Myocarditis
This nursing intervention is the priority when a patient with heart failure reports sudden weight gain and increased leg swelling.
What is administer prescribed diuretic medication?
Fever and fatigue in a post-transplant patient may indicate this serious complication.
What is organ rejection?
The nurse should monitor for this serious complication when a patient with infective endocarditis presents with Janeway lesions, indicating micro-embolic events from circulating bacteria.
What is systemic embolization?
In a patient with chronic venous insufficiency (CVI), this improvement, resulting from a walking program, indicates better circulation and reduced symptoms.
What is decreased episodes of restless legs?
This condition occurs due to a sudden reduction in blood flow to the heart, often caused by a ruptured atherosclerotic plaque and thrombus formation.
What is Acute Coronary Syndrome (ACS)?
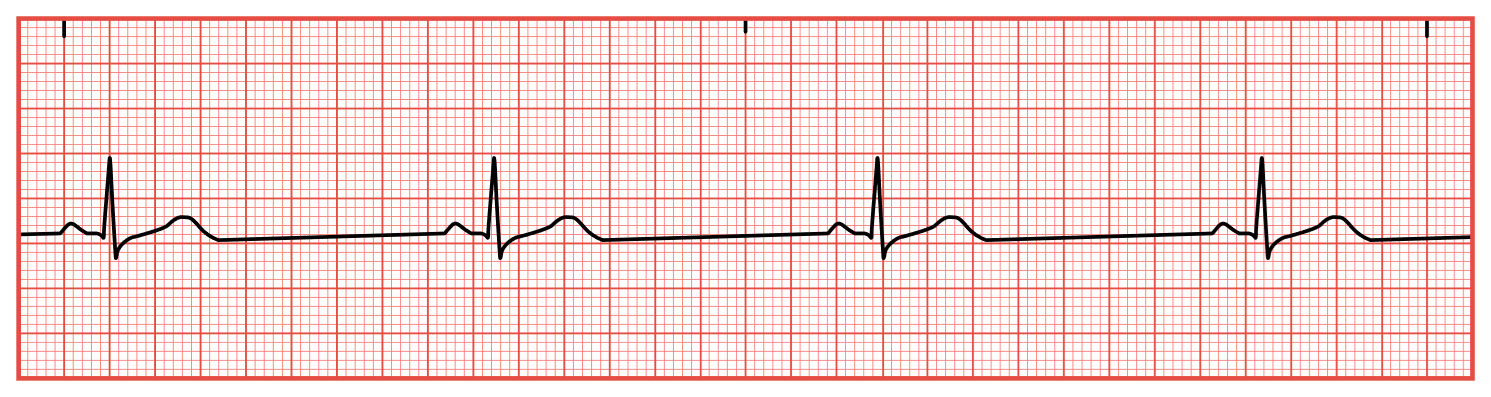
What is sinus bradycardia?
Treat with Atropine and/or pacing if symptomatic.
A patient with chronic heart failure is being discharged. Which statement indicates effective teaching?
A)“I will weigh myself daily and report a 2-pound gain in 24 hours.”
B) “I will avoid physical activity to rest my heart.”
C) “I can skip taking my diuretic if I travel long distances to avoid numerous bathroom stops.”
D) “I may need to increase my fluid intake to stay hydrated.”
.
Correct Answer: A — Daily weights help monitor fluid retention, a key sign of worsening heart failure.
Which discharge teaching point is essential for a patient post-heart transplantation?
A) “You will only need to take immunosuppressant medications for a year.”
B) “Avoid large crowds and individuals with infections.”
C) “You can resume smoking if it helps reduce stress.”
D) “You should limit daily exercise to 5 minutes.”
Correct Answer: B — Infection prevention is crucial due to immunosuppressive therapy.
This scratchy, high-pitched sound, best heard at the left lower sternal border with the patient leaning forward, is a hallmark finding in acute pericarditis.
What is a pericardial friction rub
Among various measures to prevent complications of chronic venous insufficiency (CVI), this specific behavior is the most crucial for managing venous pressure and promoting circulation.
What is wearing compression stockings consistently?
This classic symptom of myocardial infarction is described as a crushing, substernal pain that may radiate to the left arm, jaw, or back.
What is chest pain or angina?
