A 58-year-old woman with amyotrophic lateral sclerosis (ALS) presents to the emergency department complaining of increased weakness and difficulty with feeding herself. Her daughter inquires if there are any interventions which have been proven to increase life expectancy in ALS patients. Which of these is the MOST appropriate answer?
A. Amantadine
B. Noninvasive ventilation
C. Colostomy
D. Prophylactic antibiotics
E. Indwelling nasogastric tube
Answer: Non-invasive ventilation (B)
Patients with ALS have progressive degeneration of both upper and lower motor neurons causing weakness, difficulty swallowing, and respiratory insufficiency. Although many different approaches have been tried to manage these patients, there are only a few which have shown benefits in increasing life expectancy. Noninvasive ventilation, specifically with optimized bilevel positive airway pressure (BiPAP) protocols, helps to avoid hypercarbia, secondary to diaphragm and respiratory muscle weakness.
Other interventions include certain medications (riluzole) that are thought to work on the neuronal level and shown to increase survival by few months and delay the onset of tracheostomy and ventilator dependence in selected ALS patients.
Amantadine is used to promote alertness in patients with neurological injury; however, it has not been shown to be of benefit in ALS.
Although patients with ALS often get gastrostomy tubes for safer feeding, colostomy and indwelling nasogastric tubes have not been shown to increase life expectancy.
Prophylactic antibiotics are not recommended for ALS as there is no immune suppression.
A 64-year-old male with a past medical history significant for hypertension, heart failure with reduced ejection fraction, myocardial infarction 2 years prior, and chronic kidney disease presents to the ICU following open AAA repair. He was restarted on his home medications on postoperative day 1. Three days later, his vitals and pertinent laboratory values include: blood pressure 150/100 mm Hg, heart rate 94 bpm, potassium 2.9 mmol/L, serum creatinine 2.6 mg/dL. The following electrocardiogram is obtained 24 hours after admission:
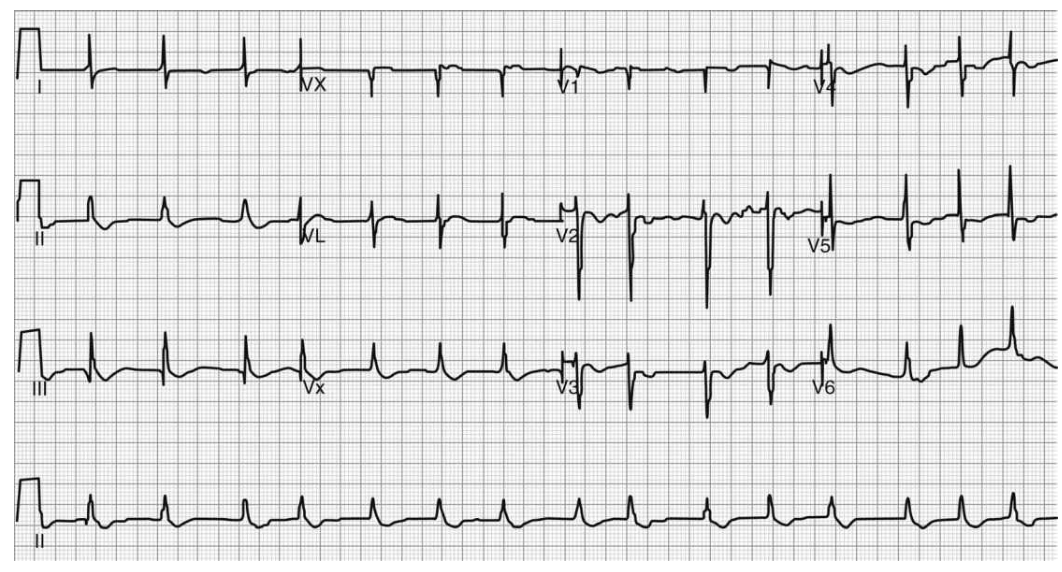
Which of the following medications was the patient most likely taking before surgery?
A. Metoprolol
B. Digoxin
C. Lisinopril
D. Furosemide
Answer: Digoxin (B)
The electrocardiogram above shows characteristic ST segment downsloping depression as well as a shortened QT interval. However, a number of atrial and ventricular arrhythmias are possible with digoxin toxicity. Increased automaticity (atrial fibrillation/ flutter) with AV block, ventricular tachycardia, fibrillation and ectopy, and bradycardia can be seen.
Symptoms of acute digoxin toxicity include nausea, vomiting, diarrhea, hyperkalemia, lethargy, and confusion. The initial GI symptoms occur early at 2 to 4 hours post ingestion, with cardiovascular complications occurring later at 8 to 12 hours.
The treatment of digoxin toxicity is with Digoxin-specific Fab antibody fragments, which bind to molecules of digoxin, making them unavailable for binding at their site of action.
Digoxin has a narrow therapeutic index and patients must be monitored closely to detect signs of toxicity in the setting of electrolyte, acid-base disturbances, and in renal impairment.
A 81-year-old female with history of atrial fibrillation on Coumadin, hypertension, and recent hip fracture from a fall s/p trochanteric fixation of the femoral head who has been recovering in a skilled nursing facility is brought into the emergency department (ED) with complaints of altered mental status, high fevers, and productive cough. The patient is emergently intubated because of lethargy and is transferred to the ICU. On arrival to the ICU, the patient’ s vitals are HR 110 bpm, BP 90/65 mm Hg, SpO2 91% on 60% FiO2 on the ventilator. ABG is showing pH of 7.38, PaO2 of 88 mm Hg, PaCO2 of 39 mm Hg, and HCO3 of 22. Despite an increase of the FiO2 on the ventilator, increase of PEEP, and repositioning of the ETT, the patient’ s oxygenation does not improve. A decision to obtain a CXR is made and the imaging obtained follows.

What is the next appropriate intervention given these clinical findings?
A. Perform needle decompression of the chest
B. Retract the endotracheal tube by 2 cm
C. Change the patient position from supine to prone
D. Perform a bronchoscopy
E. Insert chest tube on the left side of the chest
Answer: Perform Bronchoscopy (D)
Based on the chest X-ray obtained, the patient’s hypoxemia is due to left lobe collapse. Given the patient’s history of productive cough and purulent sputum, left lower lobe collapse is likely from mucous plugging, and bronchoscopy to clear the mucous plug is advised.
In case of a tension pneumothorax, contralateral shift of the mediastinum, increase in ipsilateral pleural space, and depression of the hemidiaphragm may be observed (Answer A & E Wrong).
Pleural effusion can present similarly to mucous plugging on CXR; however, the key is to look for mediastinal shift. Mucous plugging --> ipsilateral shift / Pleural effusion --> contralateral shift (Answer E Wrong).
Endotracheal tube is in appropriate position --> no evidence for mainstem intubation (Answer B Wrong)
Changing the patient’s position from supine to prone is a technique that can be adopted to improve patient’s oxygenation and V/Q mismatch. It is often employed as an adjunctive measure in patients with severe ARDS (Answer C Wrong).
Which of the following statements is MOST ACCURATE regarding the pathophysiology behind bilateral obstructive nephropathy?
A. Glomerular filtration rate (GFR) is increased by increasing renal blood flow and decrease in tubular hydrostatic pressure.
B. Sodium excretion is partially stimulated after relief of obstruction due to up regulation of atrial natriuretic peptide.
C. Arterial blood gas will demonstrate a hypokalemic, metabolic alkalosis.
D. Renal ultrasound is NOT a useful screening tool for obstructive uropathy due to low specificity.
Answer: Sodium excretion is increased post obstruction (B)
Often renal sodium excretion increases after relief of the obstruction. Two mechanisms that could potentially contribute to this include: the down-regulation of the apical membrane transporters and an up-regulation of atrial natriuretic peptide.
In patients with obstructive uropathy, a reduction in GFR (not an increase) occurs due to an increase in tubular hydrostatic pressure, which alters the balance between the glomerular capillaries and the renal tubules (Answer A Wrong).
These patients will typically present with hyperkalemia and metabolic acidosis, which is most likely a reflection of a reduced GFR and renal function (Answer C Wrong).
Ultrasound is utilized as a good screening tool for patients with new-onset or unexplained AKI to rule out urinary tract obstruction as a potential etiology (Answer D Wrong).
