Persistence of this specific aortic arch leads to the most common vascular ring anomaly seen in veterinary medicine.
Right 4th aortic arch
The Golden retriever, Boxer, and Newfie are 3 breeds predisposed to what congenital heart disease?
Subaortic stenosis
This is the most common device utilized for minimally invasive PDA occlusion.
ACDO (Amplatz Canine Duct Occluder)

Name the congenital defect shown here.
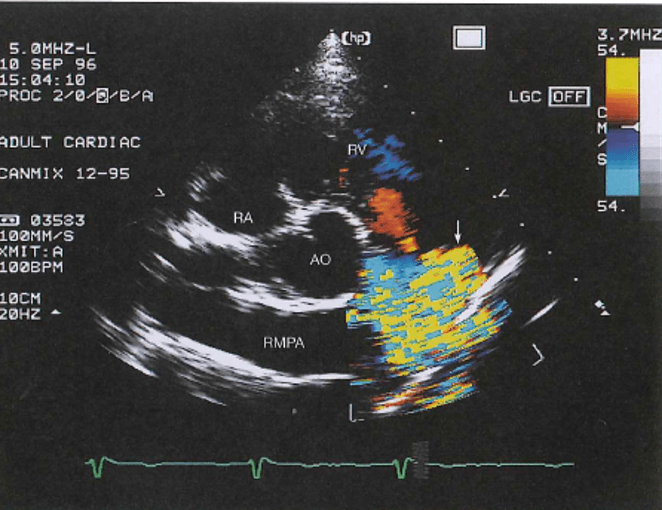
PDA
List the four components of Tetralogy of Fallot.
Large VSD
Over-riding aorta
Pulmonic stenosis/hypoplasia
Right ventricular hypertrophy
This adult structure is a result of a remnant of left cranial cardinal vein
Persistent L CrVC
This breed is the most common breed predisposed to tricuspid valve dysplasia.
100 bonus points if you can name the location of the genetic mutation of TVD in this breed.
Labrador retriever
Chromosome 9
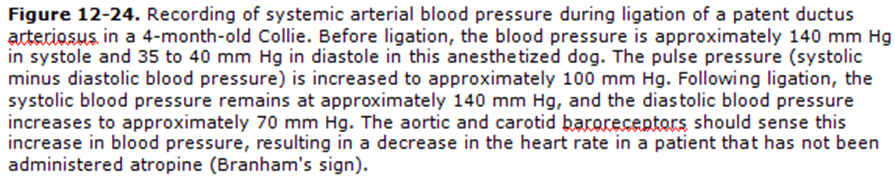
Explain Branham's sign.
When PDA ligated, systolic pressure stays same, but diastolic run-off is stopped, so diastolic pressure increases, resulting in smaller pulse pressure.
Baroreceptors sense increase in diastolic pressure and cause drop in heart rate
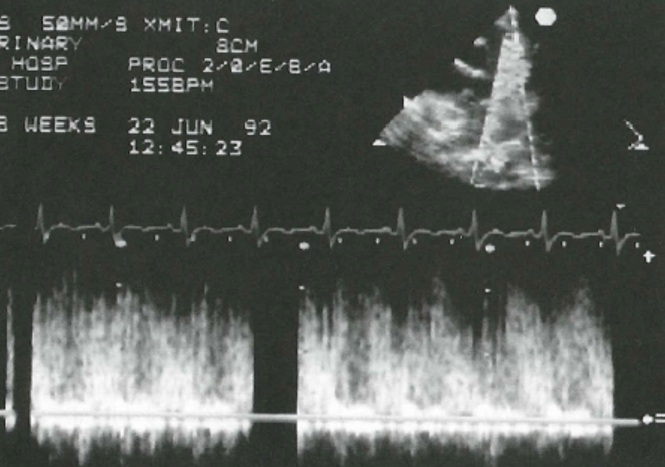
Describe the condition shown in the two images. Be specific.
