Isolated cleft palate is more likely to be __________ (syndromic versus non-syndromic) compared to cleft lip and palate.
Isolated cleft palate is more likely to be syndromic compared to cleft lip and palate.
In syndromic cleft, the incidence of isolated cleft palate is ~42% (vs ~14% cleft lip and palate).
Cleft palate results from failed fusion of the __________.
Cleft palate results from failed fusion of the palatal shelves.
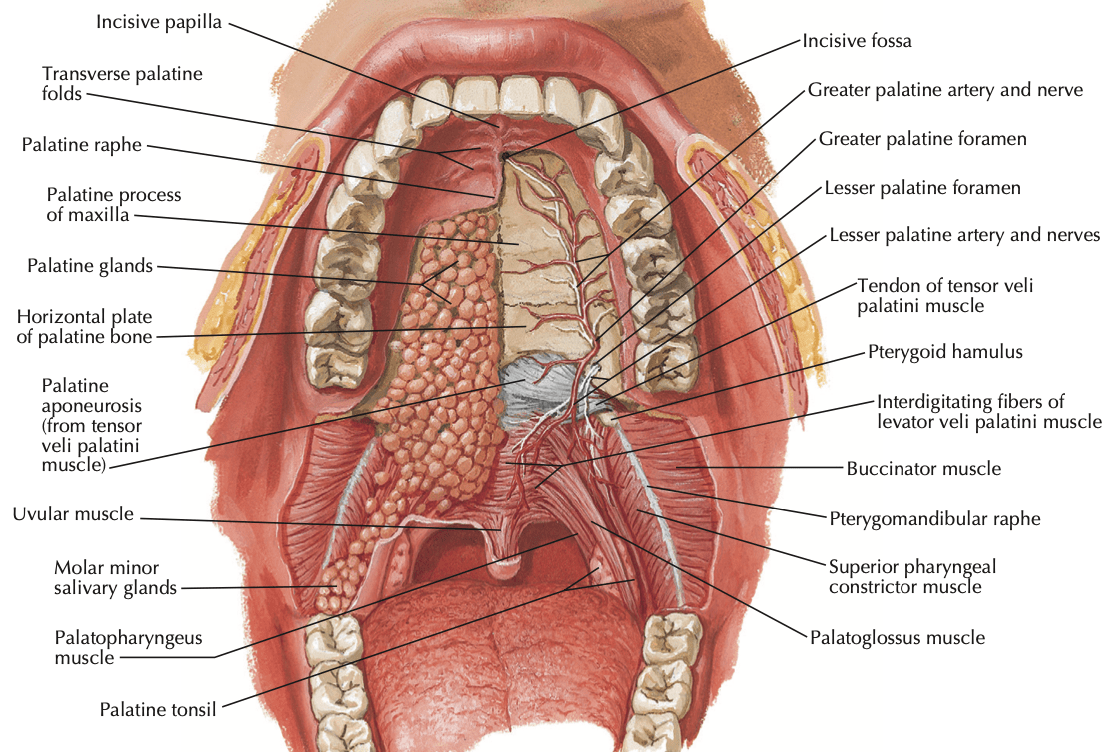
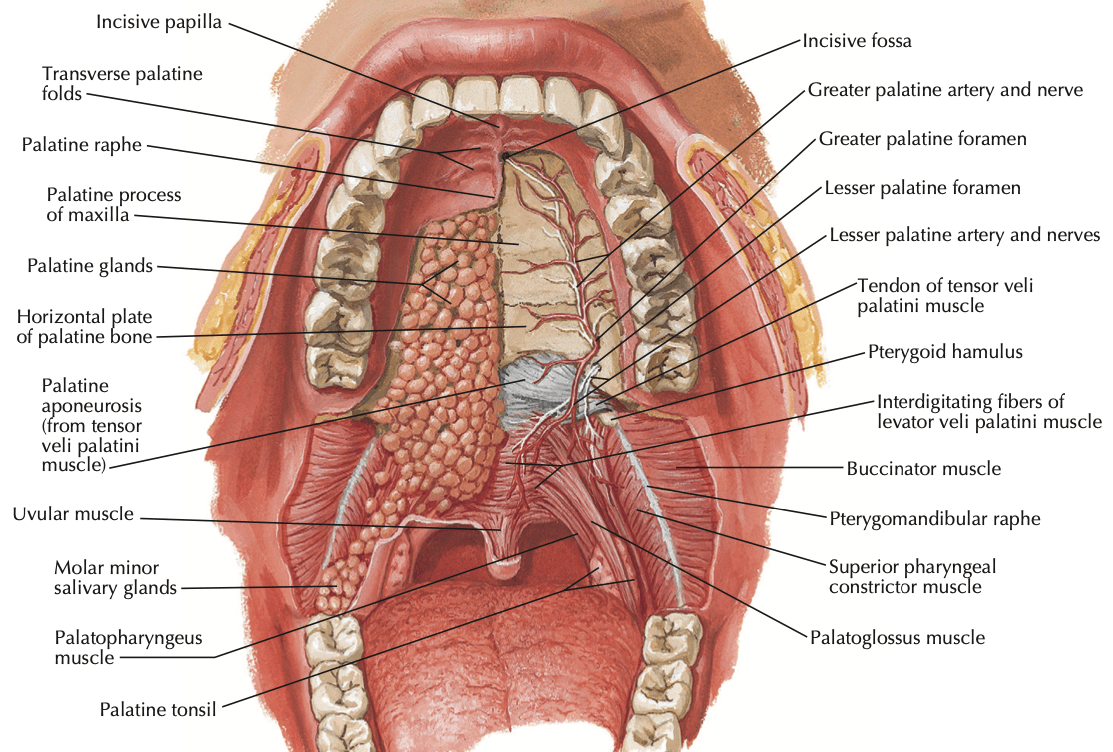
What runs through the greater palatine foramen?
