True or false: Enuresis and encopresis are not diagnosed if the behavior is intentional.
What is false?
Enuresis -- 5y/o, encopresis -- 4y/o.
Major and mild neurocognitive disorders (NCDs) exist on a spectrum of cognitive and functional impairment. Of the following, this constitutes an important threshold differentiating the two diagnoses:
A. Whether or not the individual is concerned about the decline in cognitive function.
B. Whether or not there is impairment in cognitive performance as measured by standardized testing or clinical assessment.
C. Whether or not the cognitive impairment is sufficient to interfere with independent completion of activities of daily living.
D. Whether or not the cognitive deficits occur exclusively in the context of a delirium.
E. Whether or not the cognitive deficits are better explained by another mental disorder.
What is C, whether or not the cognitive impairment is sufficient to interfere with independent completion of activities of daily living?
Criterion B for major or mild NCD relates to the individual’s level of independence in everyday functioning. Individuals with major NCD will have impairment of sufficient severity to interfere with independence, such that others will have to take over tasks that the individuals were previously able to complete on their own. Individuals with mild NCD will have preserved independence, although there may be subtle interference with function or a report that tasks require more effort or take more time than previously. The distinction between major and mild NCD is inherently arbitrary, and the disorders exist along a continuum. Precise thresholds are therefore difficult to determine. Careful history taking, observation, and integration with other findings are required, and the implications of diagnosis should be considered when an individual’s clinical manifestations lie at a boundary. For both mild and major NCD, Criterion A requires evidence of a cognitive decline based on 1) concern on the part of the patient, a knowledgeable informant, or a clinician that there has been such a decline; and 2) impairment in cognitive performance as documented by standardized testing or other objective assessment. For major NCD, significant decline and substantial impairment are specified; for mild NCD, the words modest and mild are used.
This symptom of narcolepsy is characterized by sudden, brief episodes of muscle weakness or paralysis, often triggered by strong emotions.
What is cataplexy?
True or false: The lobotomy was always an un conventional, fringe treatment.

What is false? It was very popular and António Egas Moniz won the 1949 Nobel Prize in Medicine for inventing the lobotomy.
T or F: Negative symptoms are part of the diagnosis of brief psychotic disorder?
What is false?
They first appear in the dx of schizophreniform disorder.
Brief psychotic disorder (BPD) is diagnosed based on a sudden onset of positive psychotic symptoms like delusions, hallucinations, or disorganized speech, with a full return to premorbid functioning within one month. The diagnostic criteria focus on these acute, overt symptoms because the disorder is defined by its transient nature and the presence of a psychotic episode that resolves completely, whereas negative symptoms (like social withdrawal or lack of emotion) are associated with longer-lasting and more pervasive psychotic disorders, such as schizophrenia.
True or false: Separation anxiety is a benign disorder and does not present with an increased risk for suicide.
What is false?
Children with separation anxiety have an increased risk of suicide, especially when it's a severe or persistent issue, as it's often linked to other mental health challenges like depression, anxiety disorders, and a history of trauma. While a direct link between separation anxiety and suicidal ideation exists, the risk is higher when separation is traumatic and associated with other emotional and mental health problems, according to studies cited by the National Institutes of Health (NIH) and Family Medicine and Community Health.
Of the following, this is a core feature of major or mild neurocognitive disorder with Lewy bodies:
A. Fluctuating cognition with pronounced variations in attention and alertness.
B. Recurrent auditory hallucinations.
C. Spontaneous features of Parkinsonism, with onset at least 1 year prior to development of cognitive decline.
D. Fulfillment of criteria for rapid eye movement (REM) sleep behavior disorder.
E. Evidence of low striatal dopamine transporter uptake in basal ganglia as demonstrated by single photon emission computed tomography (SPECT) or positron emission tomography (PET) imaging.
What s A??
Recurrent well-formed visual hallucinations (not auditory hallucinations) and parkinsonism arising after (not earlier than) cognitive impairment are the other core features of major or mild neurocognitive disorder with Lewy bodies. REM sleep behavioral disorder and excessive sensitivity to neuroleptic agents are “suggestive diagnostic features”; low dopamine transporter uptake in basal ganglia is a diagnostic marker but is not included in the diagnostic criteria.
This disorder is characterized by dream-enacting behaviors during REM sleep, potentially involving complex or violent movements, with individuals typically having a clear memory of the dream content upon awakening.
What is REM sleep behavior disorder?
This 'religious' group is a main part of the anti-psychiatry movement.
What is Scientology?
The formerly used diagnosis of the schizophrenia with predominant negative symptoms and abated to mild positive symptoms remaining after the initial psychotic break and episodes.
What is residual type schizophrenia?
True or false: Pupillary constriction is a reliable sign of an opioid overdose?
What is false?
Severe OD w/ anoxia can create physiological stress and pupillary dilation.
This neurocognitive disorder (NCDs) is especially characterized by deficits in domains such as speech production, word finding, object naming, or word comprehension, whereas episodic memory, perceptual-motorabilities, and executive function are relatively preserved?
