Ascites is present, and peripheral edema extends to the knees bilaterally.
On chest radiograph, sternotomy wires and vascular clips are seen, and small bilateral pleural effusions are present
What is the most likely diagnosis?
Constrictive pericarditis
Cardiac tamponade
Chronic liver disease
Restrictive cardiomyopathy
A 28-year-old woman is evaluated in the emergency department for substernal chest tightness that started several hours ago. She is 2 weeks postpartum after an uncomplicated pregnancy and delivery. She has no history of cardiopulmonary disease and has no risk factors for atherosclerotic cardiovascular disease.
On physical examination, blood pressure is 122/72 mm Hg in both arms, pulse rate is 90/min and regular, and respiration rate is 24/min. The estimated central venous pressure and apical impulse are normal. An S4 is present. The rest of the examination is unremarkable.
Laboratory studies are significant for an elevated high-sensitivity cardiac troponin level (>99th percentile upper reference limit).
An ECG shows ST-segment elevation in the anterior precordial leads. An echocardiogram shows anterior wall hypokinesis. Estimated ejection fraction is 40%.
What is the most likely diagnosis?
Spontaneous coronary artery dissection
Atherosclerotic plaque rupture
Peripartum cardiomyopathy
Stress-induced (takotsubo) cardiomyopathy
A 42-year-old man is evaluated for dyspnea that occurs while walking on a flat surface and causes him to stop when walking uphill. He has hypertrophic cardiomyopathy, which was diagnosed at age 38 years. He has no other symptoms and has no family history of sudden cardiac death. Medications are metoprolol and disopyramide.
An echocardiogram shows asymmetric septal hypertrophy with maximal septal thickness of 24 mm. Systolic anterior motion of the mitral valve is present with dynamic left ventricular outflow tract obstruction and peak gradient of 64 mm Hg at rest.
Six months ago, 24-hour ECG monitoring performed as part of surveillance showed sinus bradycardia and single premature ventricular contractions averaging 6 per hour.
What is the most appropriate treatment?
Septal reduction therapy
Addition of valsartan-sacubitril
Implantable cardioverter-defibrillator therapy
Replacement of metoprolol with carvedilol
A 45-year-old woman is evaluated in the office for palpitations. She has no other symptoms at rest or with exertion. The palpations make her anxious and are intolerable. They seem to subside with exercise and at night. She does not smoke cigarettes or drink alcohol or caffeinated beverages, and she has no other pertinent personal or family history. She takes no medications.
On physical examination, pulse rate is 65/min and irregular; other vital signs are normal. Heart sounds are regular, with premature beats associated with cannon a waves on neck examination. The remainder of the examination is unremarkable.
Laboratory studies, including complete blood count and thyroid-stimulating hormone level, are normal. Pregnancy test results are negative.
ECG is shown. Echocardiogram is normal.
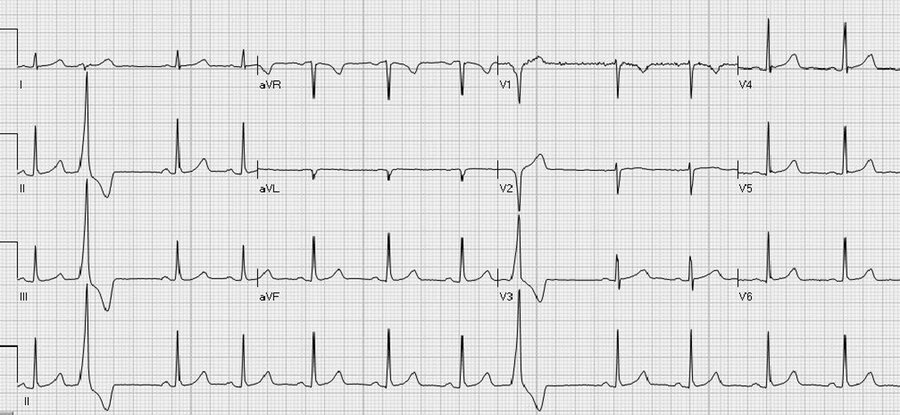
What is the most appropriate management?
