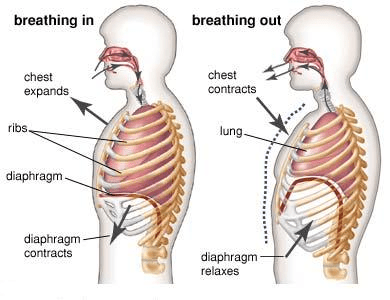
The diaphragm contracts. Increasing lung volume, and making the pleural pressure more negative. Air to rushes in and fills the lung.
Inspiration
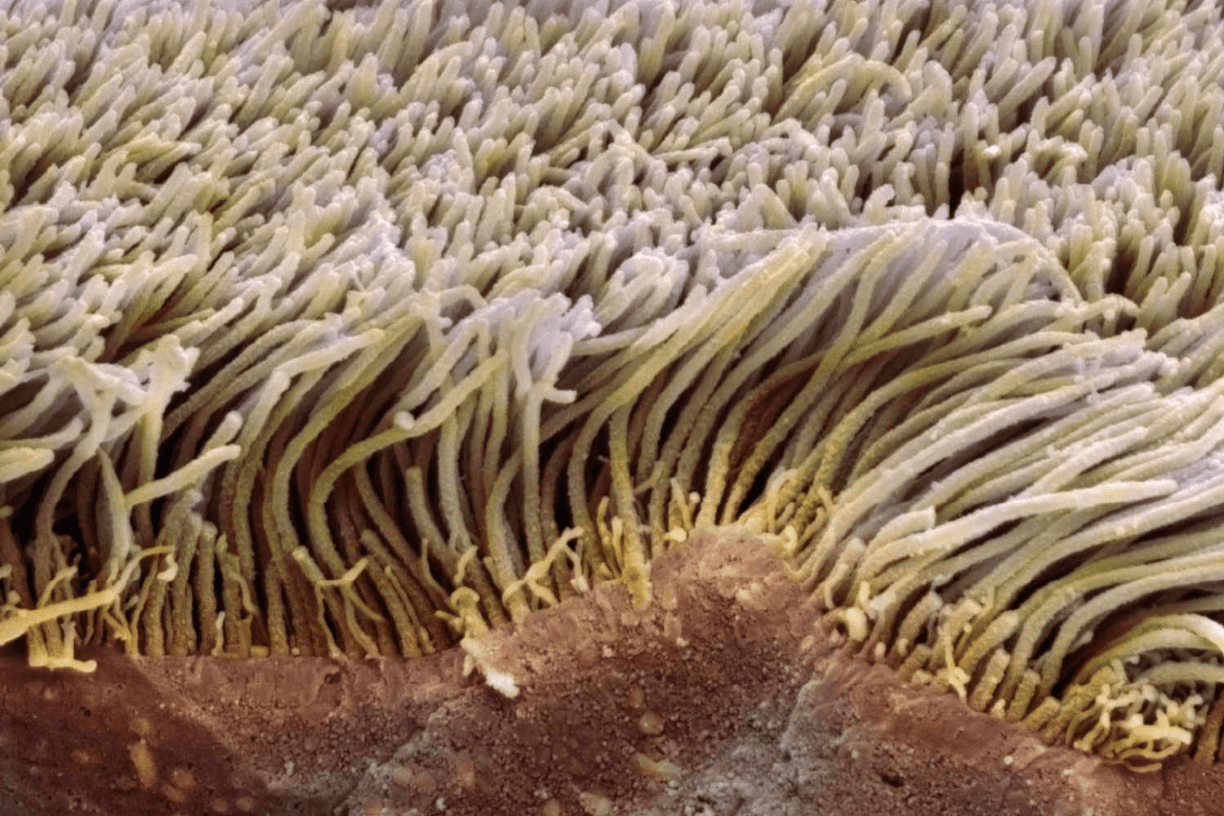
I move particles at a rate of 3mm per min to the larynx where these particles are either coughed up or swallowed.
Cilia
A build up of fluid in the interstitial space of the lungs
APO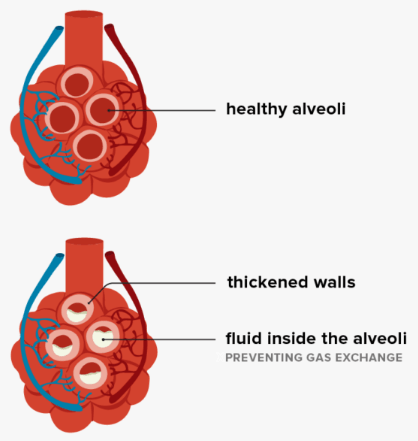
Characterised by Low Pa02 (Pa02 <50mmHg) but C02 is not elevated (paC02 <60 mmHg).