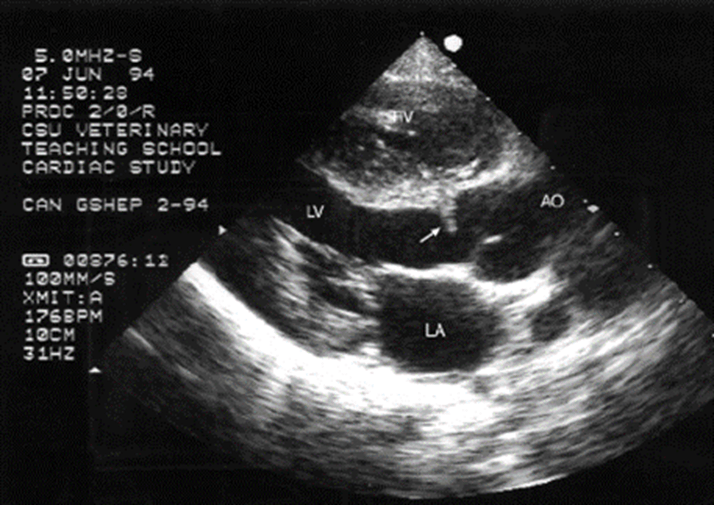
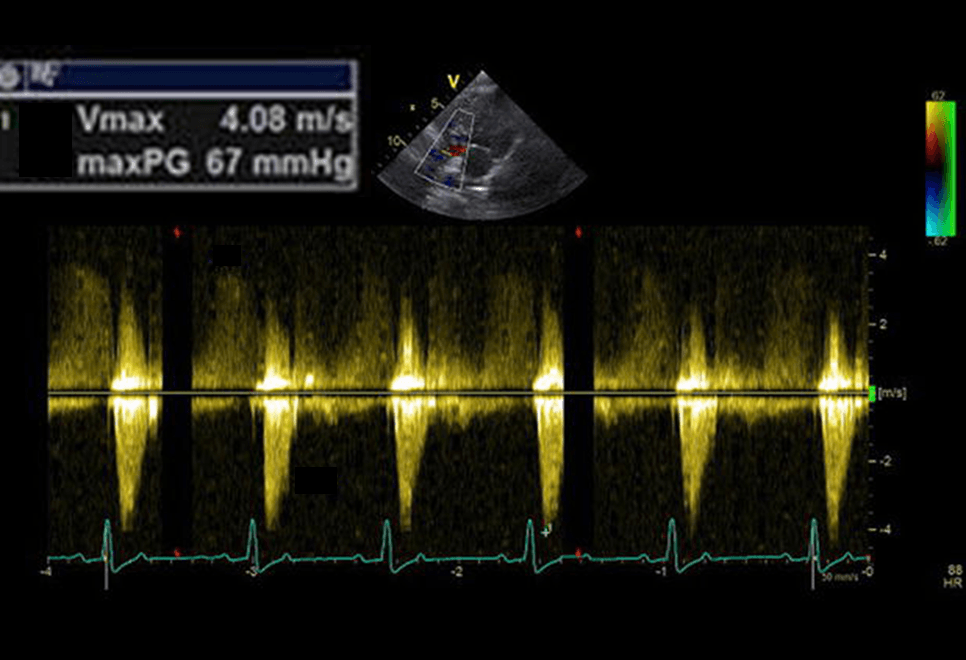
Subaortic stenosis (moderate)
Name 3 cyanotic congenital heart diseases
Tetralogy of Fallot, Truncus Arteriosus, Transposition of great arteries, Tricuspid atresia, any right to left shunt
Explain pathophysiology of PDA leading to heart failure.
Increased bloodflow through PDA, left heart, and pulmonary circulation (aorta --> PDA --> PA --> lungs --> LA --> LV --> aorta --> PDA...)
Volume overload and pulmonary overcirculation
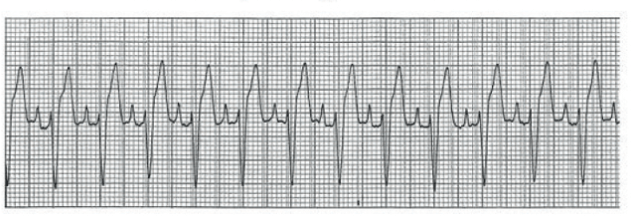
A one year old German Shepherd dog died suddenly while resting. What's your primary ddx?
Inherited ventricular arrhythmia of German Shepherd Dogs.
