What term described the development of a lipid filled inflammatory plaque in an artery wall?
Atherosclerosis
CTAs and MRAs are preferred over US when diagnosing this condition. Why?
Aortoiliac disease.
US is obscured by bowel gas.
When is an angioplasty considered for pts with renal artery stenosis?
if >70% blocked, flash pulmonary edema/volume overload, acei/arb intolderance, acute kidney injury, transplanted kidney artery stenosis.
Which arrythmias are shockable?
pulseless Vtach (monomorphic and polymorphic) and vfib
Describe peripheral artery disease
Systemic atherosclerosis of non-cardiac, non cerebral arteries.
What is the gold standard for treating aortoiliac disease?
Aortofemoral bypass surgery
Most occlusive CVD occurs from where?
If arterial in origin, where is it most likely from?
cardiac emboli
carotid artery
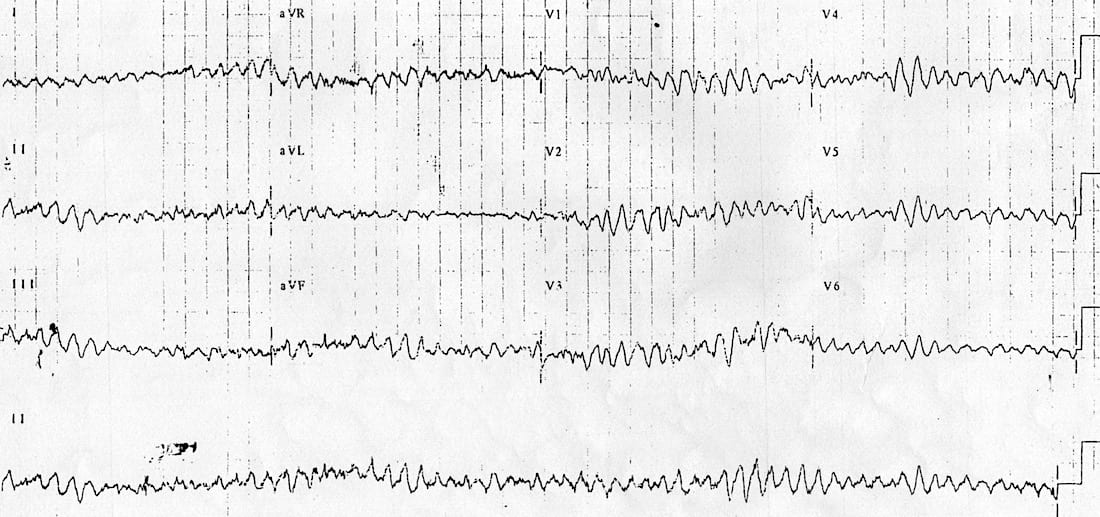
What is this rhythm defined by no identifiable p waves, QRS complexes, or T waves?
Ventricular fibrillation
PAD is a systemic marker for atherosclerosis and has a high correlation with these conditions
Coronary artery disease, cerebrovascular disease
What is the most common PAD site and its signs and symptoms
femoral and popliteal PAD - calf claudication, reduced popliteal/pedal pulses, rest pain, ischemic ulcers, skin/hair changes, and muscle atrophy
What's the difference between TIA and stroke?
Sudden deficits lasting <24 hrs vs >24 hrs
Which condition requires BBs/mexiletine along with the implantation of an AICD to treat?
Why is this necessary for this condition?
Long QT syndrome
-high likelihood of turning into Torsades Vtach, requiring defibrillation.
PAD is often segmental, meaning that lesions occur in discrete arterial regions, not diffusely. What are some common sites of atherosclerosis?
aortoiliac, femoral-popliteal, tibial-pedal

The photo shows a classic sign of advanced ischemia. What is this called?
Dependent rubor and pallor with elevation
If anterior circulation is disturbed due to an occlusion of a carotid, what symptoms might be observed?
focal motor/sensory deficits, aphasia
What factors define an unstable patient?
Systolic BP <90
AMS
Chest pain
These areas of PAD are less common but have higher mortality
thoracoabdominal arteries such as renal arteries, celiac, superior mesenteric, inferior mesenteric
Tibial and pedal PAD is primarily found in pts with this comorbidity.
What are some signs/symptoms related to tibial and pedal PAD?
Diabetes
Forefoot rest pain (pain when supine, none when standing), painful ischemic ulcers, absent pedal pulses, dependent rubor.
With a retinal embolus, what would the pt experience?
amaurosis fugax, transient monocular blindness
All pts that are hemodynamically unstable receive this treatment as first line management
Synchronized cardioversion
PAD is much ______ common in upper extremities.
less
How can you differentiate between diabetic neuropathic ulcers and ischemic ulcers?
Painless vs painful ulcerations
Dizziness, visual distubances, and ataxia might be observed in a pt an occlusion in this region.
vertebrobasilar, affecting the posterior circulation
Describe the management flow of a stable pt with monomorphic vtach.
1. vagal maneuver
2. adenosine
3. procainamide or amiodarone
4. synchronized cardioversion
Smoking, DM, HTN, age, AA decent, and dyslipidemia
Which diagnostic tests are preferred in Tibial/pedal PAD?
Toe brachial index
Digital subtraction angiography is gold standard imaging for this diagnosis
Occlusive CVD management depends on the severity of stenosis and whether the pt is symptomatic.
How do we manage pts with no symptoms and <60% occusion?
What about pts that are symptomatic with >70% occlusion?
Risk factor modification, statins, antiplatelet therapy. Consider CEA or stent is there's a low intevrentional risk.
Carotid enterectomy (CEA) or stent in select cases.
What term is used to describe wide complex tachycardia with changing QRS complexes?
How do we treat this in a stable vs unstable pt?