A 71-year-old man with diabetes, obesity, hypertension, and benign prostatic hypertrophy is admitted to the intensive care unit with abrupt-onset groin pain, fever, and a rapidly spreading erythematous groin and lower abdominal rash with ill-defined margins. The rash is exquisitely tender and firm to palpation. He develops hypotension with mean arterial pressure measured at 52 mm Hg, refractory to intravenous fluid resuscitation.
What is the MOST appropriate sequence of events to manage his disease?
A. Insert a central venous catheter, start vasopressors, obtain two sets of blood cultures, and start antibiotic therapy with vancomycin, meropenem, and clindamycin
B. Start antibiotic therapy with vancomycin, meropenem, and clindamycin; obtain two sets of blood cultures, surgical consult for emergent debridement, and start vasopressors
C. Start vasopressors, obtain two sets of blood cultures, start antibiotic therapy with vancomycin, piperacillin-tazobactam, and clindamycin; surgical consult for emergent debridement
D. Start vasopressors, obtain two sets of blood cultures, start antibiotic therapy with vancomycin, piperacillin-tazobactam, and clindamycin; obtain CT or magnetic resonance image (MRI) of pelvis, surgical consult for emergent debridement
Answer: Start vasopressors, obtain two sets of blood cultures, start antibiotic therapy with vancomycin, piperacillin-tazobactam, and clindamycin; surgical consult for emergent debridement (C)
This scenario describes the clinical presentation of necrotizing fasciitis, specifically Fournier gangrene, a necrotizing soft tissue infection of the perineum. The microbiology of this disease comprises facultative organisms (Escherichia coli, Enterococcus spp.) and anaerobes (Bacteroides, Clostridium, Fusobacterium). Thus, antimicrobial therapy should target this spectrum of bacterial pathogens and should also include clindamycin, for its antitoxin properties against toxin-producing streptococci and staphylococci. Meropenem or piperacillin-tazobactam is an appropriate component of first-line regimens, which should also include clindamycin. Patients with risk factors for MRSA should also be given vancomycin or daptomycin.
Hemodynamic instability is common with necrotizing soft tissue infections and requires aggressive supportive care with intravenous fluids and vasopressors. Vasopressor therapy should not be delayed until a central line can be placed, and hypotensive shock should be addressed before or simultaneously as blood cultures are drawn and antibiotics are started, and not delayed.
Surgical consult should not be delayed by obtaining CT, MRI, or other imaging looking for soft tissue gas collections to support a diagnosis of necrotizing soft tissue infection. Surgical exploration is the only way to definitively establish the diagnosis and obtain source control. Early surgical debridement has also been shown to improve outcomes.
A 74-year-old man with depression, hypertension, coronary artery disease, epilepsy and Parkinson disease is admitted to the ICU for management of pneumonia. He is intubated, sedated on fentanyl infusion and started on broad-spectrum antibiotics. Six days after admission, he is found to have worsening fever, rigidity, and is no longer following commands. What is the MOST likely etiology for his condition?
A. Status epilepticus
B. Meningitis
C. Serotonin syndrome
D. Neuroleptic malignant syndrome (NMS)
E. Infective endocarditis
Answer: Neuroleptic Malignant Syndrome (D)
NMS is an uncommon but often life-threatening illness characterized by fever, rigidity, obtundation, and autonomic instability . Elevated serum creatine kinase levels can also be seen. Though the pathogenesis is not well understood, it is thought to be related to a sudden decrease in dopaminergic signaling, which may be caused by stopping dopaminergic drugs such as levodopa as well as the use of neuroleptics.
It is commonly confused with serotonin syndrome; however, serotonin syndrome is a much more rapidly developing condition caused by excess serotonin signaling (within 24 hours).
This patient is unlikely to have status epilepticus or stroke, as that is unlikely to cause worsening fevers with rigidity.
Infective endocarditis would present with fevers and potentially with neurological deficits if it leads to septic emboli to the brain; however, rigidity, obtundation, and autonomic instability are not typical for infective endocarditis.
A 46-year-old male with Epstein anomaly, hypertension, coronary artery disease, and chronic obstructive pulmonary disease underwent an uncomplicated laminectomy but reports severe pain in the post anesthesia recovery unit. His pain eventually improved after repeated intravenous opioid boluses. However, an ECG reveals new-onset AF with a widened QRS complex and a heart rate between 130 and 140 beats/min. The patient’ s blood pressure is stable at 110/50 mm Hg, respiratory rate 17/min,
O2 saturation is 98% while receiving 3 L oxygen/min via nasal cannula. The patient is otherwise asymptomatic. The heart rate and rhythm have not changed for the last hour. The patient was in sinus rhythm leading up to this event.
Which next intervention is MOST appropriate?
A. Synchronized cardioversion
B. Amiodarone 150 mg IV bolus
C. Metoprolol 5 mg IV bolus
D. Procainamide 10 mg/kg IV bolus over 5 minute
E. Digoxin 0.25 mg IV bolus
Answer: Procainamide 10 mg/kg IV bolus (D)
This patient has Wolff-Parkinson-White (WPW) syndrome, possibly as a result of his Epstein anomaly. Epstein anomaly is a congenital heart defect with apical displacement of the tricuspid valve and represents a known cause of WPW.
Use of nodal blocking agents in patients with WPW is potentially harmful because these drugs accelerate the ventricular rate via the excitatory pathway and even may cause ventricular fibrillation. Procainamide is the recommended agent to achieve sinus rhythm or ventricular rate control in hemodynamically stable patients with pre-excited AF and rapid ventricular response.
Synchronized cardioversion is recommended for patients with AF, WPW, and rapid ventricular response who are hemodynamically unstable.
A 45-year-old previously healthy woman presents to the emergency department with 3 days of fevers and progressive dyspnea and is admitted to the intensive care unit (ICU) for influenza infection complicated by severe hypoxemia. She is intubated, and chest radiograph following intubation demonstrates an appropriately placed endotracheal tube with bilateral patchy opacities and interstitial markings throughout all lung fields, without effusions.Her bedside echocardiogram reveals a left ventricular ejection fraction of 0.75 with otherwise normal findings. Her ventilator settings are volume control, tidal volume (VT) 500 mL, respiratory rate (RR) 14 breaths per minute, FiO2 1.0, and positive end-expiratory pressure (PEEP) 5 cm H2O. An initial arterial blood gas (ABG) is pH 7.30 PCO2 45 mm Hg and PO2 80 mm Hg. Which of the following therapies has been best shown to improve the survival of patients such as this woman?
A. Diuresis to maintain a negative fluid balance
B. Ventilation at a TV of 6 mL/kg of ideal body weight (IBW)
C. Initiation of inhaled pulmonary vasodilator for severe hypoxemia
D. Bronchoscopy to rule out additional infections
E. Titration of PEEP with recruitment maneuver to optimize lung compliance
Answer: Ventilation at a TV of 6 mL/kg of ideal body weight (IBW) (B)
This patient is presenting with severe ARDS, as defined by the Berlin criteria: onset within 1 week or presentation, bilateral opacities on imaging, edema not fully explained by cardiogenic etiology, and PaO2:FiO2 ratio of <100. The ARDSnet trial demonstrated a significant mortality benefit with lung protective, low-TV ventilation (6 mL/kg IBW) (answer B is correct).
Diuresis to an even fluid balance increases ventilator-free days inpatients with ARDS but has not been found to have a mortality benefit (answer A is incorrect).
Similarly, while inhaled vasodilator (EPO) and PEEP titration may improve oxygenation, neither intervention has been demonstrated to improve survival (answers C and E are incorrect).
Invasive respiratory cultures are not recommended in patients with severe community acquired pneumonia (answer D is incorrect).
A healthy 24-year-old male is admitted to the intensive care unit (ICU) for AKI and hyperkalemia. History is remarkable for a recent episode of sinusitis for which amoxicillin-clavulanate therapy was initiated. Physical examination is notable for a temperature of 37.6°C, skin rashes, and joint pain. Urine microscopy shows a few RBC’ s and eosinophils. Laboratory results are given below:
WBC 12.5 k/µL, Hb 14.3 g/dL, Hct 38%, Plt 256 k/µL, and eosinophilia. Na 137 mmol/L, K 5.7 mmol/L, Cl 106 mmol/L, CO 22 mmol/L, BUN 18 mg/dL, Cr 2.3 mg/dL, and glucose 176 mg/dL.