Greater palatine artery, vein, and nerve
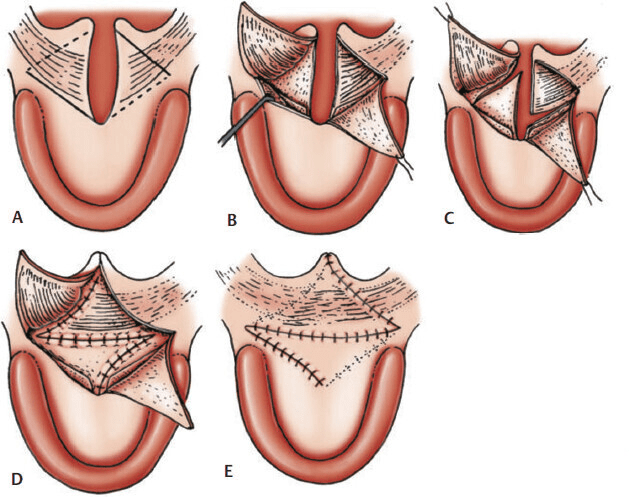
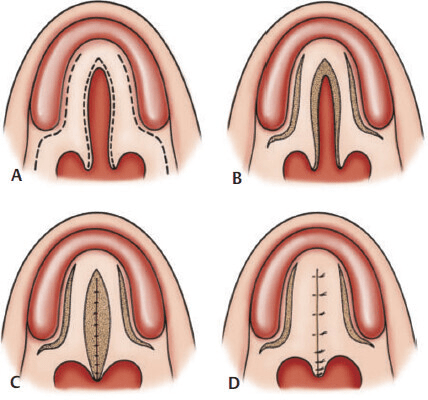
Which classic palatoplasty techniques increase palate length?
Furlow double-opposing Z-plasty (lengthens soft palate)
Veau-Wardill-Kilner (V-Y pushback)
Explain the Veau classification.
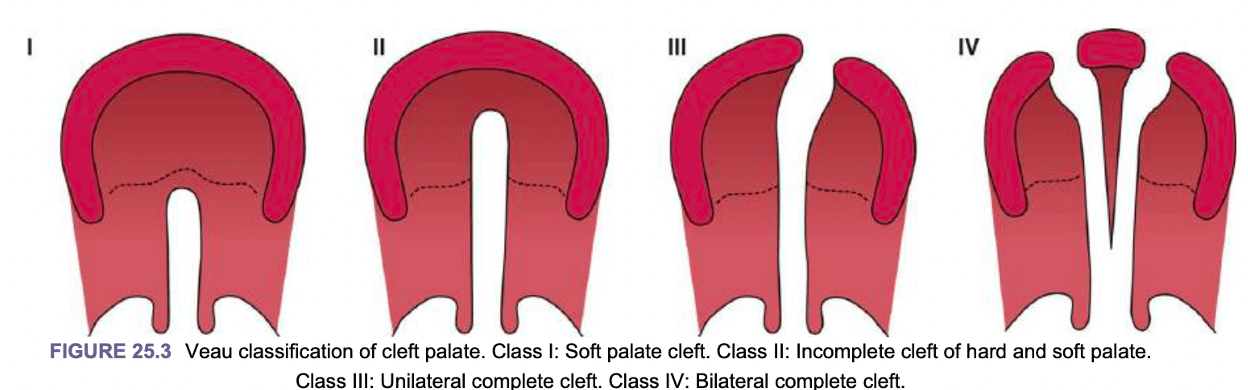 Class I - Soft palate only
Class I - Soft palate only
Class II - Incomplete, through hard and soft palate to the incisive foramen
Class III - Unilateral complete cleft
Class IV - Bilateral complete cleft
Explain the Pierre-Robin sequence.