Typically "outgrow" the arrhythmia by ~ 2 yo
This ECG abnormality is expected to be seen transiently or permanently following what interventional procedure?
(What's the abnormality?)
PS balloon
Right bundle branch block
To confirm a R to L shunt on echo, this specific type of echo study can be performed
Bubble study!
Explain how polycythemia can result from chronic right to left shunting.
Kidney/liver stimulation due to hypoxemia --> EPO release --> increased RBC production
When assessing hemodynamic significance of a VSD, one can measure a Qp/Qs ratio on echo.
Qp/Qs is measured to be 0.8. What does this mean regarding the VSD?
Qp/Qs is a ratio of pulmonary blood flow compared to systemic blood flow. 1:1 means no shunting is present.
Bonus: Right to left shunting, as there is more systemic flow compared to pulmonary flow.
List the three structures that lead to most common aortic arch anomaly in dogs
persistent right aortic arch, left sided ductus arteriosus, and pulmonary artery
Provide 3 reasons to consider surgical ligation for PDA patients (rather than ACDO)
Patient is too small; patient's minimal ductal diameter is too big for ACDO; PDA morphology not accepting of ACDO
Describe the pressure tracing abnormalities and provide primary differential diagnosis. Be as specific as possible.
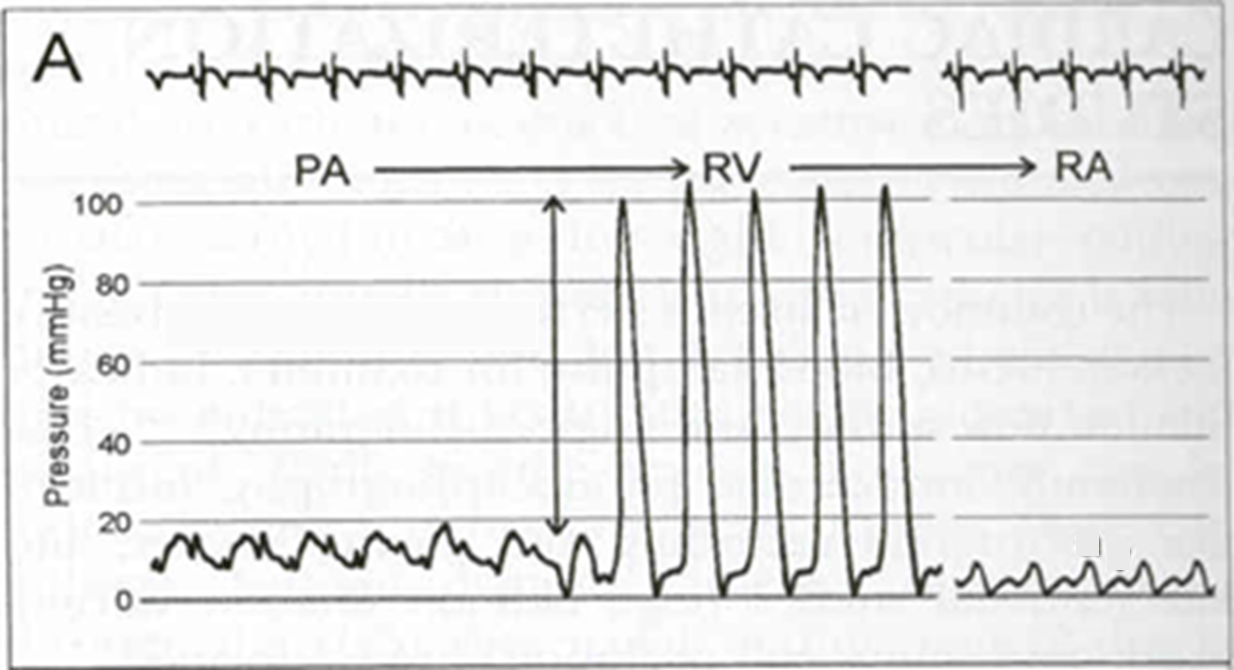
Pulmonic stenosis (valvular), PG 86 mmHg = severe.
You diagnose a left to right shunting VSD with a peak systolic velocity of 5 m/s.
