What is a big concern (hemodynamically) for patient's s/p repair of coarctation of the aorta?
Why is this a big concern to the physicians?
Paradoxical HTN
LV is used to having to use lots of force to adequately provide for the body through the coractation- when repaired, the LV has to "re-learn" that it doesn't need as much force. Thus can cause HTN. Will self correct over time.
Can pop sutures/ tamponade!
If your patient is on 5ml/hr of breastmilk ng - how much feeds should you heat up? How often should you change the tubing?
4 hours worth- 20 mls
change tubing q 4
What do you see in this xray?

Pleural effusion
What would you do if your patient's ett comes out?

SVT
Vagal Manuvers
Adenosine
Synchronized Cardioversion
Patient is a pre-op tet admitted for observation. Patient is crying and irritable and turns blue? Why did the patient turn blue? What interventions would be done to treat patient?
tet spell d/t irritability
tet spell is decrease in svr which leads to R to L shunting thus more blue (de-oxygenated) blood to the body (can be caused by rvot obstruction, increase pvr or decrease svr)
Treatment
legs to chest- increases svr
oxygen- supportive
morphine- sedation and decrease root rvot obstruction
fluid bolus- increase svr
phenylephrine - increases svr
bblocker- decrease root rvot obstruction
Your patient is 3 months old, has a PIV, a single lumen power PICC and a g tube.
Does your patient get a CHG bath? What about this patient indicates that they get a chg?
Yes!
Central Line
Older than 2 month!
What is wrong with this Xray?

ETT is right mainstem
ETT should be between 2nd and 4th intercostal space
VBG on 2 Ventricle oxyhgb is 45
Patient - SpO2 95
What does it mean/ treatment?
AVO2 difference is 50 (Norm 20-40)
High is indication of high consumption of O2. Can be indication of low cardiac output.
Causes of low SVO2- low hgb (less carrying capacity), SaO2 is low.
Treatment- supportive and treat cause if treatable.

Junctional
Symptomatic or Asymptomatic
Sedation
Electrolytes (Magnesium!)
Keep Cool 36-37
Override pace if wires are present
Meds: Precedex, Amiodarone (Give CaCl prior), procanamide, esmolol
What is the flow of blood through the heart of a hlhs patient s/p hybrid?
IVC/ SVC > RA> RV & LA (Through asd)> PA's > lungs & through PDA to body
It is a Tuesday. Your patient has a right IJ TL.
Upon initial assessment, the TL dressing is peeling up and the port is exposed partially.
Does this dressing need to be changed?
Change the dressing
Dressing are Q 7 days, on Sundays ideally
BUT CHANGE if not occlusive.
If still occlusive but starting to peel you may secure with additional dressing.

NG tube is in lungs
How can you adjust a patient's CO2 on a ventilated patient?
Goal
Lower CO2- increase the rate OR increase the TV (on volume control you can choose a tv) on pressure control you can provide additional support/ pressure
Raise CO2- wean rate/ sedate patient breathing over rate, decrease pressure/ TV
V Tach
Runs vs Sustained?
CPR/ Defibrillate
Amio or Lidocaine
Electrolyte replacement if stable?
How would you know if your patient is having a tamponade?
increase HR
decrease BP
cvp high
desats
CHEST TUBE output
How often should caps/ microclaves at the end of a central line be changed?
every 4 days! same as the tubing!

Pneumothorax L Side
Pneumos have no lung markings, only air which appears dark on xray.
Interpret this ABG
7.56/26/70/30/-1
Ventilated patient. What is your intervention?
Respiratory alkalosis
Patient is being over-ventilated
Wean rate/ give sedation.
 HR = 190
HR = 190
Sinus Tachycardia
Treat cause!
Causes: Irritability, hypovolemia, hyperthermia, sepsis, heart failure, hypoxia
Tamponade?
What major defects do not have a murmur once fully repaired?
TAPVR, TGA, ASD/ VSD if no residual, COA,
Anything with no shunt, vsd or asd!
How often do we change our arterial line dressings?
As needed!

What congenital heart defect has this boot shaped xray? Why?
Tetralogy of fallot - RV hypertrophy!
How would you interpret this gas? What treatment would you expect for a gas like this? What probably caused it?
7.53/40/80/38/+9
Metabolic Alkalosis
What treatment? Diamox or wean diuretics
Cause: Lasix/ hypovolemia
HR 80
Patient 5m 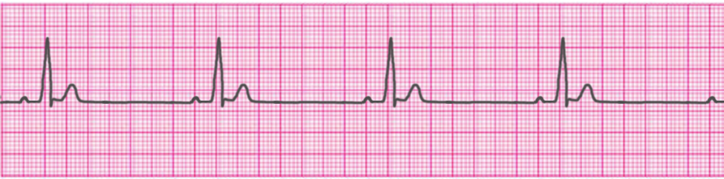
Sinus Bradycardia
Pacing if wires present!
Epinephrine or Atropine if symptomatic
Treat underlying cause- did patient vagal? Hypothermia?