What is the MOST appropriate next step in the management of this patient?
A. Initiate fluid resuscitation
B. Discontinue antibiotics
C. Initiate hemodialysis
D. Send patient for kidney biopsy
Answer: Discontinue Antibiotics (B)
Acute interstitial nephritis (AIN) is an important cause of AKI characterized by inflammation of the renal interstitium and tubules. AIN results from a hypersensitivity reaction, most commonly induced by medications, infections, and autoimmune disorders.
Common offending agents are antibiotics (penicillins, cephalosporins, sulfonamides, ciprofloxacin, and rifampin), anticonvulsants (phenytoin, carbamazepine, phenobarbital, valproate), diuretics (thiazides, loop diuretics, triamterene), NSAIDs, and proton pump inhibitors. Medications account for over two-thirds of all the AIN cases.
Patients with AIN could present with sterile pyuria, hematuria, eosinophilia, and fever. The majority of the patients have complete recovery of renal function. It is important to differentiate AIN from acute tubular necrosis (ATN). The diagnosis of AIN is difficult as symptoms could mimic infection. Sterile pyuria and eosinophiluria could suggest the diagnosis. Removal of the offending agent is the most important component of AIN treatment (Correct Answer B).
Treatment is largely supportive with use of renal replacement therapy as needed. Corticosteroid therapy in these patients is controversial. Discontinuation of the inciting agent is the cornerstone of treatment of acute interstitial nephritis.
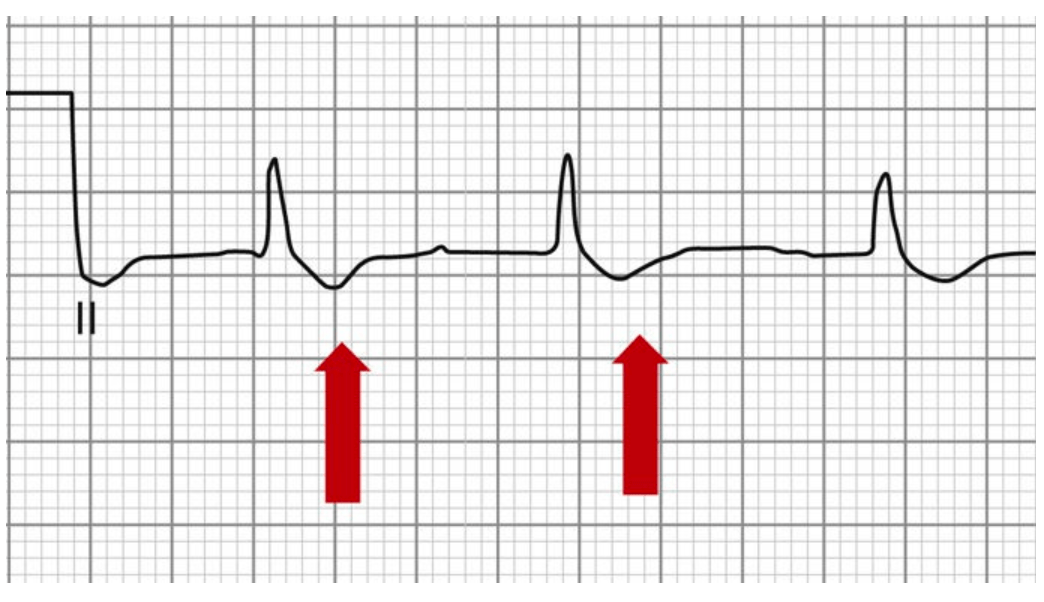
You admit a 28-year-old man to the intensive care unit in July for a generalized tonic-clinic seizure in the setting of 2 days of fevers, headache, and myalgias. The patient’ s girlfriend tells you that they were backpacking in Tennessee’ s Great Smoky Mountains National Park the week before the patient became ill, and 3 weeks before he became ill they went for a hike in the woods on Massachusetts’ CapeCod. Chest X-ray is clear, and his white blood cell count is normal. Platelet count on presentation is 139,000/µL, and hemoglobin and hematocrit are normal. Two days after admission, he develops worsening thrombocytopenia and a rash.
What is the MOST likely diagnosis?
A. Babesiosis
B. Rocky Mountain Spotted Fever (RMSF)
C. Mumps
D. Lyme disease
Answer: RMSF (B)
RMSF (Answer B) is the most common tick-borne illness in the United States, with a broad distribution across most of the lower 48 states. Symptoms on presentation are often non-specific. Classic associations include thrombocytopenia and rash (which often eventually involves palms and soles); however, it is rarely present when the patient becomes ill and commonly develops 3 to 5 days into the course of illness. RMSF has an incubation period of 2 to 14 days after being bitten by an infected tick, and many patients do not recall any tick bite.
Although Lyme disease (Answer D) can cause thrombocytopenia, confusion and seizures are not common with central nervous system Lyme disease; nor is late presentation of rash.
Babesiosis (Answer A) is also a tick-borne disease that can be contracted, but usually presents with anemia and does not cause seizures.
Co-infections should always be considered when evaluating a patient with suspected tick-borne illness, as it is not uncommon for a single tick bite to transmit multiple infectious pathogens.
A 49-year-old man with no past medical history is admitted to the medicine service for 2 weeks of intermittent night sweats, myalgia, and progressive headache. Other than febrile, his vital signs are normal at the time of admission. His neurologic examination at the time of admission is normal, and basic laboratory workup is unrevealing. A lumbar puncture is performed with a normal opening pressure, pleocytosis with 41 white blood cells/microL (94% polymorphonuclear cells), 5 red blood cells/microL, glucose 58 mg/dL, and protein 53 mg/dL. There w as concern for potential infectious meningitis, so vancomycin, ceftriaxone, and acyclovir were started. One day following the lumbar puncture, the patient had acute onset of marked expressive aphasia and right facial weakness. A head computed tomography (CT) was completed and demonstrated in the figure that follows.