Propranolol
Amiodarone
Exercise ECG
Reassurance
A 65-year-old man is evaluated for a 2-day history of several episodes of chest discomfort and dyspnea occurring both at rest and with exertion. Today he presents with 3 hours of persistent severe central chest pressure.
On physical examination, blood pressure is 155/90 mm Hg, pulse rate is 90/min, respiration rate is 20/min, and oxygen saturation is 93% with the patient breathing ambient air. BMI is 29. An S4 is present, but the remainder of the cardiac examination is normal.
High-sensitivity cardiac troponin level is elevated (>99th percentile upper reference limit).
An ECG is shown.
He is given aspirin, clopidogrel, intravenous unfractionated heparin, and a nitroglycerin infusion. His chest pain initially improves but returns despite nitroglycerin infusion and morphine
What is the most appropriate management?
Urgent coronary angiography
Echocardiography
Eplerenone
Oxygen per nasal cannula
A 42-year-old man is evaluated in the emergency department for sudden-onset right-sided weakness. His symptoms resolved fully over the past hour. He has no known medical problems and takes no medications.
On physical examination, vital signs are normal. His heart rhythm is regular. Neurologic examination is normal. No carotid bruits or heart murmurs are noted.
Laboratory study results are normal.
Magnetic resonance angiogram of the brain demonstrates a small left-sided ischemic stroke but no other lesions. ECG, carotid ultrasound, telemetry, and lower extremity ultrasound are normal. A transesophageal echocardiogram demonstrates a patent foramen ovale (PFO) with right-to-left shunt noted with cough and Valsalva release. No other abnormalities are identified.
What is the most appropriate management?
PFO device closure
Aspirin
Warfarin
Observation
A 73-year-old man is evaluated in the emergency department for a 2-hour history of crushing chest pain and diaphoresis. An admission ECG is shown.
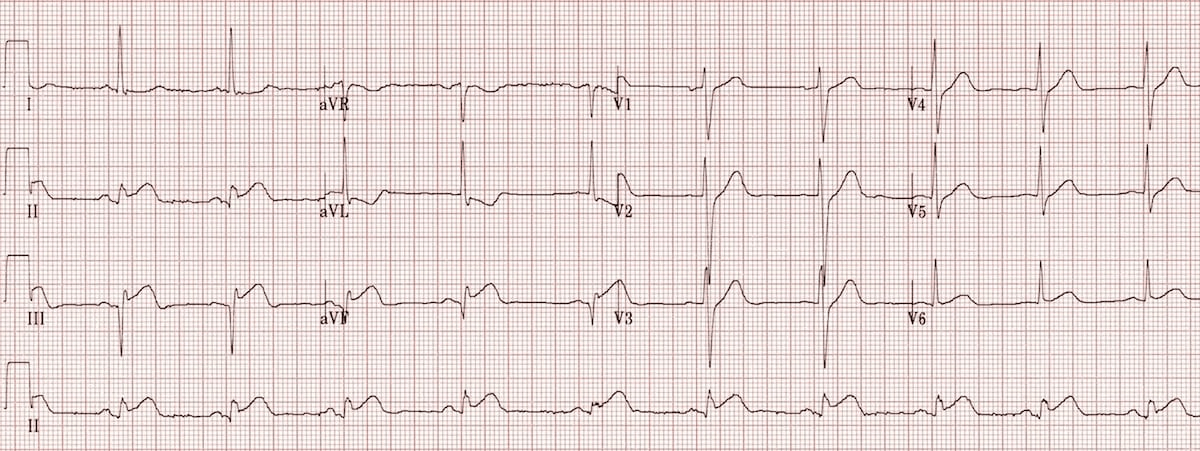
A drug-eluting stent is placed in the proximal right coronary artery, and he is transferred to the coronary care unit.
On physical examination, blood pressure is 80/50 mm Hg, pulse rate is 120/min, respiration rate is 22/min, and oxygen saturation is 94% with the patient breathing ambient air. An S3 is heard; there is no pericardial rub. Central venous pressure is elevated. The lungs are clear to auscultation.
What is the most appropriate treatment?