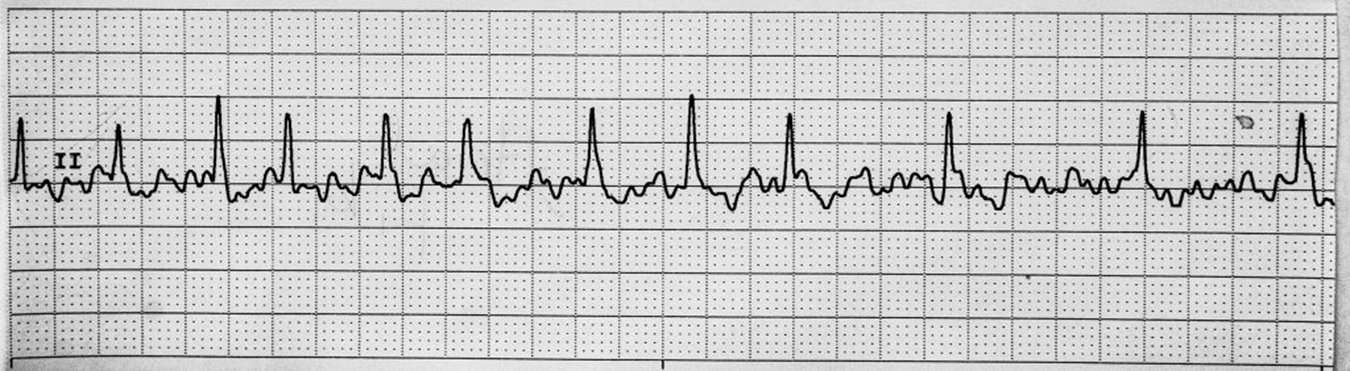
What is atrial fibrillation?
Treatment
Drugs to control ventricular response, prevent stroke, and/or convert to sinus rhythm (amiodarone most common)
Electrical cardioversion
Anticoagulation
Radiofrequency ablation
A nurse expects to hear this lung sound when assessing a patient with left-sided heart failure.
What are crackles in the lungs?
If a patient taking ivabradine for heart failure has a resting heart rate of 55 bpm, the nurse should take this action.
What is withhold the medication?
In a patient with myocarditis and a new arrhythmia, this action is the most urgent due to the risk of worsening myocardial inflammation and potential hemodynamic instability.
What is notify the provider immediately?
Effectiveness of pentoxifylline (Trental) in a patient with chronic venous insufficiency (CVI) is indicated by this improvement, which results from enhanced blood flow.
What is improved circulation and reduced claudication?
Trental: is a hemorheologic (the study of blood flow) agent that improves blood flow by making red blood cells more flexible and reducing blood viscosity. This helps increase oxygen delivery to tissues, especially in the legs, reducing symptoms like claudication (pain from poor circulation) in patients with chronic venous insufficiency (CVI) or peripheral arterial disease (PAD).
This diagnostic test is the first-line assessment tool in ACS and helps differentiate between STEMI and NSTEMI.
What is a 12-lead ECG?
What is NSR with PVCs?
This compensatory mechanism of the sympathetic nervous system increases heart rate and contractility in heart failure.
What is increased myocardial contractility?
A patient recovering from a heart transplant asks about infection prevention. Which statement by the patient requires further teaching?
A) “I will wash my hands frequently.”
B) “I will avoid large crowds.”
C) “I will stop my immunosuppressant if I feel better.”
D) “I will monitor for signs of fever.”
Answer: C) “I will stop my immunosuppressant if I feel better.”
Rationale: Stopping immunosuppressants increases the risk of rejection.
Blood cultures are performed in a patient with infective endocarditis primarily for this reason, which helps guide targeted antibiotic therapy.
What is to identify the infecting organism?
This sign, characterized by a moist, pink, and bumpy appearance in the wound bed, indicates that a venous ulcer is healing effectively.
What is pink granulation tissue in the wound bed?
This emergency procedure must be performed within 90 minutes of first medical contact in a STEMI case to restore blood flow to the heart.
What is Percutaneous Coronary Intervention (PCI)?
The treatment for this rhythm.
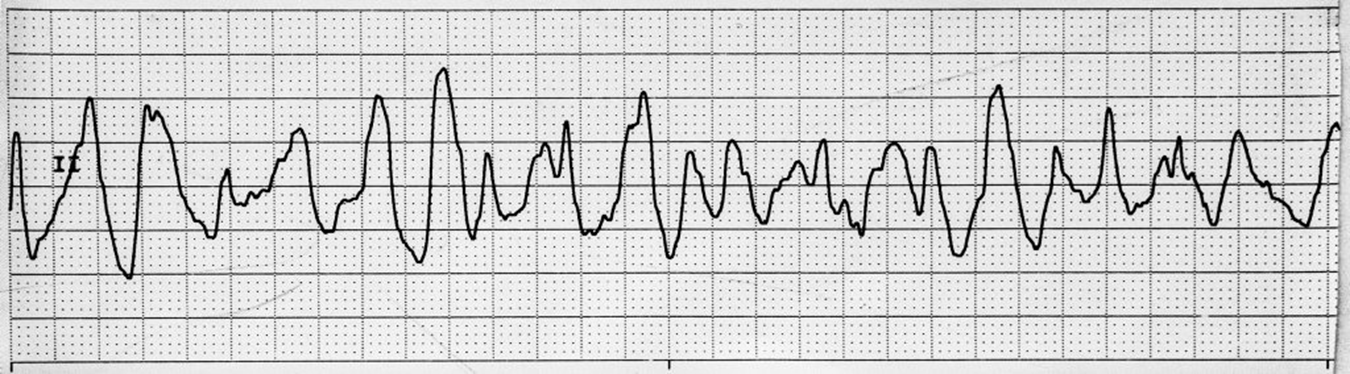
What is Immediate defibrillation?
A patient with ADHF and pulmonary edema requires which priority intervention?