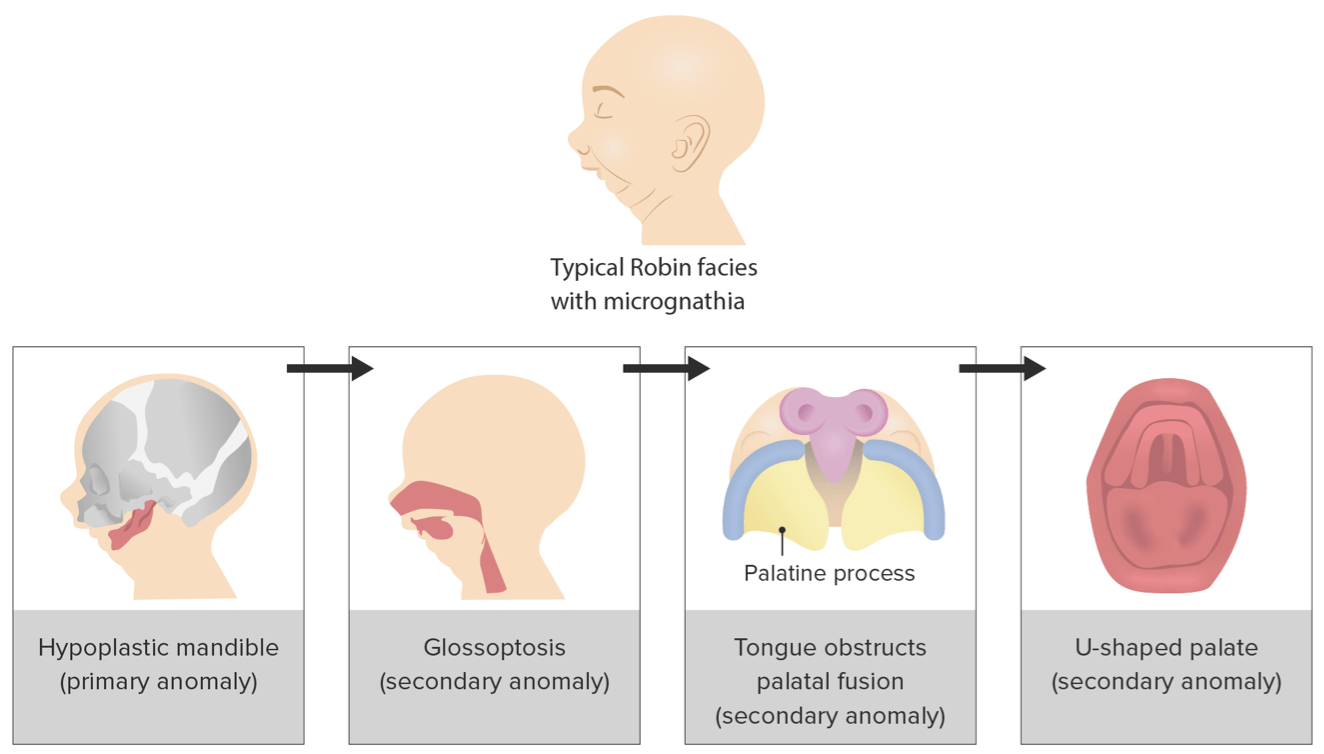
Micrognathia/retrognathia -> glossoptosis -> airway obstruction +/- cleft palate
Cause not fully understood, can be due to isolated genetic mutation or syndrome (eg. Stickler syndrome)
The primary palate forms at ______ weeks gestation, with secondary palate forming at ______ weeks gestation.
The primary palate forms at 4-7 weeks gestation, with secondary palate forming at 5-12 weeks gestation.
The __________ separates the primary palate from the secondary palate.
The incisive foramen separates the primary palate from the secondary palate.
A patient presents with a Veau class I cleft. What are the options for repair?
Intravelar veloplasty (IVV)

Furlow double-opposing Z-plasty
List the triad for a submucous cleft palate.
Bifid uvula, notching of the posterior hard palate, zona pellucida (midline mucosal attenuation)
A 2-year-old boy who was recently adopted is brought to the office for evaluation and treatment of cleft of the lip and palate. Physical exam demonstrates an isolated cleft palate and lower lip pitting. What is the patient's risk of having a child with same condition?
50%. This patient has Van der Woude syndrome, caused by mutation in IRF-6 and inherited in an autosomal dominant fashion. It is characterized by lower lip pitting with CL/P or isolated CP.
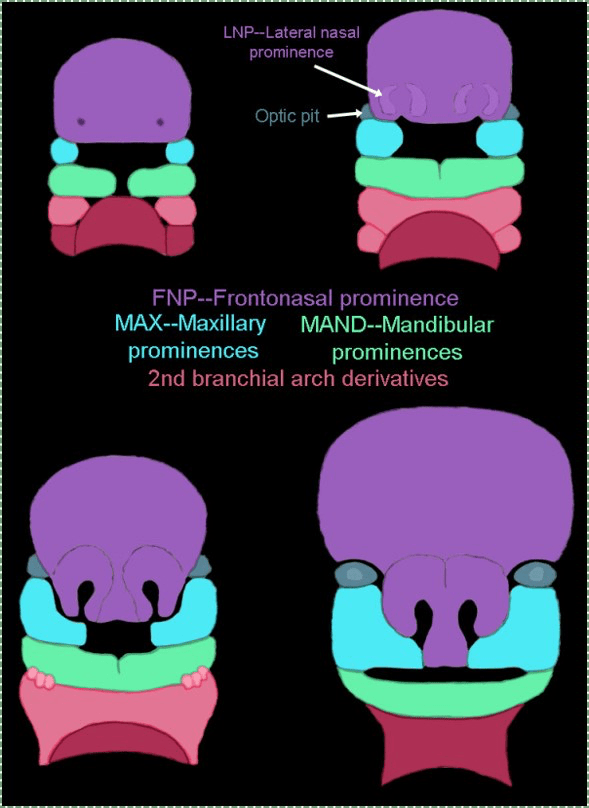
Which pharyngeal arch(es) are the frontonasal, maxillary, and mandibular prominences derived?
First (and second per G&S)
Name the 5 traditional muscles of the soft palate and their innervation.