Magnesium sulfate if stable, then implantation of AICD
Defib if unstable
Describe the typical progression of PAD
Asymptomatic -> intermittent symptoms (pain, weakness) -> symptoms at rest with skin and hair changes -> end organ damage.
How would one manage Tibial/pedal disease?
Amputation if untreated.
Vein bypass revascularization is preferred over stenting.
The only effective treatment for thromboangiitis obliterans
What medication is injected into affected tissue to help treat ulcers in this disease?
absolute smoking cessation
prostacyclin analogs
PVCs are treated with these medications
Is there a p wave in a PVC? Why or why not?
BBS, CCBs
No p wave because the beat arises from an ectopic site in the ventricles
How do you diagnose PAD?
Take the highest systolic pressure of the two ankle arteries and divide that by the systolic pressure at the brachial artery to get your ABI number.
Acute arterial occlusions are emergencies that occur due to what?
What are the clinical features of an acute artery occlusion?
A cardiac or arterial embolus that gets lodged in a smaller vessel downstream.
Pain, pulselessness, pallor, poikilothermia, paresthesia, paralysis
An inflammatory and thrombotic disease found predominantly in young men who smoke heavily.
Thromboangiitis obliterans (Buerger Disease)
A normal ABI is .9-1.4
>1.4 indicates?
.5-.8 indicates?
<.5 indicates?
Calcification/Hardening of arteries
Moderate PAD
Severe PAD
Ischemia due to __________ is usually less severe and abrupt due to its chronic nature and compensation via collateral neovascularization.
thrombosis
> or equal to 3cm infrarenal aorta that often involves the iliac bifurcation, mostly seen in older M smokers.
abdominal aortic aneurysm
What is occurring in the arteries and distal tissue if a patient has an ABI of <.5 at the ankle?
The tissue below the ankle is experiencing chronic ischemia and end organ damage due to the severe occlusion of the ankle arteries.
How do you confirm acute arterial occlusion and how would you treat it?
US doppler to confirm absent pulse
Immediate IV heparin
Imaging via angiography if there is time, but do not delay revascularization via thrombectomy, thrombolysis, or bypass.
Amputation is ischemic is irreversible.
A pt coming in with a known AAA has pain and tenderness in his abdomen. You notice a pulsating mass when you go in for a physical exam. How would we treat this patient?
Send for EVAR (endovascular aneurysm repair): lower mortality in open aneurysm repairs.
Or an open aneurysm repair.
First line treatment for PAD is lifestyle changes such as smoking cessation and exercise therapy.
Medical management includes what kinds of medications?
2. maximizing statins to reduce ruptures and further lipid accumulation
3. Adding cilostazol (PDE4 inhibitor with antiplatelet and vasodilator effects) helps with claudication pain
A pt presents to the ED with severe and steady abdominal pain. You perform a physical exam and note no severe tenderness or rebound tenderness upon abdominal palpation. Because of this, you rule out several GI issues such as cholecystitis, pancreatitis, and appendicitis. You look through your pts chart and see a history of uncontrolled Afib and hyperlipidemia. What is at the top of your differential and how would you treat?
Acute mesenteric ischemia
Emergent revascularization and bowel resection if needed.
How do we screen for an diagnose AAAs?
Once diagnosed, look for growth every 3 yrs if (3.0-3.9, yearly of 4.0-4.9, or every 6 months >5cm.)
Get a CT angiogrpahy for pre-op sizing at 5cm
If a pts PAD has progressed to end organ damage, revascularization must occur to save the tissue. What are two ways to achieve revascularization? List the pros and cons of both.
Surgical graft (autologous or synthetic bypass): more invasive surgery, not likely to reocclude.
Chronic mesenteric ischemia is much less common than acute and requires at least two of the three arteries to be diseased to produce symptoms. Name the arteries and the symptoms pts would experience with chronic mesenteric ischemia?
How would you treat this condition?
Celiac, superior mesenteric, inferior mesenteric
Postprandial abdominal pain, weight loss, "food fear"
Angioplasty/stent or bypass
Elective repair of AAAs are reserved for these pts
M: > or equal to 5.5cm
F: > or equal to 5cm
or rapid growth/symptomatic
A pt comes in with concerns of painful cramping and weakness in their calf muscles when walking upstairs. Upon physical exam, you notice their legs are shiny and hairless. You take off their shoes and notice several ulcers on the sides of their feet. What is at the top of your differential?
Chronic limb ischemia
A pt comes in with concerns of LLQ pain and tenderness upon exam. They state they've been experiencing bloody/mucus-y diarrhea x3 days. What is your suspected diagnosis and how might you diagnose and treat this condition?
Ischemic colitis
Flexible sigmoidoscopy, supportive treatment and monitoring for bowel perforation.
A pt comes in with chest and neck pain. They have complaints of increased hoarseness and difficulty swallowing. The patient has a history of smoking and emphysema. Upon CXR you notice a widened mediastinum. What is your top differential and next test to order for confirmation? What would you order in addition to the gold standard?
Thoracic aortic aneurysm
CTA to diagnose TAA
MRA to visualize and measure for impending repair.
A blockage in this arterial region typically presents with bilateral hip, buttocks, and thigh claudication along with erectile dysfunction and diminished femoral pulses or bruits
Aortoiliac Disease (Leriche syndrome)
There are two types of renal artery stenosis. What are they and who do they typically effect? Which is most common?
Atherosclerotic RAS - >45yrs, smokers, DM, HLD (80-90% of RAS)
Fibromuscular dysplasia - F <40yrs
What is the most common peripheral artery aneurysm?
What is a classic physical finding?
What imaging is diagnostic?
Popliteal > femoral
Pulsatile masses in femoral or popliteal region
US