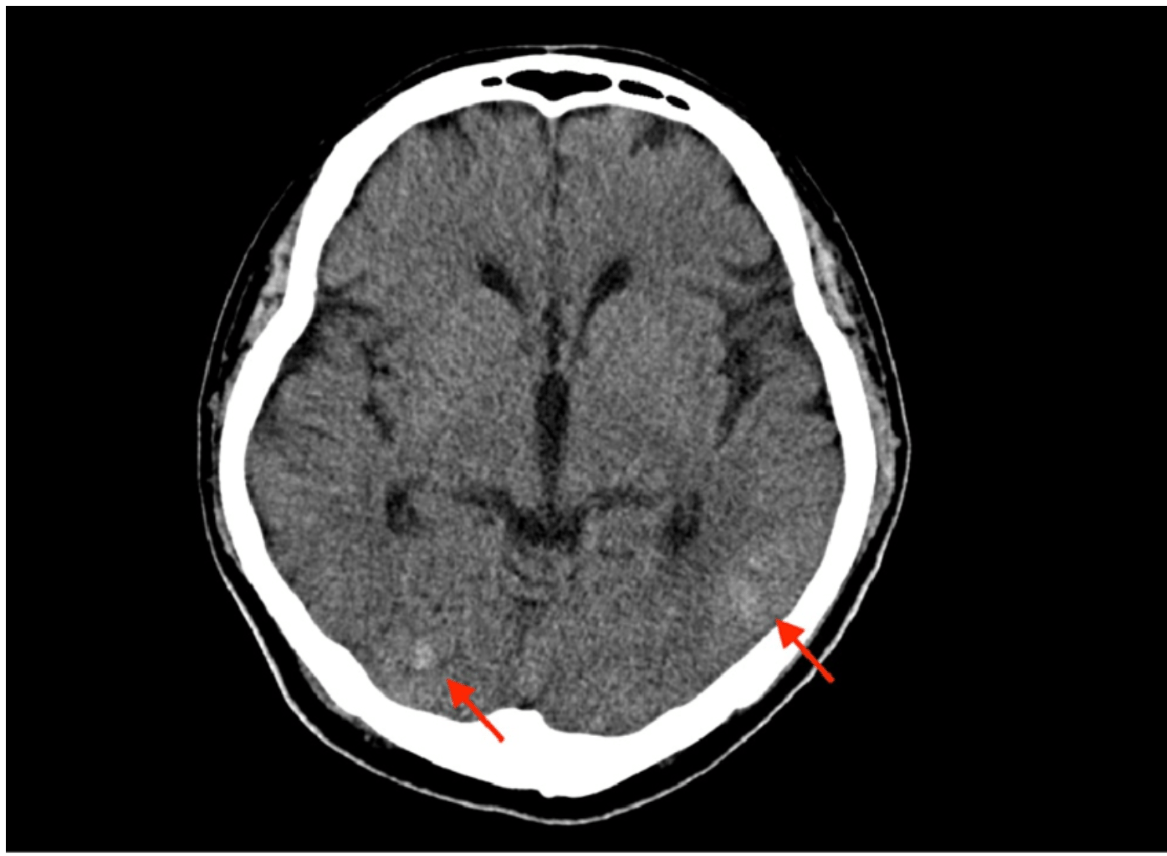
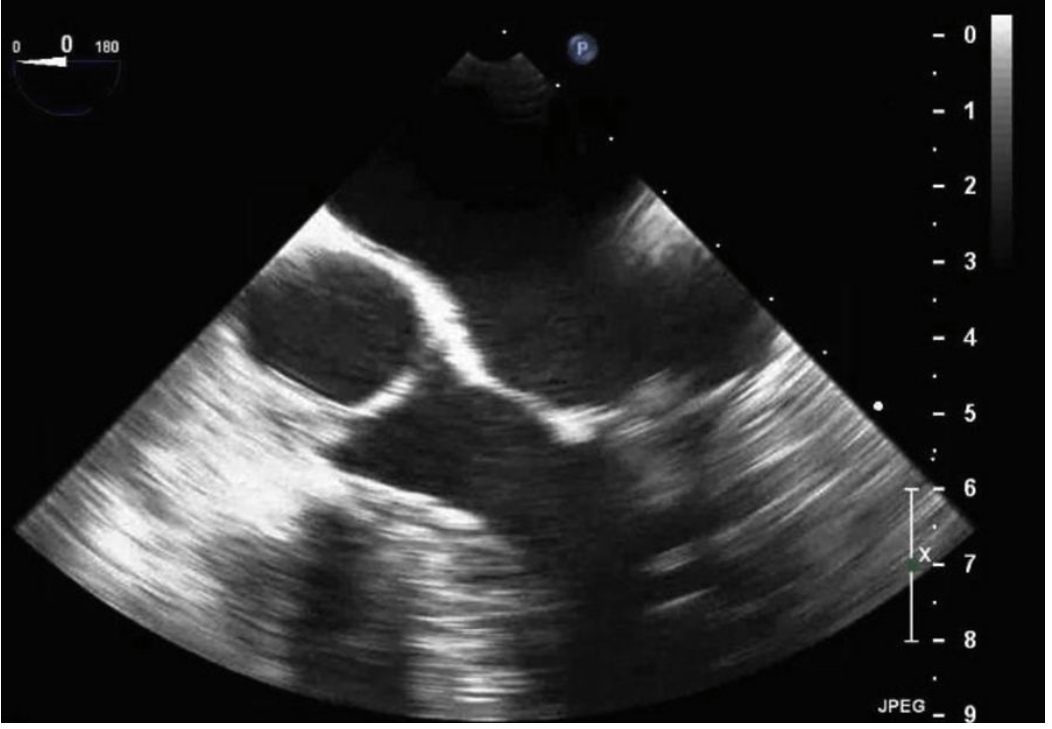
What is the next best step in management of the patient’ s possible endocarditis?
A. The patient should undergo urgent (within 5 days) mitral valve replacement.
B. The patient should undergo urgent (within 5 days) mitral valve repair.
C. The patient should undergo delayed (∼4 weeks) mitral valve replacement.
D. The patient should undergo delayed (∼4 weeks) mitral vale repair.
E. Only antibiotics therapy is needed, and current antibiotics should remain the same.
Answer: Delayed mitral valve repair (D)
The patient meets Duke criteria for possible endocarditis, given he has one major criteria (transthoracic echocardiography [TTE] with new regurgitation and mobile target) and two minor criteria (fever and emboli).
The patient has a severe mitral regurgitation, which will require surgical repair. There are mixed criteria for early intervention, but the American Heart Association recommends early intervention if any of the following is observed:
1) Valve dysfunction causing symptoms or signs of heart failure
2) Para-valvular extension of infection with development of annular or aortic abscess
3) Destructive or penetrating lesion causing heart block
4) Infection from a difficult-to-treat pathogen such as fungal or highly resistant organism
5) Persistent infection after the start of appropriate antibiotics
This patient does not meet the criteria above, and there is no need to repair his mitral valve urgently.
In patients with mitral valve IE, repair is generally preferred over replacement (especially in younger patients), as it has been shown to have distinct advantages (increased survival rates, lower recurrence of infection, fewer complications).
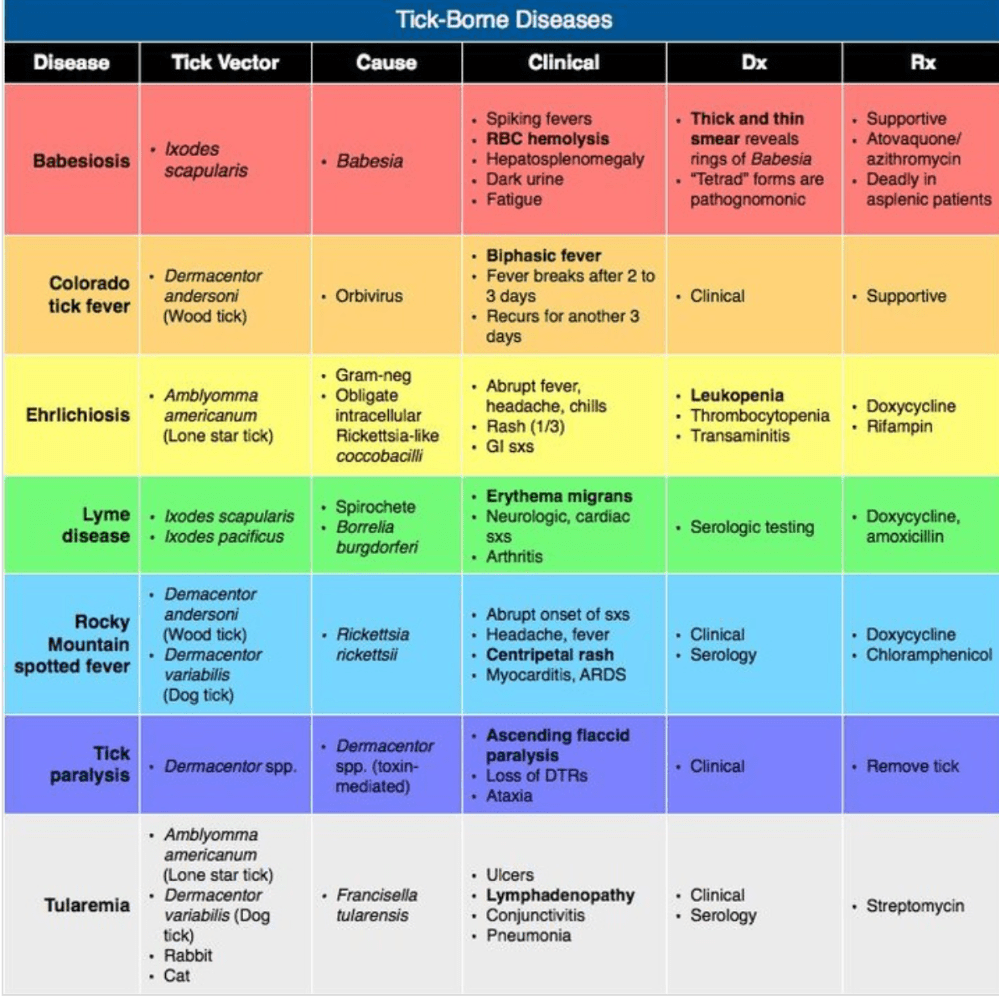
An 88-year-old male with complex coronary disease that includes prior three-vessel coronary artery bypass grafting and prior complete heart block necessitating dual chamber permanent pacemaker implantation presents with substernal chest pain identical in character to his past angina.