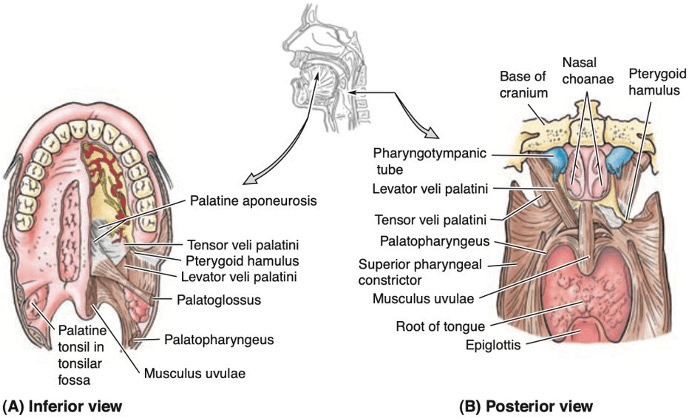
Levator veli palatini, palatopharyngeus, palatoglossus, musculus uvulae - all innervated by CN X
Tensor veli palatini - CN V3
Other muscles of the velum include superior pharyngeal constrictor (X), salpingopharyngeus (CN X), stylopharyngeus (CN IX)
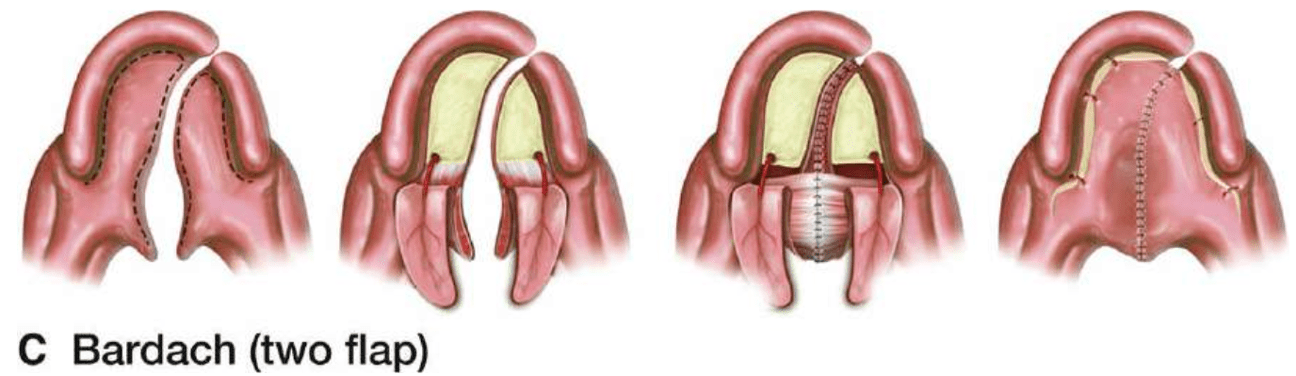
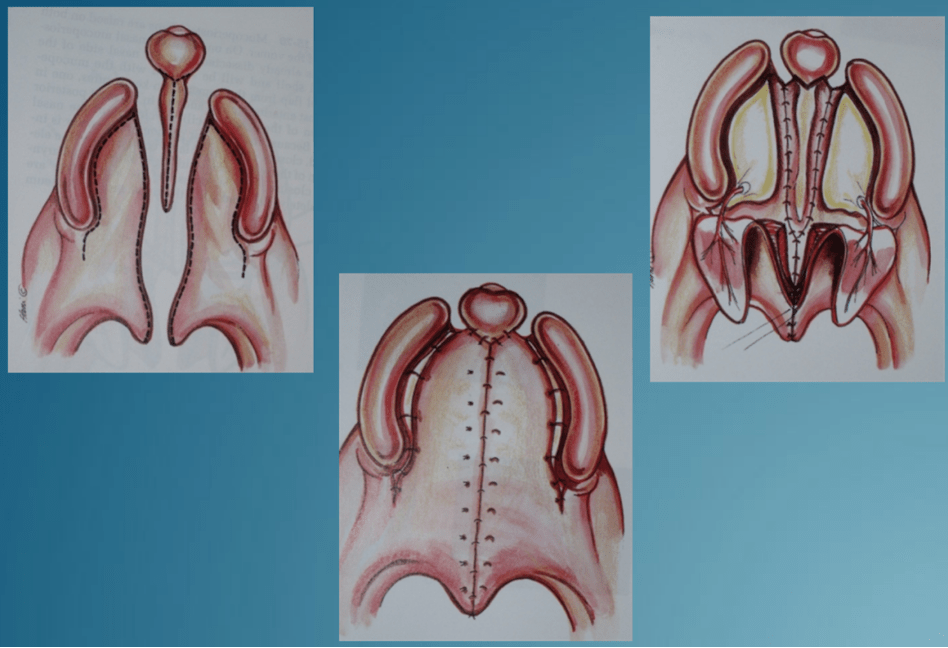
A patient presents with a bilateral complete cleft. What are your options to for repair?
Bardach 2-flap palatoplasty + vomer flap
Why do kiddos with cleft palate develop recurrent ear infections?
