A 50 yo F recently started a TKI for newly diagnosed CML. She presents to clinic with new shortness of breath with decreased breath sounds bilaterally to mid lungs. What drug is she likely taking?
Sprycel aka dasatinib
Pleural effusion, pericardial effusion, pulmonary hypertension, edema
Discontinue if pulmonary hypertension or recurrent pleural or pericardial effusions
Pt has h/o DVT now on dabigatran. Comes in with massive UGIB 5 hours from last dose. What reversal agent do you give? (Assuming on formulary)
Idarucizumab,
PCC/FEIBA,
Can do dialysis (only oral agent)
17-20h half life
Name the cytoplasmic inclusions
Döhle bodies are single or multiple blue cytoplasmic inclusions that are remnants of rough endoplasmic reticulum. They are associated with myeloid left shifts and are seen in conjunction with toxic granulation. In the upper cell, they can be clearly seen near the cell membrane.
53 yo F w adeno of pancreatic tail. She has h/o breast ca and PALB2 germline mutation. MDT recommends neoadj chemo before surgery. ECOG 0, quite active. Which neoadj regimen do you give?
FOLFIRINOX
Mutations in homologous recombination genes (BRCA 1/2, PALB2) are sensitive to DNA-damaging agents such as platinums. Retrospective survival analysis showed these patients had significantly longer mOS than those wo mutations.
50 yo M w right-sided mCRC meets to discuss starting FOLFOX + bevacizumab. Name (3) labs you plan to monitor while on bevacizumab.
Patients receiving bevacizumab require monitoring of blood pressure, urinary protein, complete blood count, comprehensive metabolic panel, and baseline coags
blood pressure every 2-3 weeks
dipstick urinalysis at every 3-4 weeks
CMP and CBC on day 1 of each treatment cycle, and as clinically indicated throughout therapy
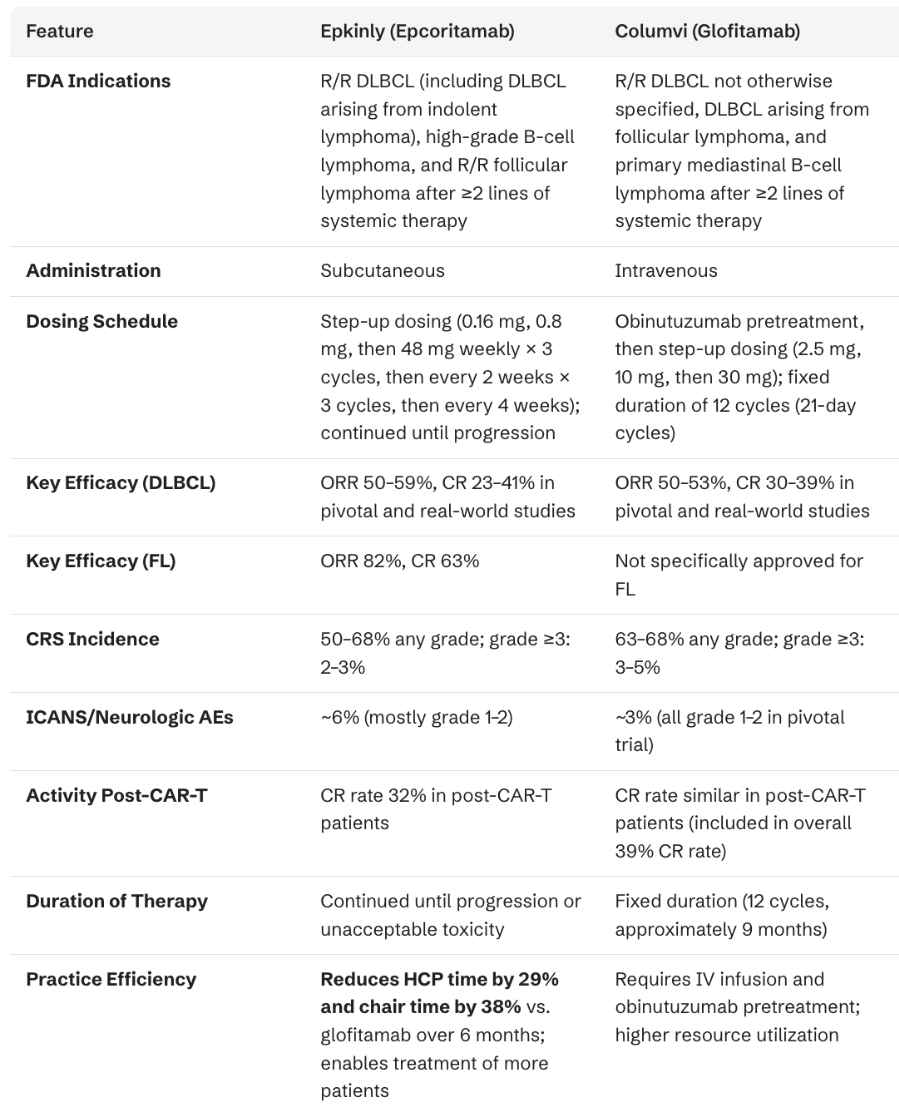
Name (2) bispecific T-cell engaging antibody drugs targeting CD3 and CD20. Both are approved for RR DLBCL.