Intravenous 0.9% saline
Intra-aortic balloon pump placement
Intravenous dobutamine
Oral metoprolol
A 35-year-old man is evaluated for exertional dyspnea. His history is otherwise unremarkable.
On physical examination, vital signs and oxygen saturation are normal. Central venous pressure is elevated. A left parasternal impulse is present. A grade 2/6 systolic murmur is heard at the second left intercostal space, and a diastolic flow rumble is heard at the left sternal border. Fixed splitting of the S2 is present. The remainder of the physical examination is normal.
An ECG demonstrates sinus rhythm with right axis deviation and incomplete right bundle branch block. A transthoracic echocardiogram demonstrates a 1.5-cm ostium secundum atrial septal defect, with moderate right heart enlargement. Left ventricular cavity size and function are normal. The estimated right ventricular systolic pressure is 30 mm Hg.
What is the most appropriate management?
Atrial septal defect closure
Cardiopulmonary exercise testing
Coronary angiography
Echocardiographic surveillance
A 26-year-old woman is evaluated for palpitations that began 2 months ago. The palpitations begin with no specific inciting factors, last 5 to 15 minutes, and are alleviated by rest or deep breathing. They occur a few times per week. Between events, she engages in usual daily activities with no limitations. She has no other pertinent history and takes no medications.
Physical examination findings, including vital signs, are normal.
Resting 12-lead ECG shows sinus rhythm and no abnormalities.
What is the most appropriate diagnostic testing option?
30-Day event monitor
Exercise ECG
Implantable loop recorder
Mobile cardiac telemetry
A 75-year-old man is evaluated for dyspnea and an episode of exertional syncope. He is diagnosed on clinical examination with aortic stenosis.
An ECG shows normal sinus rhythm and left ventricular hypertrophy with repolarization abnormalities. The echocardiogram reveals a severely thickened, minimally mobile tricuspid aortic valve compatible with severe aortic stenosis. However, hemodynamic data from echocardiography show a mean aortic gradient and aortic valve area consistent with moderate aortic stenosis. Left ventricular ejection fraction is greater than 55%, and stroke volume index is normal.
What is the most appropriate next step in management?
Cardiac catheterization
CT of the aortic valve
Exercise stress testing
Surgical aortic valve replacement
Transcatheter aortic valve implantation
A 71-year-old man is evaluated for a 6-month history of exertional chest pain. The pain has increased in frequency and now occurs earlier during his exercise regimen. The pain is relieved by sublingual nitroglycerin. He underwent coronary artery bypass graft surgery 4 years ago. History is also significant for hypertension and hyperlipidemia. Medications are metoprolol, lisinopril, atorvastatin, and aspirin.
Physical examination findings, including vital signs, are normal.
ECG shows left bundle branch block.
What is the most appropriate test?
Vasodilator single-photon emission CT
Dobutamine echocardiography (SPECT)
Exercise ECG
Exercise single-photon emission CT
A 76-year-old woman is evaluated in the emergency department for acute-onset substernal chest discomfort with associated dyspnea. The symptoms developed this morning after her husband's unexpected death. She has hypertension treated with chlorthalidone.
On physical examination, blood pressure is 140/70 mm Hg and pulse rate is 90/min. Oxygen saturation is 98% with the patient breathing ambient air. Other than an S4, the cardiopulmonary examination is normal.
Serum high-sensitivity cardiac troponin level is elevated (>99th percentile upper reference limit).
An ECG demonstrates ST-segment elevation in the anterior precordial leads, and echocardiogram shows preserved basal left ventricular function with apical and mid-ventricular hypokinesis. The left ventricular ejection fraction is 35%. Valve function and the ascending aorta appear normal. Coronary angiography shows normal coronary arteries.
What is the most likely diagnosis?
Takotsubo cardiomyopathy
Ascending aortic dissection
Coronary artery dissection
Coronary artery embolism
A 54-year-old man is evaluated in the emergency department 2 hours after the onset of acute, sharp, central chest pain that radiates to the back and has intensified over time. He has hypertension. He quit smoking 2 years ago. Medications are hydrochlorothiazide and lisinopril.