His presenting electrocardiogram is:
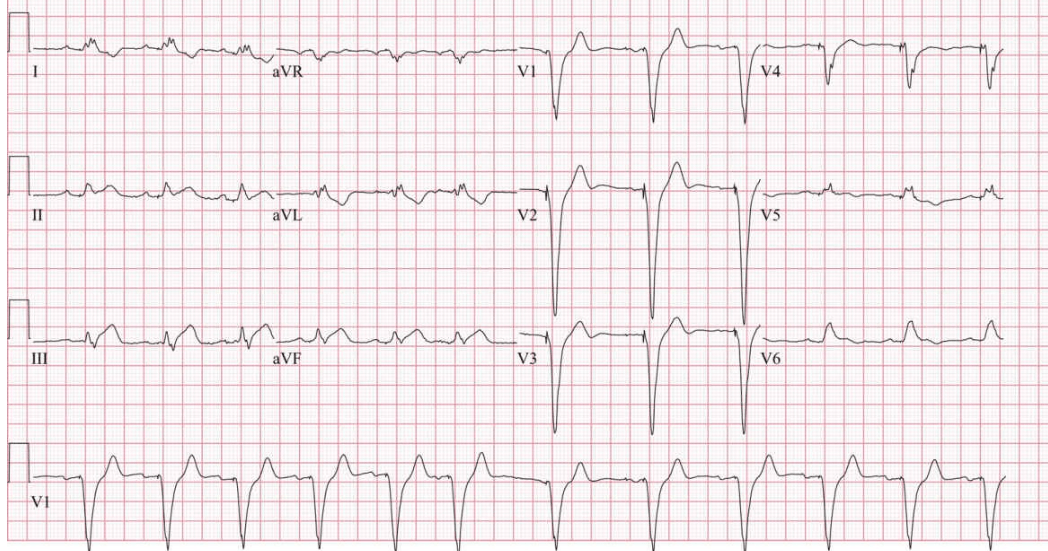
His presenting troponin-T is 0.54 ng/mL (reference <0.03 ng/mL).
Which of the following is the next best step in management?
A. Emergent coronary angiography with the intent to revascularize
B. Urgent (24-48 hours) coronary angiography with the intent to revascularize
C. Noninvasive risk stratification
D. Intravenous nitroglycerin
Answer: Emergent coronary angiography (A)
The diagnosis of myocardial ischemia and infarction in the presence of conduction disturbances proves more challenging. Ischemic symptoms with a presumed new left bundle branch block (LBBB) or right bundle branch block (RBBB) that is not rate related is associated with adverse prognosis.
In patients with an LBBB, ST segment elevation ≥1 mm concordant with the QRS complex in any lead may be an indicator of acute myocardial ischemia. Similar criteria can be used to diagnose acute myocardial infarction in the presence of right ventricular pacing as demonstrated in this patient’ s electrocardiogram. Because of the concordant QRS-ST changes apparent in the inferior leads of this patient’s electrocardiogram, emergent angiography should be pursued.
A 54-year-old man with ischemic cardiomyopathy is admitted to ICU for respiratory failure due to decompensated heart failure and cardiogenic pulmonary edema. On the day of admission, he requires intubation and mechanical ventilation, and aggressive diuresis is initiated. On day 3 of his ICU stay , his ventilator is set on pressure support, with a driving pressure of 5 cm H2O, PEEP of 10 cm H2O, and FiO2 of 0.3. He is fully aw ake and breathing comfortably. He is placed on a spontaneous breathing trial with pressure support settings of driving pressure of 5 cm H2O, PEEP of 0 cm H2O, andFiO2 of 0.3. Within minutes, he experiences oxygen desaturation, tachypnea, and respiratory distress.
Which among the following is the MOST LIKELY cause for failure of his spontaneous breathing trial?
A. Atelectrauma from collapse of alveoli with tidal breathing
B. Mucous plugging from lower airway pressure
C. Increased preload and decreased afterload
D. Decreased preload and increased afterload
E. Increased preload and increased afterload
Answer: Increased preload and increased afterload (E)
The application of PEEP in both noninvasive and invasive positive pressure ventilation serves to decrease cardiac preload, through decreased venous return and decrease (left-sided) cardiac afterload as a result of decreased ventricular volume (and therefore radius) and transmural cardiac wall tension.
In patients with baseline cardiac dysfunction, weaning-induced cardiac dysfunction may be observed when the absence of PEEP leads to an acute increase in cardiac preload and afterload (answer E is correct; answers C and D are incorrect).
A 62-year-old woman with medical history of hypertension and smoking presents to the hospital after sudden onset of severe headache followed by collapse. In the emergency department, CT scan of the head showed diffuse subarachnoid hemorrhage and CT angiogram revealed a left middle cerebral artery aneurysm. An extra-ventricular drain is placed by neurosurgery team. On day 7 of hospitalization, the patient develops new aphasia. The urine output has been 1800 mL in the past 3 hours, while the serum sodium has decreased from 138 to 132 mmol/L.
What is the best next step in management to address this high urine output?
A. Start fluid restriction and continue to monitor the sodium every 6 hours
B. Aggressively replace volume deficit by giving bolus of 2 L of 0.9% normal saline and recheck sodium after the bolus
C. Start fludrocortisone and salt tablets
D. Stop maintenance intravenous fluids and give 250 mL of 3% hypertonic saline, recheck sodium level after administration
E. Continue administration of intravenous normal saline for maintenance and to replete urine output. Give a 250 mL bolus of 3% hypertonic saline
Answer: Fluid and Sodium Repletion (E)
In the setting of acute intracranial injury, both syndrome of inappropriate secretion of antidiuretic hormone (SIADH) and cerebral salt wasting (CSW) are potential causes of hyponatremia. The main difference between the two is the patient’s volume status which can be difficult to determine using clinical criteria.
In SIADH, the patient is typically in an euvolemic or hypervolemic state, while in CSW, the patient is hypovolemic. Consistent with the above description, CSW is associated with large urine output volumes, whereas SIADH is associated with low to normal amounts of urine output volumes.
Evaluation for CSW begins with a basic metabolic panel to identify the hyponatremia (serum sodium less than 135 mEq/L). Urine studies are commonly checked for urine sodium and osmolality. Urine sodium is typically elevated above 40 mEq/L. Urine osmolality is elevated above 100 mosmol/kg.
High urine output with reduction in serum sodium, in a patient with subarachnoid hemorrhage, likely suggests CSW syndrome. The treatment for CSW involves repletion of fluid and salt to prevent volume contraction (Answer E).
A 78-year-old woman with diabetes and hypertension presents to the emergency department with confusion and hypotension. A urinalysis is notable for a white blood cell count of >100,000 and is positive for leukocyte esterase. Urine culture subsequently grows>100,000 Pseudomonas aeruginosa, resistant to ciprofloxacin. You begin appropriate antibiotic therapy with a beta-lactam antibiotic.
For how long should she be treated?
A. 5 to 7 days
B. 7 to 10 days
C. 10 to 14 days
D. Until her confusion resolves
Answer: 10 to 14 days (C)
This patient has an acute complicated urinary tract infection. Patients presenting with complicated urinary tract infections should have urine culture performed to confirm the microbiologic cause of the infection and antimicrobial susceptibility of the pathogen(s) causing the infection. Total antibiotic duration depends on the antibiotic class used to treat the infection. Fluoroquinolones are given for 5 to 7 days, trimethoprim/sulfamethoxazole for 7 to 10 days, and beta lactams for 10 to 14 days. Longer durations may be appropriate for patients with an ongoing nidus of infection (eg nonobstructing stone).
A 56-year-old female is admitted to the intensive care unit for management of a complete right middle cerebral artery ischemic stroke. During her stay within the intensive care unit, she has progressive somnolence over the course of 96 hours with only minor changes on her CT scan and no midline shift. Given her profound stupor, an EEG w as ordered and a portion of the recording is shown in the figure that follows. Her current neurologic examination showed symmetric and reactive pupils at 3 mm, right gaze preference but crosses midline, profound upper motor neuron facial droop on the left, left arm and leg weakness. Patient did not follow commands or open eyes, but she continues to localize with the right arm.
