This is the primary mechanism responsible for airflow limitation in COPD.
Small airway inflammation and alveolar wall destruction (emphysema)
This is the most common cause of acute worsening in COPD symptoms.
Respiratory infections
Albuterol belongs to this drug class and provides quick relief of COPD symptoms.
Beta-2 agonist
This spirometry test confirms the diagnosis of COPD by showing an FEV₁/FVC ratio less than this value.
70%
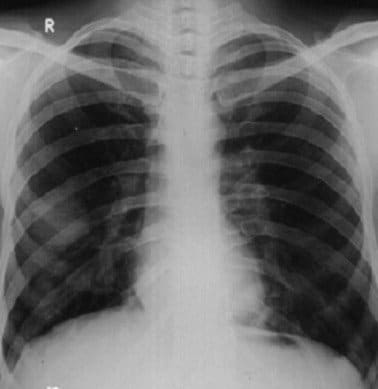
Normal or abnormal?
Normal.
This term describes the trapping of air in the lungs due to loss of elastic recoil and narrowed airways during expiration.
Air trapping or dynamic hyperinflation
Long-standing COPD can lead to this form of right-sided heart failure.
Cor pulmonale
This long-acting anticholinergic bronchodilator, taken once daily, helps maintain open airways in COPD.
Tiotropium
In COPD, lung volume testing typically reveals this increase in total lung capacity due to air trapping called:
Hyperinflation
What do you think the arrows are pointing to?
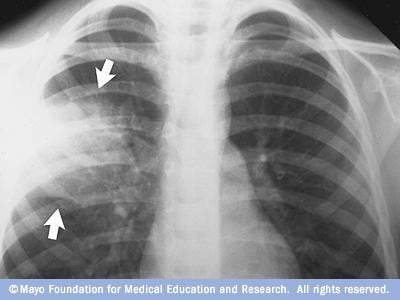
Pneumonia
This immune cell plays a central role in chronic inflammation seen in COPD.
What are neutrophils
Due to air trapping and hyperinflation, COPD patients are at increased risk of this complication if alveoli rupture.
Spontaneous pneumothorax
Salmeterol in the salmeterol-fluticasone combo belongs to this drug class.
Beta-2 agonist
This lung volume is often elevated in COPD and reflects the amount of air remaining in the lungs after maximal exhalation.
Residual volume.
Council Rocco to stop smoking.
Chronic hypoxia from COPD can lead to this vascular complication, increasing the risk of right heart failure.
Pulmonary hypertension
This chronic complication of COPD leads to low oxygen levels, increased red blood cell production, and hyperviscosity.
Secondary polycythemia
Fluticasone in the salmeterol-fluticasone combination helps reduce COPD exacerbations by acting through this mechanism.
Anti-inflammatory action via corticosteroid (glucocorticoid) effects
On arterial blood gas, this acid-base disturbance may be seen in advanced COPD due to chronic CO₂ retention.
Compensated (or chronic) respiratory acidosis
What do you think is going on?

Pneumothorax
This condition, often coexisting with chronic bronchitis in COPD, is defined by permanent enlargement of airspaces distal to the terminal bronchioles with destruction of their walls.
Emphysema
COPD increases the risk of this skeletal complication due to chronic inflammation, steroid use, and inactivity.
Osteoporosis.
This is the major adverse effect of inhaled corticosteroids like fluticasone in COPD management.
Increased risk of pneumonia
This measurement from spirometry reflects the volume of air exhaled in the first second and is used to grade the severity of COPD.
FEV₁ (Forced Expiratory Volume in 1 second)
What respiratory disease do you think this diva has?

COPD