A. Major or mild NCD due to Alzheimer’s disease.
B. Major or mild NCD with Lewy bodies.
C. Major or mild vascular NCD.
D. Behavioral-variant major or mild frontotemporal NCD.
E. Language-variant major or mild frontotemporal NCD.
What is, E. Language-variant major or mild frontotemporal NCD.?
Explanation: Major or mild frontotemporal NCD comprises a number of syndromic variants characterized by the progressive development of behavioral and personality change and/or language impairment. The behavioral variant and three language variants (semantic, agrammatic/nonfluent, and logopenic) exhibit distinct patterns of brain atrophy and some distinctive neuropathology.
The criteria must be met for either the behavioral or the language variant to make the diagnosis, but many individuals present with features of both.
Individuals with language-variant major or mild frontotemporal NCD present with primary progressive aphasia with gradual onset, with three subtypes commonly described: semantic variant, agrammatic/nonfluent variant, and logopenic variant, and each variant has distinctive features and corresponding neuropathology. Individuals with behavioral-variant major or mild frontotemporal NCD present with varying degrees of apathy or disinhibition. They may lose interest in socialization, self-care, and personal responsibilities, or display socially inappropriate behaviors. Insight is usually impaired, and this often delays medical consultation. The first referral is often to a psychiatrist. Individuals may develop changes in social style, and in religious and political beliefs, with repetitive movements, hoarding, changes in eating behavior, and hyperorality. In later stages, loss of sphincter control may occur. Cognitive decline is less prominent, and formal testing may show relatively few deficits in the early stages.
Common neurocognitive symptoms are lack of planning and organization, distractibility, and poor judgment. Deficits in executive function, such as poor performance on tests of mental flexibility, abstract reasoning, and response inhibition, are present, but learning and memory are relatively spared, and perceptual motor abilities are almost always preserved in the early stages.
This specific type of circadian rhythm disorder is common among adolescents who have a natural tendency for later sleep onset and wake times.
What is delayed sleep phase syndrome (or disorder)?
The use of this medication was discovered in 1948 by Australian psychiatrist John Cade, who was testing its effects in guinea pigs and then on himself and patients. He noticed it had a calming, anti-manic effect. Although it had been used in ancient Greek medicine (via mineral water) and as a nineteenth-century gout treatment, its potential as a psychiatric treatment was a modern, accidental discovery.
What is lithium?
All of the 5 major negative symptoms start with "A" and the rest can be remembered with A words o phrases. This one means "A lack of motivation and energy, making it difficult to start or complete goal-directed activities."
What is avolition?
This personality disorder has the highest prevalence among individuals with cannabis use disorder.
A. Obsessive-compulsive personality disorder.
B. Paranoid personality disorder.
C. Schizotypal personality disorder.
D. Borderline personality disorder.
E. Antisocial personality disorder.
F. Cannabis induced personality disorder
What is E, ASPD?
Per the DSM5 handbook -
Antisocial personality disorder is the most prevalent (30%) personality disorder among individuals with cannabis use disorder, followed by obsessive-compulsive personality disorder (19%) and paranoid personality disorder (18%).
This medication is FDA-approved for psychosis in Parkinson's disease and is being studied for dementia-related psychosis, notes the Lewy Body Dementia Association.
What is Pimavanserin (Nuplazid)??
It works by acting as an inverse agonist and antagonist at serotonin 5-HT2A and, to a lesser extent, 5-HT2C receptors. Unlike many antipsychotics, it has no appreciable activity at dopamine D2 receptors, which is a key aspect of its mechanism of action. Its precise mechanism in treating hallucinations and delusions in Parkinson's disease psychosis is not fully understood.
An 80-year-old man has a history of myocardial infarction and had coronary artery bypass graft surgery 8 years ago. He plays tennis three times a week, takes care of his grandchildren 2 afternoons each week, generally enjoys life, and manages all of his activities of daily living independently; however, he complains of excessively early morning awakening. He goes to sleep at 9:00 P . M . and sleeps well, with nocturia once nightly, but wakes at 3:30 A . M . al- though he would like to rise at 5:00 A . M . He does not endorse daytime sleepi- ness as a problem. His physical examination, mental status, and cognitive function are normal. This is the most likely sleep-wake disorder diagnosis:
A. Insomnia disorder.
B. Rapid eye movement (REM) sleep behavior disorder.
C. Restless legs syndrome.
D. Obstructive sleep apnea hypopnea.
E. The man is a short sleeper, which is not a DSM-5 diagnosis
What is E?
This, the world's first antipsychotic drug, was initially investigated in 1949 by a French military surgeon, Henri Laborit, as an antihistamine to reduce surgical shock. He found it had strong psychological effects and convinced a colleague to try it on a schizophrenic patient in 1952. Its dramatic success ushered in the era of modern psychopharmacology.
What is chlorpromazine/Thorazine? 