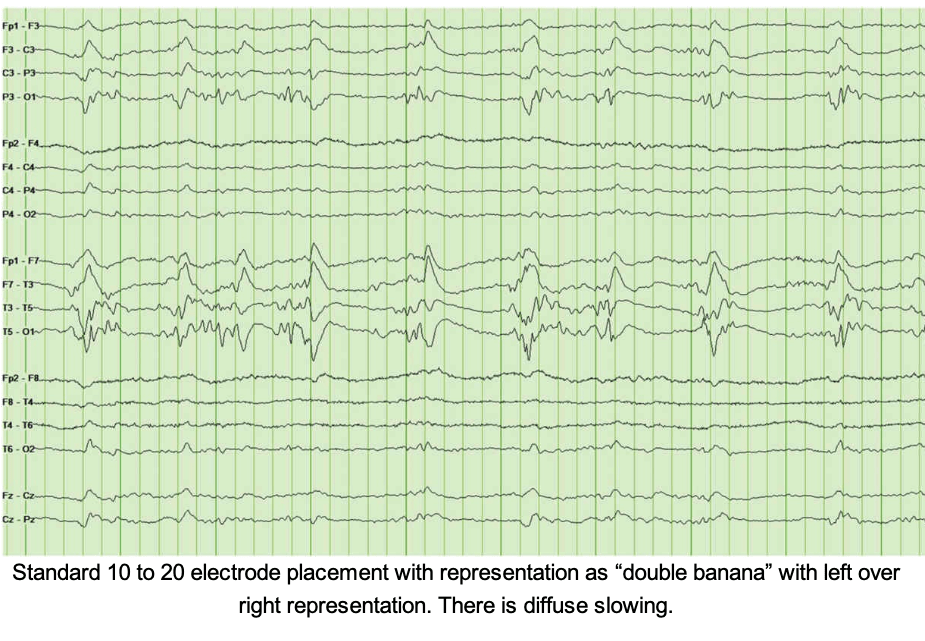
What is the next best step in management for this patient?
A. Continue with supportive care and no change to medications
B. Initiation of antiepileptic medication—levetiracetam 500 mg twice a
day
C. Benzodiazepine trial—lorazepam 1 mg IV once
D. Neurosurgery consultation for craniectomy
Answer: Continue with supportive care (A)
Patient’s neurological examination is consistent with her right middle cerebral artery stroke. There is no clear clinical signs of seizures noted. The EEG was done to further investigate her mental status, which demonstrates spikes or sharp waves occurring at regular intervals, which is called periodic lateralized epileptiform discharges (PLEDs). There are no electrographic signs of seizures present on this EEG.
PLEDs are commonly seen in patients with multiple CNS diseases such as acute ischemic stroke, tumor, infection, hemorrhage, and metabolic disorders. In this case presentation acute stroke is the likely etiology. Given stable CT head with no signs of midline shift, there is no indication of decompressive craniectomy at this point. There are no signs of clinical or electrographic seizures, so option B and C are not indicated at this point. Continue supportive care is the right choice for now.
A 40-year-old woman with idiopathic pulmonary arterial hypertension on continuous treprostinil has worsening shortness of breath and weight gain of 8 kg in the setting of non-adherence to her home diuretic regimen. On evaluation in the emergency department, she is found to have T 37°C, BP 90/62 mm Hg, HR126 beats per minute, respiratory rate 40 breaths per minute, andSpO2 74% that improves to 84% on high-flow nasal cannula at60 L/min and FiO2 0.6. While undergoing other workup, the patient’s respiratory status worsens and the decision is made to intubate her.
Which of the following is most accurate regarding her physiology?
A. She should receive an IV fluid bolus before induction to maintain preload.
B. Vasopressin may help preserve right ventricular systolic function during intubation.
C. She should receive high minute ventilation with a high positive end-expiratory pressure to maintain her oxygenation during intubation.
D. There is evidence that norepinephrine is the best medication for hemodynamic support in this situation.
E. Propofol is the preferred agent for induction in this patient.
Answer: Vasopressin may help preserve right ventricular systolic function during intubation (B)
Patients with right heart failure and cardiogenic shock have very tenuous hemodynamics, and intubation presents a uniquely dangerous challenge in this patient population. The combination of induction medications and mechanical ventilation with increased intrathoracic pressures acutely decreases preload to the right ventricle and can increase afterload via an increase in pulmonary vascular resistance with overdistention of the lungs. In addition to avoiding intubation whenever possible, strategies can be undertaken to minimize risk if intubation is unavoidable.
Vasopressor support is recommended, and vasopressin can preserve right ventricular systolic function by preserving cardiac preload in the setting of vasodilatory induction drugs and by preserving perfusion to the right ventricle and preventing worsening ischemia (answer B is correct).
Norepinephrine provides additional inotropic support and is commonly used but there is no high-quality evidence that shows that norepinephrine is superior to other agents (answer D is incorrect).
Although hypercarbia is poorly tolerated, aggressive ventilation with high tidal volumes, high respiratory rate, and high positive end-expiratory pressures can worsen right ventricular afterload by increasing pulmonary vascular resistance (answer C is incorrect).
Propofol is vasodilatory, therefore decreasing preload, and has a potential negative inotropic effect (answer E is incorrect).
Although an acute decrease in preload is a concern, this patient is already volume overloaded and additional IV fluids are not recommended (answer A is incorrect).
A 70-year-old male with a history of COPD, requiring prior intubation, and active tobacco use presents to the emergency department with shortness of breath. He states that over the last 24 hours, he has had increasing difficulty breathing. He denies fevers or chills at home and is not aw are of any sick contacts. His initial vitals are temperature of 99.4 F, heart rate 90/min, blood pressure 130/80 mm Hg, respiratory rate 22/min, and SpO2 95%. On examination, he appears to have a mild increase in work of breathing. He is noted to have scattered wheezing throughout both lung fields. He is started on albuterol nebulizers and IV steroids.
Three hours into his emergency room stay you are called to the bedside as the patient appears to be in more distress. His vitals demonstrate temperature of 99.8, HR 125, BP 120/70 with an RR of 35 and SpO2 90%. On examination, the patient is using accessory muscles, and his lung examination is notable for poor air movement with no wheezing. An arterial blood gas is performed pH 7.28, PCO2 50, and PaO2 65. A chest x-ray is performed and demonstrates hyperinflation of both lung fields with no infiltrate.
He is intubated for hypoxemic respiratory failure and is subsequently paralyzed with a neuromuscular blocker secondary to ventilator dyssynchrony. He arrives to the ICU ventilated, with an FiO2 of 0.8, PEEP 10, RR 30, and TV 420 mL/kg (the patient weighs70 kg). His arterial blood gas demonstrates a pH 7.29/PCO2 50/PaO2 200. His blood pressure upon arrival to the ICU is 80/50 mm Hg.
His flow/time wave form is noted in the following figure:
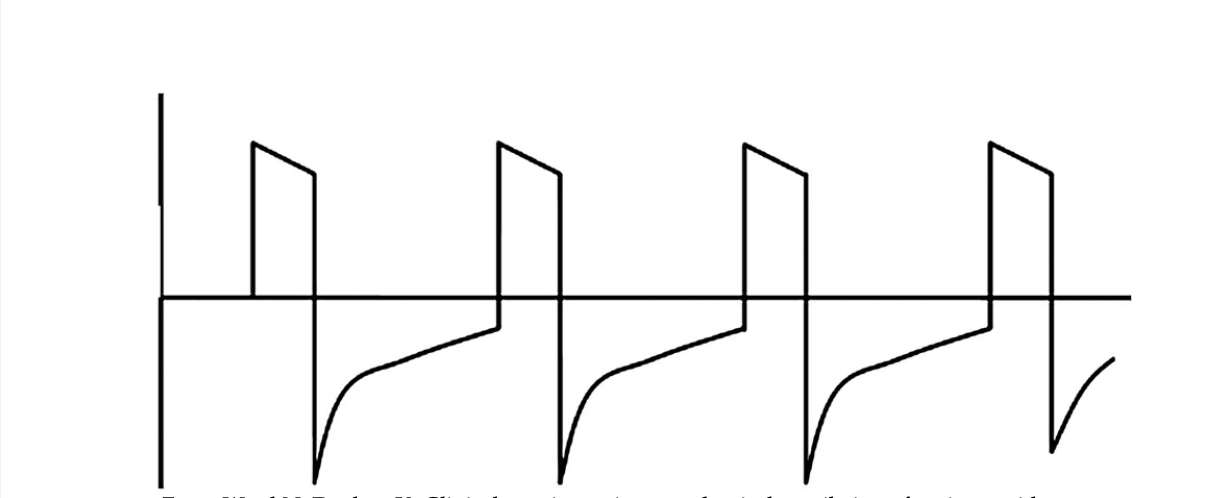
What would be the next step in management?