Type 1 Respiratory Failure or Hypoxemic Respiratory Failure
The diaphragm relaxing, and intrinsic recoil of the lungs allowing air to be expelled passively
Expiration
Observing respiratory rate, pattern, effort, colour, accessory muscles, chest symmetry and tracheal position are examples of what component of the respiratory assessment?
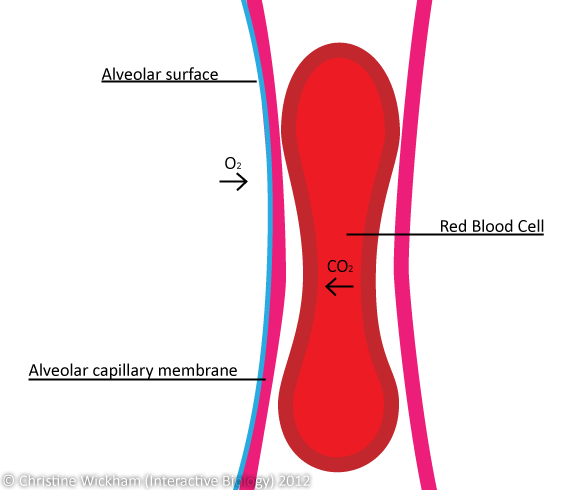
I form 70-80 sq meters of surface area in close contact with capillaries for gas exchange.
Alveoli

Viral replication, cellular damage, inflammatory mediators release, and recruitment of immune cells. Leads to airway obstruction, reduced mucociliary clearance and in severe cases cause pneumonia.
Respiratory Virus
Characterised by low Pa02 (<50mmHg) and elevated PaCO2 (>60mmH)
Type 2 Respiratory Failure
During quiet breathing the amount of air that is inspired and expired
Tidal Volume - Vt
Discontinuous, popping sounds auscultated during breathing. Can be categorized as fine or coarse.
Crackles
When in network for gas exchange, each red blood cell passes by me single file for approximately 3/4 second, and exchanges 02 or C02 within 0.25seconds
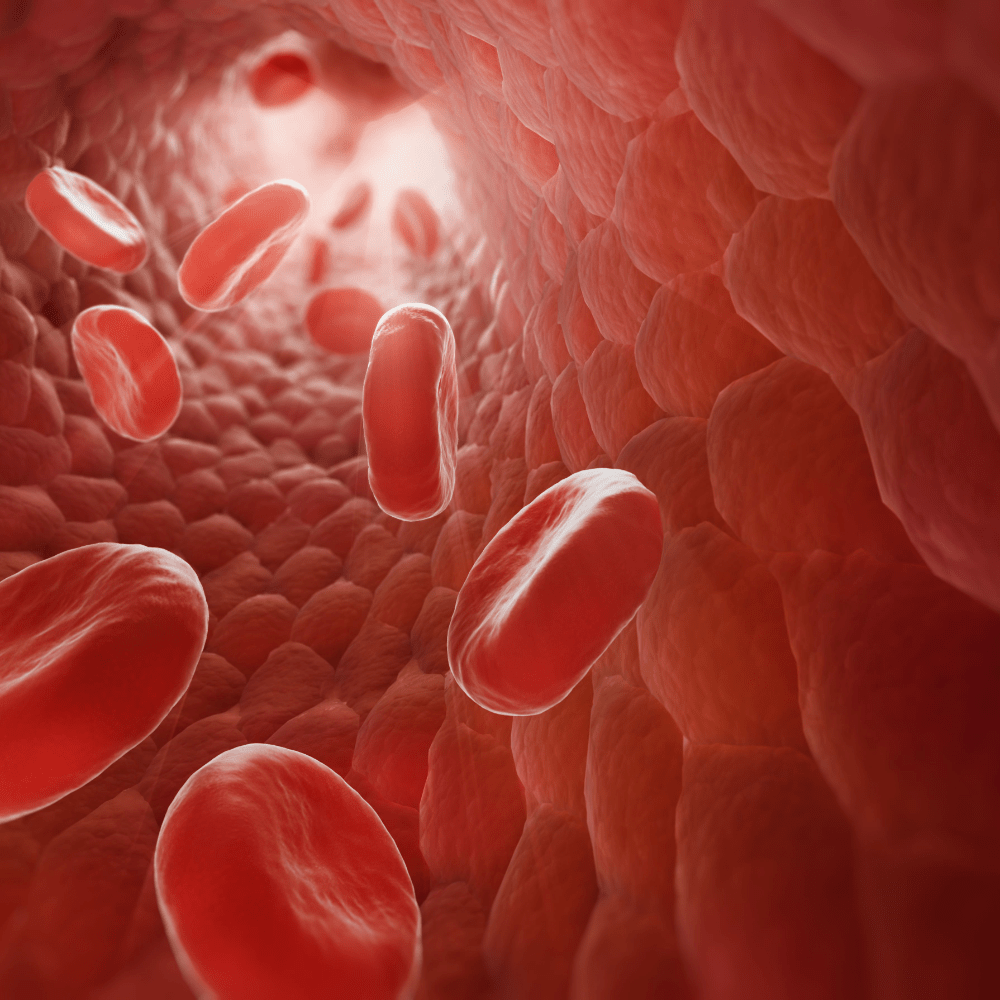
Capillary Membrane
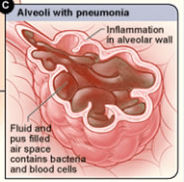
Pathogen invades the alveoli, leading to an inflammatory response, accumulation of fluid, pus, and inflammatory cells within the alveoli. This contributes to impaired gas exchange.