Epcoritamab aka EPKINLY (also approved for RR FL)
Glofitamab aka COLUMVI
__________ are the most common arterial events in patients with APS
Stroke and transient ischemic attack
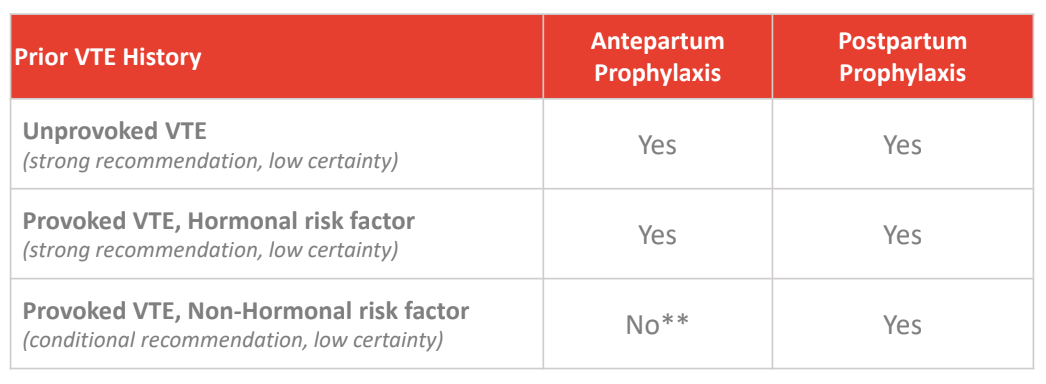
A 36 yo F p/f thrombosis mgmt during her 1st pregnancy. 10 years ago, LLE DVT following car wreck. AC for 3 months. No issue since. Hypercoag testing... reveals heterozygous for FVL. MGM had a DVT. What is the most appropriate AC regimen for her during pregnancy (antepartum and postpartum)?
No antepartum anticoagulation; postpartum prophylaxis only
For low-risk thrombophilia, (heterozygous FVL), antepartum anticoagulation is not recommended. Patients with a history of prior VTE should be considered for post-partum prophylaxis.
50 yo F w chronic HCV p/w abdominal pain. Found to have 5 cm mass in gallbladder w mets to liver. +adenocarcinoma. Genomic profiling of the tumor shows BRAF V600E mutation, TP53 alteration, and microsatellite stability with low TMB. She receives gem/cis/durva w POD after 5 months. Now what?
Dabrafenib and trametinib
5-7% of BTCs have BRAF alterations. ROAR trial w BRAF V600E mutated BTC. RR ~50% w stable disease 35%...
40 yo M w left-sided CRC met to liver currently receiving FOLFOX + cetuximab develops this skin finding. What do you prescribe?

Grade 2-3
For moderate (grade 2) rash, add oral tetracyclines (doxycycline 100 mg twice daily or minocycline)
For severe (grade 3 or higher) rash, cetuximab dose interruption and/or oral corticosteroids are recommended, with urgent dermatology consultation.
Short-term use of higher-potency topical corticosteroids (Class 2 or 3) is preferred over prolonged lower-potency agents.
80 yo F w R/R AML +IDH1 presents to ED unresponsive. Cardiac monitor reveals torsades de pointes. Her family reports she just completed a course of abx for sinusitis. Which targeted therapy was the patient likely taking for her leukemia?
Either IDH1 inhibitor:
Ivosidenib (TIBSOVO) or Olutasidenib (Rezlidhia)
CYP3A4 substrate (major) & P-gp Inducer of CYP3A4, 2B6, 2C8, 2C9
Examples of strong CYP3A4 inhibitors
Antibiotics: Clarithromycin, itraconazole, and ketoconazole
Anti-HIV drugs: Ritonavir, nelfinavir, and saquinavir
Antidepressants: Nefazodone
Other medications: Verapamil and diltiazem (calcium channel blockers)
Herbal and dietary components: Grapefruit juice
As lupus anticoagulant can interfere with INR testing, the accuracy and reliability of using INR (by venipuncture and point-of-care) to monitor vitamin K therapy should be confirmed with what assay?
Chromogenic factor X. If on UFH and LMWH, check an anti-Xa level.
A markedly prolonged PT in the setting of LAC may result from an acquired factor II deficiency, so called lupus anticoagulant hypoprothrombinemia syndrome. This rare complication of APS occurs from an autoantibody that increases the clearance rate of factor II.
Name three drugs a/w an increased risk for sinusoidal obstruction syndrome after allo BMT.