A. Increase his tidal volumes
B. Increase his PEEP from 10 to 15
C. Decrease the respiratory rate
D. Increase the inspiratory time
Answer: Increase Respiratory Rate (C)
The figure above demonstrates air trapping or “auto-PEEP” as the exhalation wave form fails to reach zero before the next breath is taken. Auto-PEEP can cause decreased venous return which leads to a decrease in cardiac output and results in hypotension which was seen in this patient.
To address air trapping, the key is to increase the expiratory time. Decreasing the respiratory rate is an effective way to achieve a longer exhalation period. Another way to enhance the expiratory time is to change the inspiration:expiratory ratio or the I:E time. This can be accomplished by increasing the inspiratory flow rate thus decreasing the inspiratory time.
A 78-year-old man is brought to the hospital after being found down by his daughter at his home this morning. He w as functional at baseline and last seen normal yesterday . He is a life-time smoker with chronic obstructive pulmonary disease (COPD) and w as recently diagnosed with lung cancer. On physical examination, he is lethargic, has unsteady gait, and is confused. His temperature is37.4°C, blood pressure is 127/94 mm Hg, pulse rate is 74 beats/min, and respiratory rate is 11 breaths/min. On examination, he has a normal jugular venous pressure, but he has decreased air entry at the lung bases. A CT head obtained shows age-related atrophic changes. Laboratory studies obtained are as follows:
Sodium 120 mEq/L (mmol/L)
BUN 9 mg/dL
Bicarbonate 30 mmol/L
Creatinine 1.0 mg/dL
Urine osmolality 275 mOsm/kg H2O
Urine sodium 45 mEq/L (mmol/L)
Serum osmolality 264 mOsm/kg H2O
Glucose 84 mg/dL (4.6 mmol/L)
Which of the following is the MOST appropriate next step in management of this patient?
A. Fluid restriction to 800 mL
B. Desmopressin
C. Isotonic saline infusion
D. Tolvaptan
E. Hypertonic saline infusion
Answer: Hypertonic Saline Infusion (E)
The patient’ s history and laboratory studies are consistent with hypotonic euvolemic hyponatremia. The important differentials are SIADH, adrenocortical insufficiency, polydipsia, physiological stimulus antidiuretic hormone (ADH) release (nausea, pain, anxiety), and hypothyroidism. Based on presentation, the most likely etiology of hyponatremia in this patient is SIADH.
Patients with lung cancer, particularly small cell lung cancer, have a reported incidence of up 18.9%. SIADH is caused by the secretion of ADH from the posterior pituitary gland or unregulated ectopic production by tumor cells. Elevated levels of ADH lead to hyponatremia and hypoosmolality by decreasing the renal excretion of free water.
While not all cases of hyponatremia require correction with hypertonic saline, this patient has acute onset, severe hyponatremia with moderate symptoms. Symptoms of hyponatremia include: headache, nausea, vomiting, confusion, disorientation, and seizures. Though his sodium needs correction with hypertonic saline, the sodium should not be corrected by more than 6-8 mEq/L in 24 hours to avoid osmotic demyelination syndrome (ODS). It is important to note that neurological effects related to ODS can take up to 1 week to manifest, including dysarthria and dysphagia.
A 32-year-old previously healthy man presents with fevers and hypotension. He w as bitten by a dog 4 days ago with deep puncture wounds that required operative closure. He has a history of anaphylaxis to penicillin and cephalosporins and has been receiving trimethoprim-sulfamethoxazole since surgery. Tetanus toxoid was administered and his other immunizations are up to date. On examination, his wound shows evidence of cellulitis.
Which of the following changes to his antibiotic regimen is most appropriate?
A. Change trimethoprim-sulfamethoxazole to levofloxacin
B. Add vancomycin
C. Add clindamycin
D. Continue current therapy
Answer: Add Clindamycin (C)
Amoxicillin-clavulanate for 3 to 5 days is the preferred prophylactic agent for animal bites. Alternatives in patients with cephalosporin allergies should have activity against both Pasteurella multocida (ie,trimethoprim-sulfamethoxazole, doxycycline, levofloxacin) and anaerobes (clindamycin, metronidazole). Thus, this patient has untreated anaerobic infection and would benefit from the addition of clindamycin. Changing to levofloxacin or adding vancomycin would not give the appropriate coverage.
Tetanus toxoid should also be administered to all patients who have completed primary immunization but who’s booster has been 5 years of greater.
A 73-year-old female with hypertension, hyperlipedemia, and atrial fibrillation on oral anticoagulation with coumadin sustained a mechanical fall backwards and hit the right posterior aspect of her head. Following the fall, there w as no loss of consciousness. On initial arrival to the emergency department (ED), she was interactive, but over the course of 30 minutes, she had neurologic deterioration with loss of spontaneous movement on the left side and multiple episodes of emesis and w as intubated for airway protection. A head CT was completed at that time and is shown below. Her labs are remarkable for an elevated international normalized ratio (INR) of 2.1, Cr 1.4. Vitals are remarkable for blood pressure (BP) 126/88 mm Hg, pulse 80 but irregular.
What is the age of the hemorrhage that is present on the non-contrast head CT?

A. There is only acute subdural hemorrhage.
B. There is mixed acute and subacute subdural hemorrhage.
C. There is mixed acute and chronic subdural hemorrhage.
D. There is only chronic subdural hemorrhage.
E. There is only acute epidural hemorrhage.
Answer: Only acute SDH (A)
The head CT demonstrates an acute large right-sided subdural hemorrhage. This hemorrhage is not limited by the cranial sutures as is the case with an epidural hemorrhage. Subdural hemorrhages are seen in all ages, most commonly due to trauma. Subdural hemorrhages are typically formed from stretching and tearing of bridging veins as they cross the subdural space.
1) In the hyperacute (first hour) phase, the hemorrhage typically will have a swirled appearance due to a mixture of clot, serum, and unclotted blood.
2) An acute subdural hemorrhage is typically a homogenous hyperdense extra-axial collection; however, they can also have areas of unclotted blood causing mixed densities within the hemorrhage.
3) A subacute subdural hemorhage (between day 3 and 21) will become isodense to the adjacent cortex.
4) Lastly, a chronic subdural hemorrhage becomes hypodense and appears similar to cerebrospinal fluid (CSF) and can mimic subdural hygromas.
A 53-year-old woman is recovering in the ICU on postoperative day 2 after undergoing LVAD implantation. Over the course of several hours she is noted to become progressively hypotensive with her mean arterial pressure dropping from 75 to 53 mm Hg as measured by a radial arterial line. Her LVAD monitor shows multiple power spikes in the last 2 hours. Her nurse additionally notes that the patient’ s urine has become much darker in color over the last several hours.
Which of the following is the next best step in management?
A. Complete transthoracic echocardiogram
B. Transesophageal echocardiogram
C. Echocardiographic ramp study
D. CT angiography of the chest
Answer: Echocardiographic ramp study (C)
In this patient with a recently implanted LVAD, hypotension in conjunction with power spikes on the LVAD and clinical signs of hemolysis is strongly suggestive of pump thrombosis, which can be seen as both an early and late complication of VAD therapy.
In addition to laboratory markers of hemolysis, echocardiographic ramp studies during which left ventricular parameters are measured at varying pump speeds have been shown to be both sensitive and specific for pump thrombosis.
Early pump thrombosis generally requires urgent surgical pump exchange or heart transplantation, whereas late pump thrombosis can sometimes be managed with intensified anticoagulation.
Echocardiogram without a ramp study is not helpful in diagnosing pump thrombosis. CT angiography is reserved for selected patients when the diagnosis is challenging after echocardiographic ramp study.