- What is the pressure gradient? (200 pts)
- Are you concerned or relieved by this velocity and why? (200 pts)
- Pressure gradient ~ 100 mmHg
(PG ~ 4 x vel^2; 4 x 5^2)
- Relieved. Higher velocity indicates high pressure gradient between LV and RV (typical pressure gradient should be ~ 100 mmHg; LV syst P = 120 mmHg; RV syst P = 20 mmHg)
Explain Eisenmenger's Physiology.
Right to left shunting that occurs secondary to pulmonary vascular disease/increased pulmonary vascular resistance; leads to reversal of previous left-to-right shunt
List the 3 fetal shunts that close upon birth
Ductus arteriosus
Ductus venosus
Foramen ovale
Name the site and direction of this shunt? (Oximetry run)
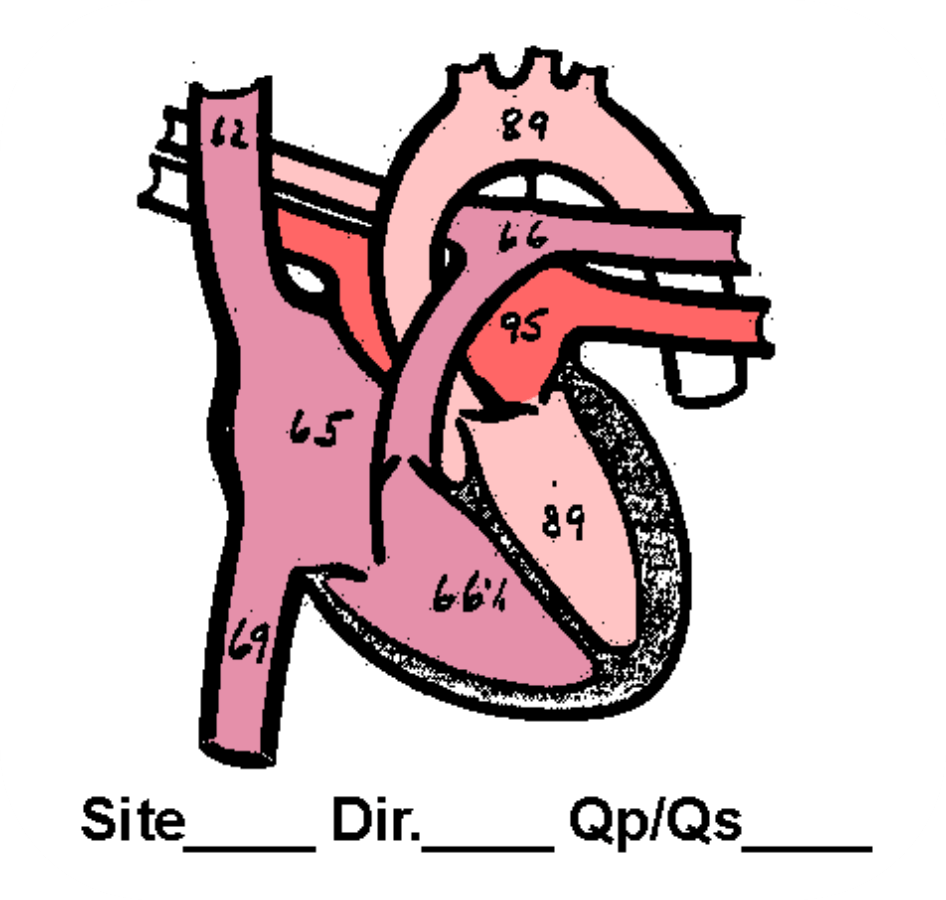
R-L VSD shunt, with O2 stepdown in LV.
This is cyanotic heart disease. Elevated Right heart pressures required to shunt from RV to LV.
Explain what is occurring in this pressure study.
Branham's Sign
You diagnose a left to right PDA on echo. The transaortic velocity is 3.5 m/s. Provide two differential diagnoses.
1. (Sub)aortic stenosis
2. Increased stroke volume secondary to L to R PDA
Explain differential cyanosis and which specific type of a congenital heart disease this is associated with in dogs.
Occurs with R to L shunting PDAs
Differential cyanosis occurs because deoxygenated blood enters the aorta after the brachiocephalic trunk and left subclavian artery (the “head” vessels – the head and front limbs receive oxygenated blood)