Pneumonia
Imbalance between the amount of air reaching the alveoli and the amount of blood perfusion the pulmonary capillaries.
Ventilation-Perfusion (V/Q) Mismatch
The lungs ability to stretch and expand
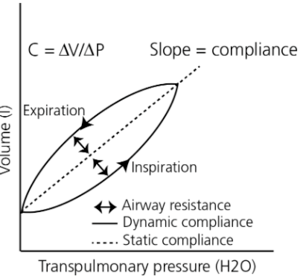
Lung compliance
Continuous, high-pitched, musical sounds. Often indicating narrowing of the airways
Wheeze
It takes 0.25 seconds for these levels to reach normal saturation when exposed to alveolar gas
Haemoglobin
Loss of elasticity, the walls between alveoli are destroyed, alveoli become large and floppy because there is less surface area for gas exchange, airways are thick, inflammed and there is increased mucus production
Chronic Obstructive Pulmonary Disease - COPD
Alveoli are well-ventilated, however there is poor gas exchange due to poor blood supply
Dead Space
More air than blood flow in lung segment
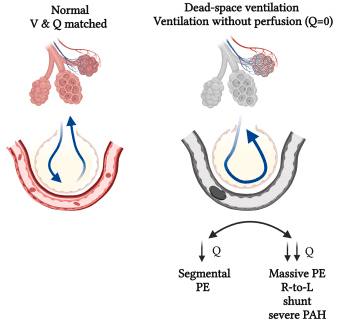
Examples:
-PE
-Pulmonary Hypertension
Volume in the alveoli after passive expiration
Functional Residual Capacity
Important to keep small airways open, thus prevention areas of collapse and allows for continual gas exchange.
Can be caused by trauma or a procedure that causes a leak from the respiratory tract, esophagus, or gastrointestinal tract. This can cause abnormal presence of air in the tissues beneath the skin.
Subcutaneous Emphysema
A gas that diffuses 20 times more rapidly than oxygen
C02
Airway inflammation and hyper-responsiveness cause airway smooth muscles to contract and relax.
Airway remodeling and mucous hypersecretion occur.
These contribute to variable airflow obstruction.
Additionally, chronic inflammation can lead to irreversible airway remodeling.
Asthma
1. Airway inflammation
-Immune cell infiltration, cytokine release, IgE production
2. Airway hyper-responsiveness
-Causes bronchospasm
3. Airway remodeling
-Repeated inflammation and repair can lead to long-lasting structural airway changes eg. thickening airway wall, increased smooth muscle mass, increased collagen under the epithelium
4. Mucous hypersecretion
-Increased mucous production and inflammation and swelling of the airways, can lead to mucous plug formation further obstructing the airways
Blood flowing past poorly ventilated alveoli that does not exchange gas.
Poorly oxygenated blood then lowers the total oxygen content of the arterial blood - leading to hypoxaemia.
Shunt/shunting
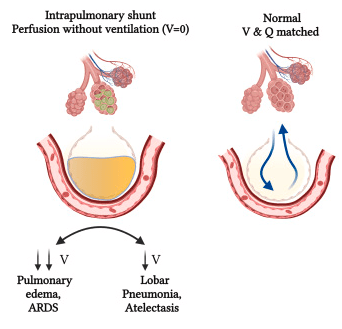
Common causes of shunt include:
- Pnueomnia and pulmonary oedema
- Tissue trauma - alveolar wall swelling
- Atelectisis collapse of alveoli from failure to expand
- Mucus plugging