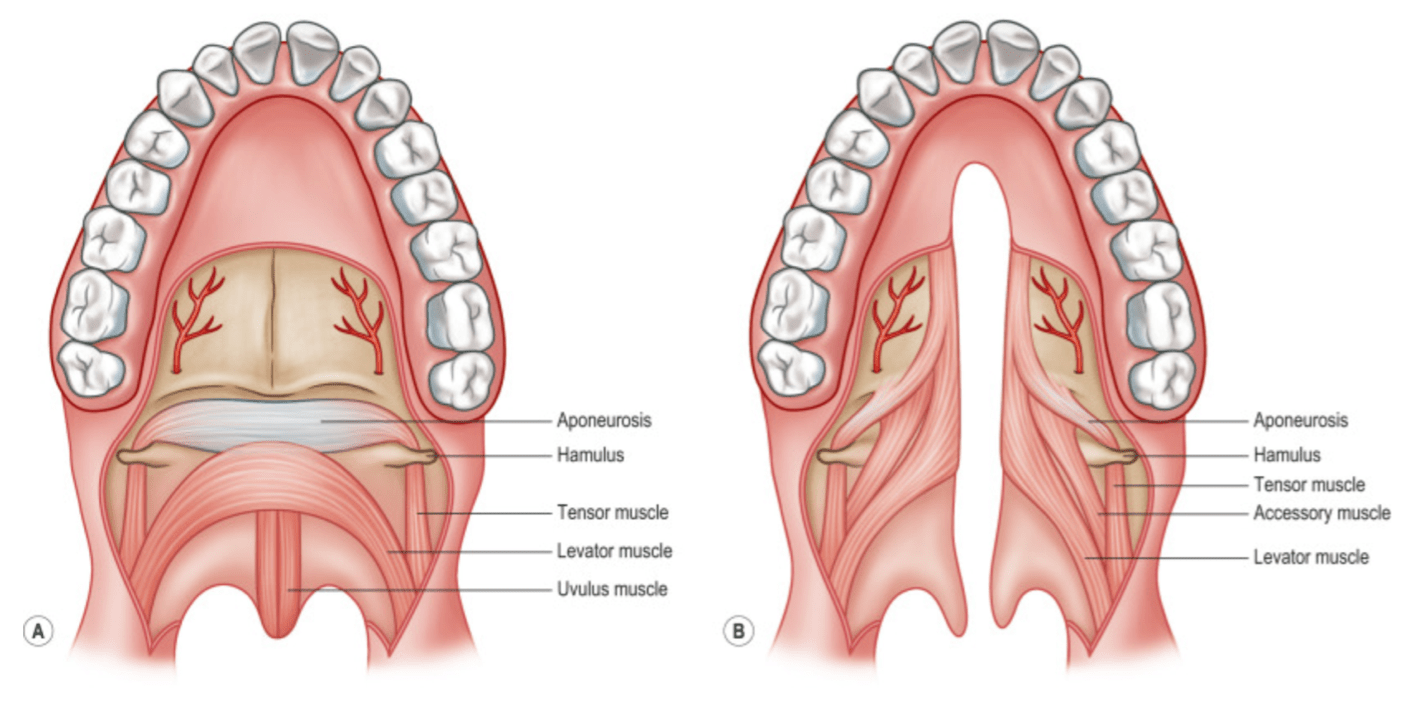
Anomalous insertion of levator veli palatini onto the posterior margin of the hard palate leads to poor venting and decreased drainage of the middle ear, resulting in recurrent ear infections (and thus why kiddos with cleft palate get ear tubes, often at the same time as cleft palate repair).
What is the gender distribution for isolated cleft palate? What is the ongoing theory for this?
Male/female 1:2; palatal fusion is delayed in females (by roughly 1 week)
Explain the formation of the primary and secondary palates, including which prominences they primarily derive from.