A 56-year-old male with 30-pack year smoking history, CAD, and advanced liver disease due to alcoholic cirrhosis is being evaluated for a liver transplantation. He complains of worsening shortness of breath. His heart rate is 110/min, blood pressure is 97/64 mm Hg, respiratory rate is 32/min, and saturation 90% on 5 L/min nasal cannula. When asked to sit up in bed, the patient states that he“usually breathes better” when lying supine.
Which of the following is the MOST likely pathophysiology behind the diagnosis?
A. Decreased FRC resulting in increasing closing capacity leading to atelectasis
B. Acute on chronic pulmonary thromboembolism
C. Increased production or decreased clearance of endogenous nitric oxide
D. Increased venous congestion leading to pulmonary edema
Answer: Increased Production or Decreased Clearance of Endogenous Nitric Oxide (C)
The development of intrapulmonary vascular dilatations (IVPD) in the presence of advanced liver disease and portal hypertension results in hepatopulmonary syndrome (HPS). Several mediators included nitric oxide, endothelin 1, TNF alfa, and vascular endothelial growth factor have been implicated in the development of these IVPDs. The dilation of these blood vessels results in shunting of blood, leading to V/Q mismatch, hypoxemia, and an increased alveolar arterial oxygen gradient.
These IVPDs tend to occur predominantly in the base of the lungs, resulting in worsening of the shunt while upright. This manifests as platypnea-orthodeoxia.
A 59-year-old female with a history of hypertension and gout is admitted in the ICU for observation status post thrombolysis for ischemic stroke. Her outpatient medications include metoprolol, colchicine, aspirin, metformin, and meloxicam. Vitals are normal except for sinus tachycardia with a heart rate (HR) of 108 beats per minute. Low bicarbonate is noted on labs prompting an arterial blood gas (ABG), and patient is found to be mildly acidotic. Lab values are given below:
Urine Electrolytes:
1. Na—56 mEq/L
2. K—10 mEq/L
3. Cl—56 mEq/L
Which of the following can most likely be expected to be the cause of this?
A. Chronic diarrhea
B. Type 1 renal tubular acidosis
C. Type 4 renal tubular acidosis
D. Bartter syndrome
Answer: Type 4 RTA (C)
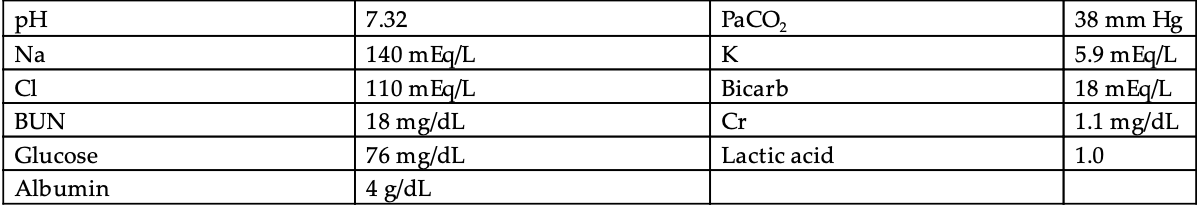
The blood gas suggests a metabolic acidosis. The anion gap is 12, which is appropriate for an albumin of 4. There is no respiratory-driven acidosis component as denoted by normal pCO2 of 38 mm Hg. This patient has a NAGMA. The next step is to calculate the UAG:
[U (Na) + U (K)] - U (Cl) --> (56 + 10) - 56 = 10
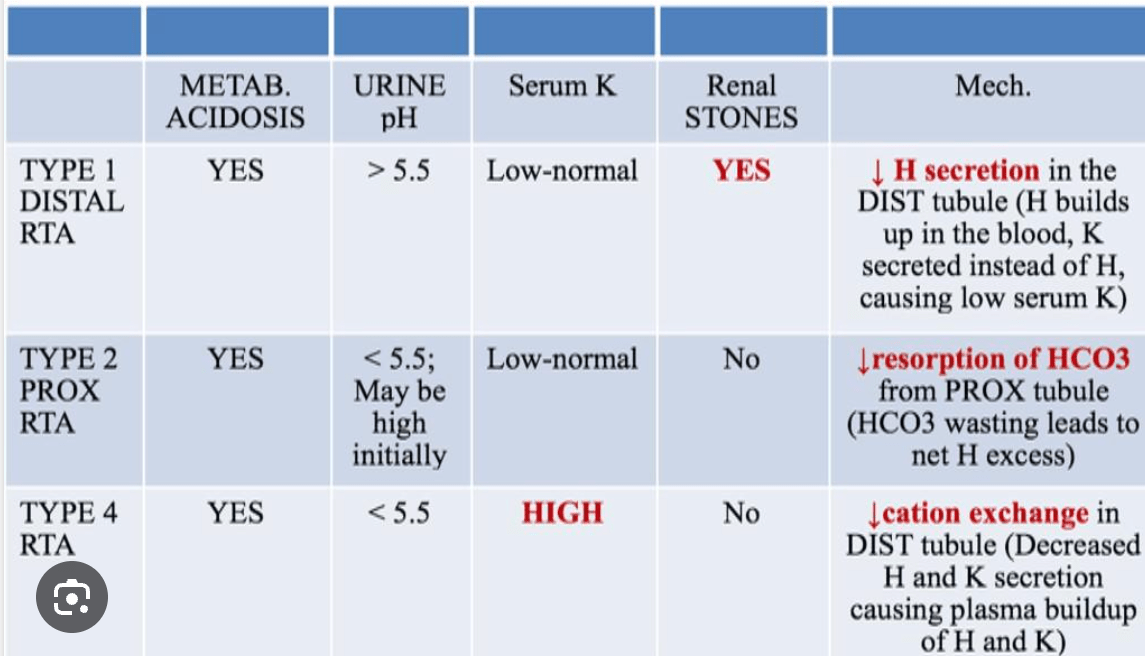
A positive numerical value on UAG in NAGMA can be seen in renal tubular acidosis (type 1 and type 4), spironolactone, and acetazolamide use. Conversely, a negative value on UAG in NAGMA suggests GI etiology. In addition, this patient has serum chemistry consistent with renal tubular acidosis type 4 (hyperkalemia not explained by any other etiology). Types of renal tubular acidosis with their respective differentiating features are depicted in the table below:
A 53-year-old female presents with mydriasis, ptosis, diplopia, dysphagia, dysarthria, and a progressive, symmetric descending flaccid paralysis. She is conscious and has no cardiovascular perturbations. Colleagues at other area hospitals are reporting several similar cases.
You recommend to:
A. Start plasmapheresis or intravenous immunoglobulin and admit her to an intensive care unit (ICU) for close respiratory and cardiovascular monitoring
B. Administer atropine, pralidoxime, anticonvulsants if seizures occur and admit her to an ICU for close monitoring for respiratory failure and risk of aspiration
C. Administer antitoxin, supportive care, and admit her to an ICU for close monitoring for respiratory failure and risk of aspiration
D. Administer edrophonium 2 mg
Answer: Administer antitoxin, supportive care, and admit her to an ICU for close monitoring for respiratory failure and risk of aspiration (C)
Clostridium botulinum produces neurotoxins (types A–G) that block acetylcholine release and affect both nicotinic and muscarinic receptors. Symptoms of botulism include an acute, afebrile, symmetric, descending flaccid paralysis, and prominent bulbar palsies (diplopia, dysarthria, dysphonia, and dysphagia). Blockade of muscarinic receptors result in postural hypotension, nausea, and vomiting from ileus. Respiratory muscle involvement can result in respiratory failure. Mental status is not affected; patients usually have a clear sensorium.
The diagnosis of botulism must be done on a clinical basis as laboratory testing is specialized and requires several days to complete. Differential diagnosis includes Guillain-Barre Syndrome, myasthenia gravis, tick paralysis, organophosphate toxicity, and tick paralysis. Distinguishing features of botulism include prominent cranial nerve palsies initially, symmetric, descending progression, and absence of sensory nerve dysfunction.
Treatment of botulism is largely supportive. Antitoxin should be administered in a timely basis (most effective if given within 24 hours). The antitoxin will limit the severity of disease and subsequent nerve damage but will not reverse existent paralysis.