The 5 "A" main negative symptoms of schizophrenia are: Affective flattening (blunted or flat affect), Alogia (poverty of speech), Anhedonia (inability to feel pleasure), Avolition (reduced motivation), and this term meaning a lack of social interaction leading to social withdrawal.
What is asociality?
Emotional and social symptoms
- Affective flattening: A reduced or absent outward display of emotions, such as limited facial expressions, gestures, and changes in speech tone.
- Asociality: A lack of interest in social relationships and a preference for being alone.
- Autistic interaction: Difficulty forming and maintaining relationships with others.
Motivational and behavioral symptoms
- Anhedonia: The inability to experience pleasure from activities that are typically enjoyable.
- Avolition: A lack of motivation and ability to complete goal-oriented tasks.
- Apathy: A general lack of interest or enthusiasm.
- Amotivtion/Lack of spontaneity: Difficulty with social interactions and a reduced ability to think or act independently.
Communication symptoms
- Alogia: Poverty of speech, meaning reduced speech output or answers that are very brief and uninformative. In severe cases, this can include a complete lack of speech.
Other associated symptoms
Difficulty with personal hygiene, Trouble sleeping, and Reduced interest in hobbies or work.
-Awful hygiene
-At it all night.
-Autistic interests (focused, limited interests).
This newer antipsychotic is novel in having two active ingredients: The first is a muscarinic agonist that selectively targets M1 and M4 receptors in the brain without blocking D2 receptors. The second's MOA is a muscarinic antagonist that blocks the muscarinic receptors primarily in the peripheral tissues to limit adverse effects.
What is Cobenfy (xanomeline-trospium)?


Cognitive agents have excellent evidence for helping w/ various neuropsychiatric symptoms of dementia. When we are presented with agitation/impulsivity and behavioral issues, this class of medications and this specific medication have the strongest evidence and tolerability.
Of the larger group mentioned, this one is less studied but has less of an effect on the QTc and a relatively favorable interactive profile compared to the other agents remaining in the class.
What are SSRIs and trazodone?
The SSRI is sertraline.
Es/citalopram are more studied but affect the QTc. If the QTc is not an issue, escitalopram has the better profile re interactions w/ other meds.
Sleep terrors and sleepwalking fall under this specific non-REM sleep category in the DSM-5.
What are non-REM sleep arousal disorders?
Subtypes of sleepwalking include sleep related eating and sexual behaviors.
"Confusional arousals" are an incomplete awakening from sleep with apparent confusion and a lack of responsiveness to others. It is mentioned in the DSM5 but included as a diagnosis. It is included in the International Classification of Sleep Disorders.
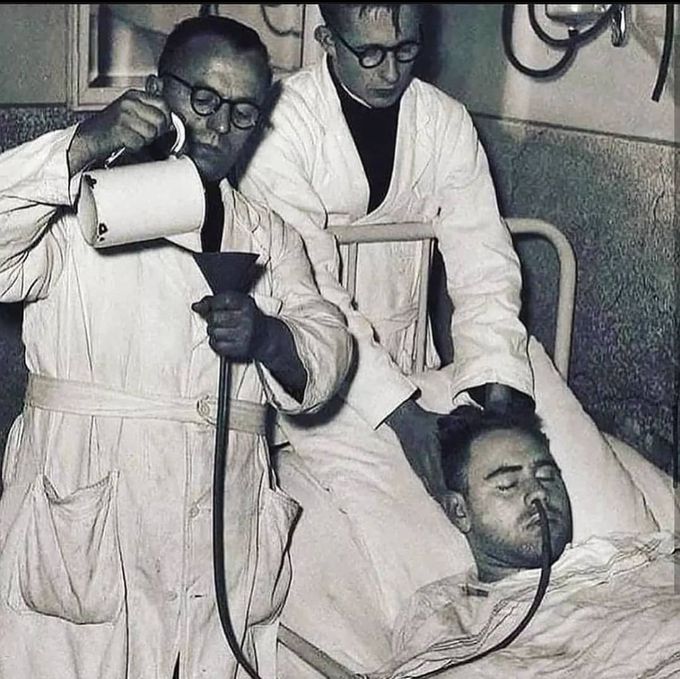
Treatment seen here:
What is insulin shock therapy?
Here, they are pouring a glucose solution via an NG tube to reverse the effect.
"Insulin shock therapy or insulin coma therapy was a form of psychiatric treatment in which patients were repeatedly injected with large doses of insulin in order to produce daily comas over several weeks.[1] It was introduced in 1927 by Austrian-American psychiatrist Manfred Sakel and used extensively in the 1940s and 1950s, mainly for schizophrenia, before falling out of favor and being replaced by neuroleptic drugs in the 1960s."
T or F: Negative symptoms are considered a good prognostic feature.
What is false?
"They are associated with a poorer quality of life, more impairment in daily functioning, and are more persistent and resistant to treatment compared to positive symptoms like hallucinations. They can predict long-term occupational and social difficulties."