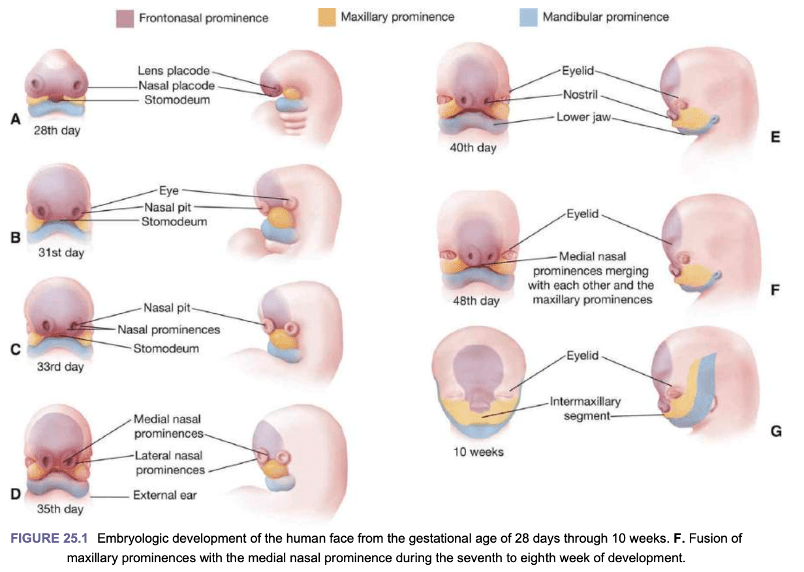
Primary palate: Medial nasal prominences (of the frontomaxillary prominence) migrate and fuse to form the intermaxillary segment, which then fuses with the maxillary prominence
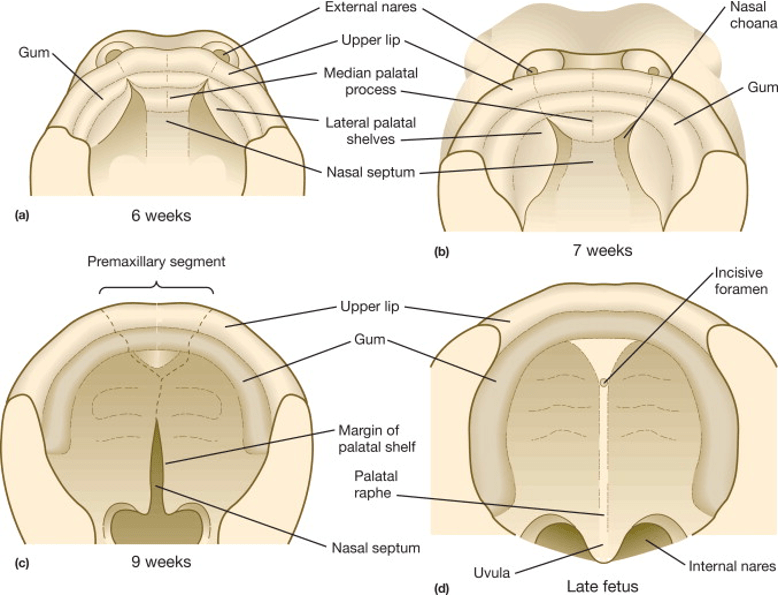
Secondary palate: Lateral palatal shelves of the maxillary prominence migrate and fuse medially
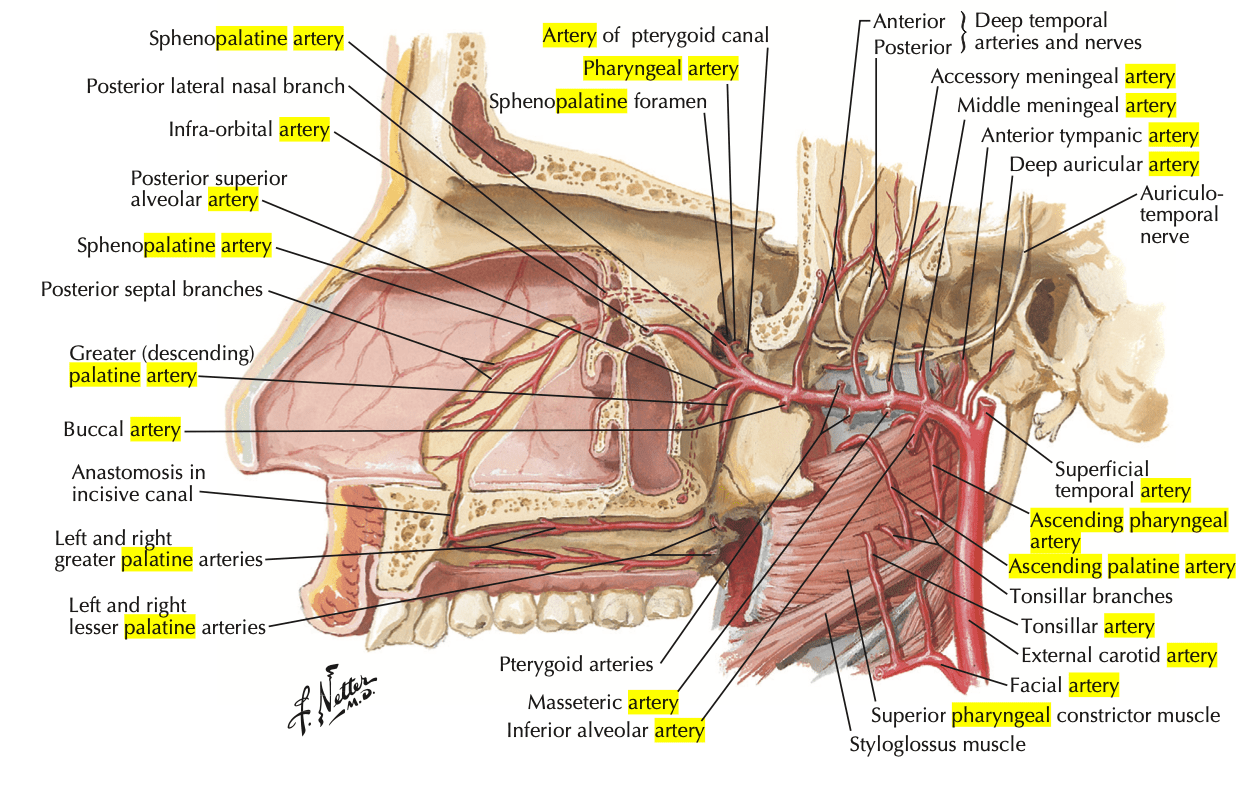
In hard palate palatoplasty, flaps are typically based on the __________.
Name the vessels it is derived from (all the way to external carotid artery ).
In hard palate palatoplasty, flaps are typically based on the greater palatine artery.