A) Encourage ambulation
B) Place in High Fowler's position
C) Administer IV furosemide
D) Restrict fluid intake
Answer: C) Administer IV furosemide
Rationale: IV diuretics reduce fluid overload and relieve congestion.
Which nursing intervention is most important post-heart transplant?
A) Monitor for acute rejection signs.
B) Encourage bed rest for one month.
C) Restrict fluid intake to prevent overload.
D) Provide low-fiber diet education.
Answer: A) Monitor for acute rejection signs.
Rationale: Early detection of rejection is crucial to prevent graft failure.
A patient with pericarditis should adopt this position to relieve chest pain, as it helps reduce pericardial pressure and discomfort.
What is upright and leaning forward?
This patient statement demonstrates a proper understanding of a key therapeutic measure for managing chronic venous insufficiency (CVI), as it uses gravity to facilitate venous return and reduce lower extremity edema.
“I will elevate my legs above heart level when sitting.”
Patient statement reflects the most effective technique for promoting venous return and preventing edema in chronic venous insufficiency (CVI)?
This dual therapy includes aspirin and a P2Y12 inhibitor and is crucial for preventing platelet aggregation in ACS patients.
What is Dual Antiplatelet Therapy (DAPT)?

What is Normal Sinus Rhythm?
Which patient statement indicates a need for more education?
A) "I will weigh myself daily and report a 2-pound weight gain in two days.
B) "I can skip my medication if I am feeling nauseated."
C) "I will increase sodium intake to prevent dehydration."
D) "I will monitor for ankle swelling."
Answer: C) "I will increase sodium intake to prevent dehydration."
Rationale: Increased sodium can worsen fluid retention.
During discharge teaching for a post-heart transplant patient, which topic is most critical?
A) Importance of daily weight monitoring.
B) Recognition of infection symptoms.
C) Benefits of aerobic exercise.
D) Reducing salt intake.
Answer: B) Recognition of infection symptoms.
Rationale: Immunosuppressive therapy increases infection risk.
The nurse is evaluating a patient with myocarditis. Which outcome indicates improvement?
A) Increased heart rate
B) Decreased chest pain
C) Development of a new murmur
D) Elevated troponin levels
Answer: B) Decreased chest pain
Rationale: Less chest pain signals reduced myocardial inflammation.
A nurse evaluates a patient's adherence to CVI prevention strategies. Which action indicates proper self-care?
A) The patient applies compression stockings after getting out of bed.
B) The patient elevates their legs for 10 minutes once a day.
C) The patient performs ankle flexion exercises while sitting for extended periods.
D) The patient increases sodium intake to maintain hydration.
Answer: C) The patient performs ankle flexion exercises while sitting for extended periods. Rationale: Promotes venous return and prevents venous stasis.
A and B are incorrect because: A) Compression stockings should be applied before getting out of bed to prevent venous pooling from gravity and B) Elevating legs for only 10 minutes once a day is insufficient. Frequent and prolonged elevation is necessary to promote venous return effectively.
This life-threatening complication of myocardial infarction occurs in 80-90% of ACS patients and can lead to sudden cardiac arrest.
What are dysrhythmias (ventricular fibrillation and tachycardia)?
The treatment for this rhythm is the patient is symptomatic?
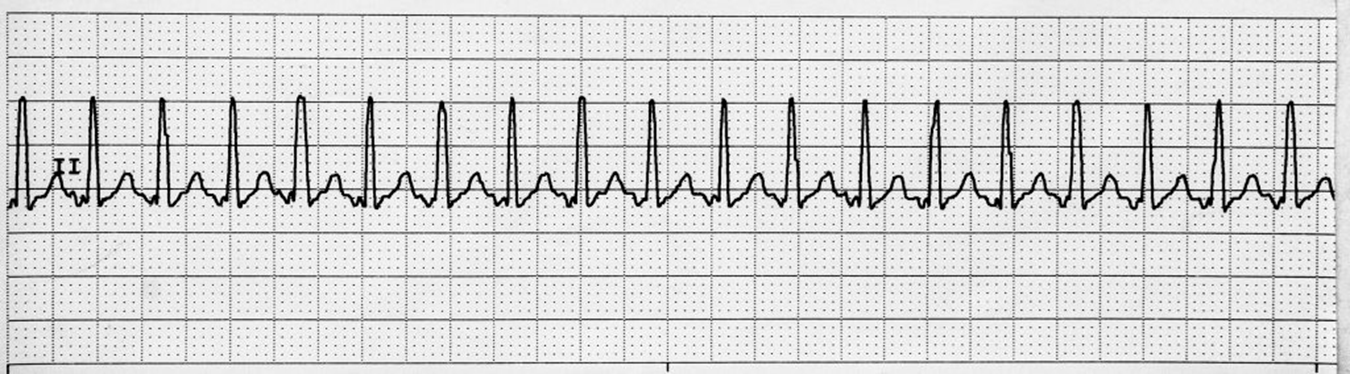
Guided by cause (e.g., treat pain)
Vagal maneuvers
β-blockers, adenosine, or calcium channel blockers
Synchronized cardioversion