On physical examination, blood pressure in the right arm is 90/56 mm Hg, blood pressure in the left arm is not obtainable, and pulse rate is 120/min. He is confused and diaphoretic. Cardiac examination reveals a summation gallop and a grade 3/6 diastolic murmur at the right upper sternal border. Pulmonary examination reveals crackles. Radial pulses are weakly present on the right and absent on the left. Lower extremity pulses are diminished. Skin is cool and mottled.
Chest radiograph reveals a widened mediastinum, and a CT angiogram shows a type A aortic dissection.
What is the most appropriate treatment?
Open aortic repair
Coronary angiography
Intravenous nitroprusside
Thoracic endovascular aortic repair
A 69-year-old man is evaluated for a 1-week history of redness at the site of his pacemaker. Medical history is significant for diabetes mellitus and hypertension. Medications are metformin, atorvastatin, and lisinopril.
On physical examination, the patient is afebrile; other vital signs are normal. The pacemaker site is shown. The remainder of the examination is unremarkable.

Laboratory studies, including leukocyte count, are within normal limits. Three sets of blood cultures are obtained.
What is the most appropriate additional management?
Pacemaker extraction
Aspiration of the device pocket
Topical mupirocin
Clinical observation and reassessment
A 78-year-old woman is evaluated 4 months after placement of a drug-eluting stent for treatment of chronic stable angina pectoris. She is asymptomatic. She has hypertension, gastroesophageal reflux disease, and a history of several colonic angiodysplasias treated with electrocoagulation 8 months ago. Medications are pravastatin, aspirin, clopidogrel, metoprolol, hydrochlorothiazide, ferrous sulfate, and omeprazole.
On physical examination, blood pressure is 132/72 mm Hg, pulse rate is 78/min, and respiration rate is 20/min. BMI is 17. Scattered ecchymoses are evident over both lower extremities.
Results of laboratory studies show a hematocrit of 34%.
What is the most appropriate initial management?
Discontinue clopidogrel
Assess platelet reactivity|
Discontinue aspirin and clopidogrel
Assess platelet reactivity
A 65-year-old man is evaluated in the hospital for progressive dyspnea with light exertion. He was diagnosed with restrictive cardiomyopathy 2 years ago and atrial fibrillation 18 months ago. Attempts at pharmacologic rhythm control have been unsuccessful. Medications are apixaban, spironolactone, torsemide, and potassium chloride.
On physical examination, blood pressure is 106/68 mm Hg, pulse rate is 86/min and irregularly irregular, and oxygen saturation is 94% with the patient breathing ambient air. Central venous pressure is elevated. Bibasilar crackles are present. Hepatomegaly is noted. There is bilateral pitting edema to the knees.
ECG shows atrial fibrillation with a ventricular rate of 86/min, right bundle branch block, and QRS duration of 136 ms.
An echocardiogram shows a left ventricular ejection fraction of 50%, increased left and right ventricular wall thickness, and abnormal left ventricular diastolic function. The estimated right ventricular systolic pressure is 64 mm Hg.
What is the most appropriate management?
Cardiac transplantation
Cardiac resynchronization therapy
Implantable cardioverter-defibrillator
Pulmonary vein isolation
A 28-year-old woman is seen for pregnancy planning. She underwent mitral valve replacement with a mechanical prosthesis 4 years ago for congenital mitral valve stenosis. She is asymptomatic. Medications are warfarin, 4 mg/d, and low-dose aspirin. Her INR measurements have been within the therapeutic range for the past 18 months, including her most recent INR measurement of 3.0.
Other than a mechanical-sounding S1, vital signs and all physical examination findings are normal.
Echocardiography shows a normally functioning mitral valve prosthesis and normal left ventricular function and estimated pulmonary artery pressure.
The patient would like to attempt pregnancy as soon as possible. During this time, aspirin will be continued.
What is the most appropriate anticoagulation strategy during the first trimester?
Continue warfarin
Stop warfarin and start bivalirudin
Stop warfarin and start dabigatran
Stop warfarin and start subcutaneous dose-adjusted unfractionated heparin