Greater palatine artery <- descending palatine artery <- maxillary artery <- external carotid artery
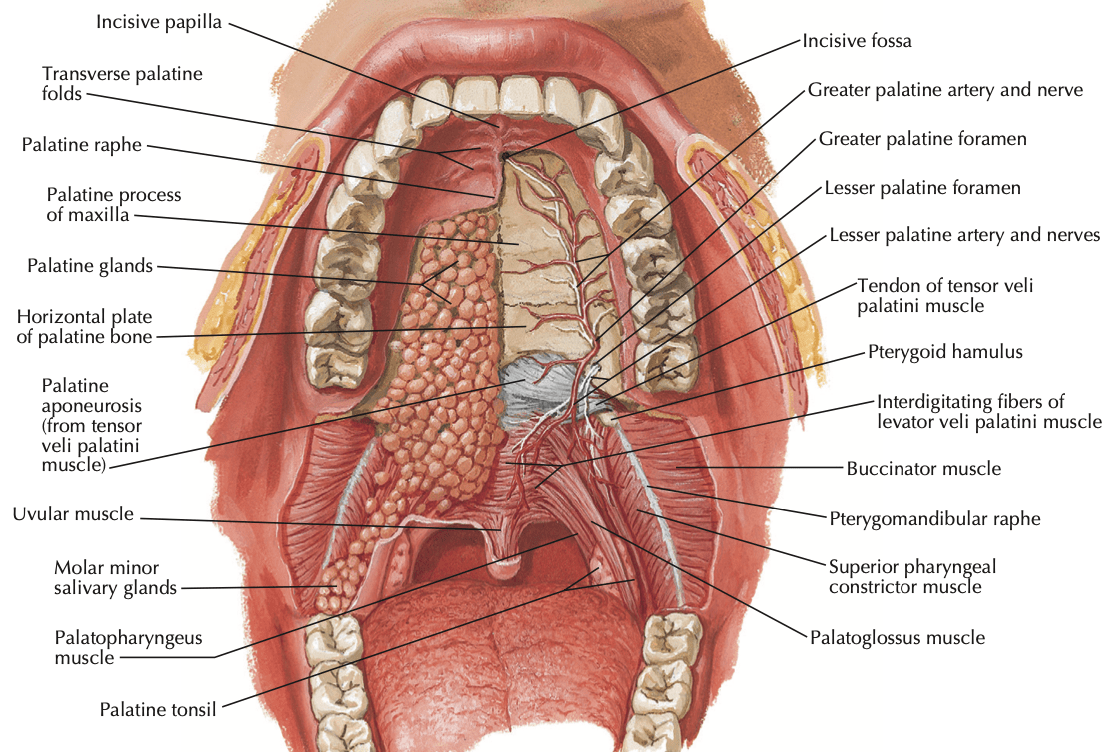
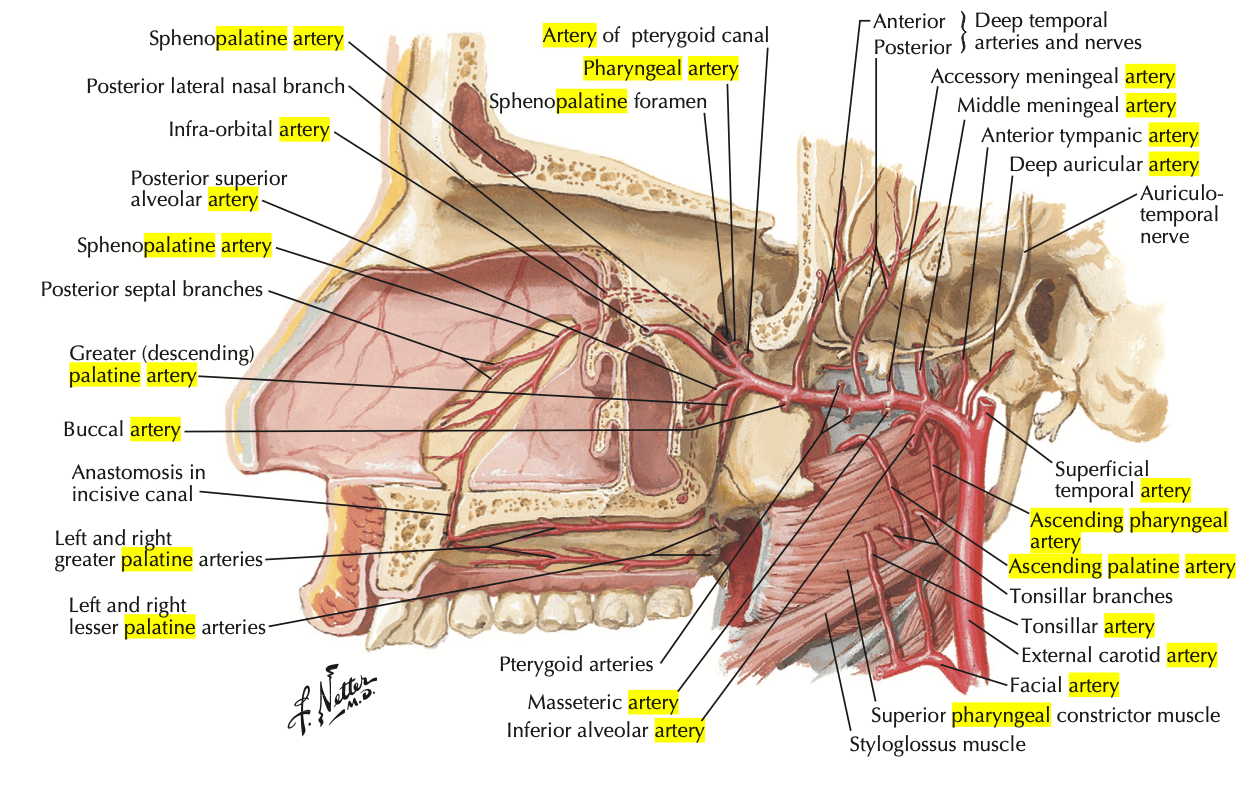
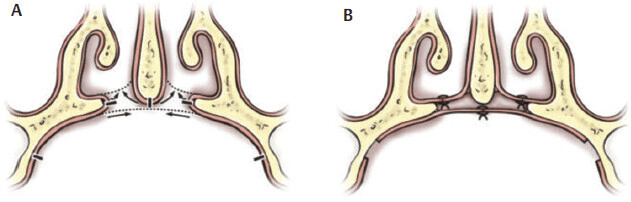
Which hard palate repair technique is typically bipedicled? What are its pedicles?
Von Langenback palatoplasty, based on the greater palatine artery posterior and sphenopalatine artery anteriorly
At what age does primary cleft palate repair typically happen? (Bonus points for why)
9-12 months
Early correction (<12 months) enables improved speech, but adversely affects maxillary growth; late correction (> 12 months) allows for uninterrupted maxillary growth, but impacts speech
An 8-year-old girl presents to the ophthalmologist for evaluation of myopia. She has history of cleft palate repair, thought to be secondary to Pierre-Robin sequence, as well as scoliosis. She has a flat face and a long chin. Her mother is similar in appearance. What syndrome do they most likely have and what is it caused by?
Stickler syndrome, an autosomal dominant inherited syndrome caed by a mutation in type 2 collagen
Characterized by Pierre-Robin sequence, eye abnormalities, hearing loss, and joint problems
Which side (right vs left) tends to have more clefts and why?
Left; right lateral palatal process becomes more horizontal before the left process, increasing risk of a left-sided cleft
What runs through the incisive foramen?
Sphenopalatine artery and vein, nasopalatine nerve
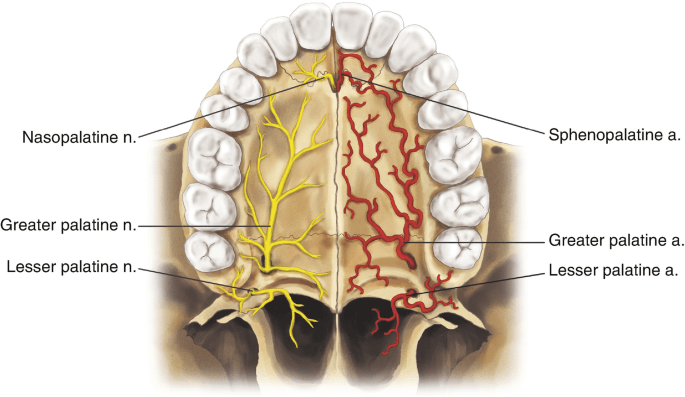
You accidentally divide the greater palatine artery pedicle during dissection of one side for a Bardach two-flap palatoplasty, but Mancho isn't worried. What else can the flap survive on?
Posterolateral supply from the lesser palatine artery, ascending pharyngeal artery, and ascending palatine artery
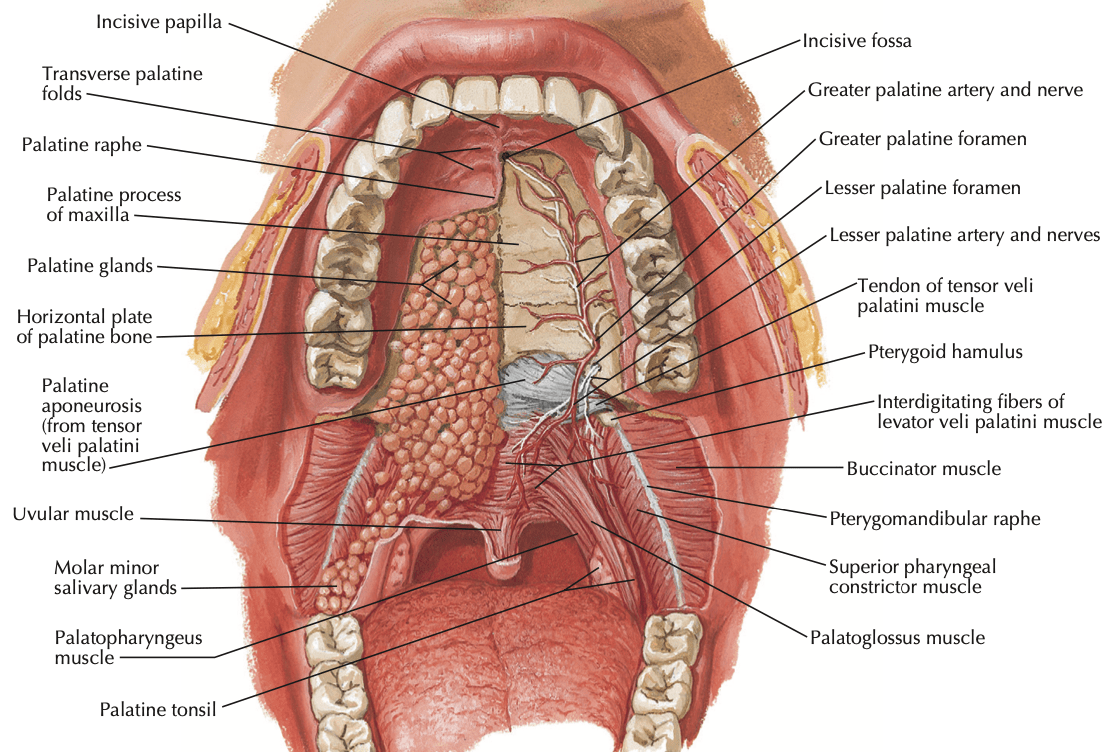
Name 2 maneuvers used to address wide clefts during palatoplasty.
Straight-line closure (instead of Z-plasty)
Additional hard palate mucoperiosteal undermining
Infracturing of the hamulus (brings lateral elements toward midline)
Osteotomy of the greater palatine foramen (increases pedicle length)
Meticulous dissection of the periosteal sheath around the pedicle (also increases pedicle length)
If doing Z-plasty, place incisions more posteriorly (less anchored to bony hard palate, buccal mucosa laxity increases mobility)