Akylating agents such as Busulfan, cyclophosphamide, melphalan, and carmustine
ADCCs such as gemtuzumab ozogamicin and inotuzumab ozogamicin
combination of sirolimus and tacrolimus esp w inotuzumab
Less likely: Platinum-based agents (oxaliplatin, carboplatin, cisplatin) and thiopurines (azathioprine, mercaptopurine, thioguanine)
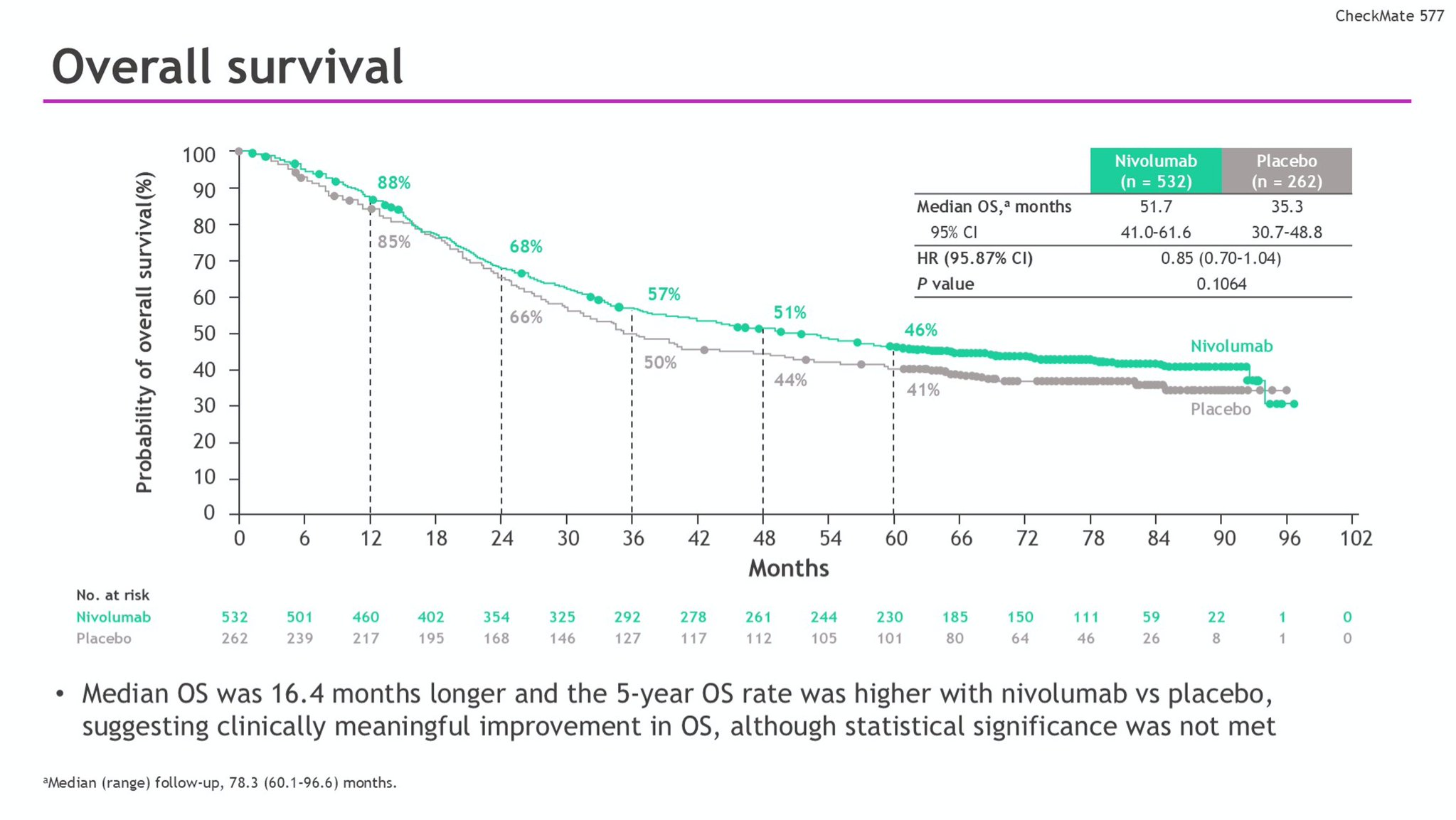
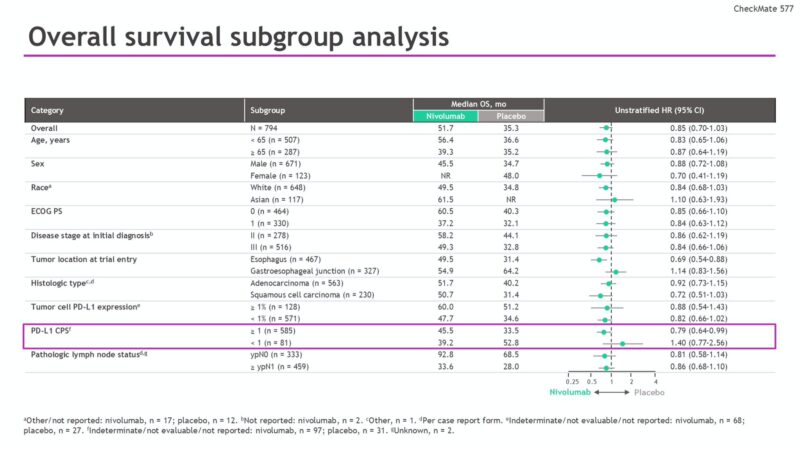
51 yo M w GERD p/w severe dysphagia. EGD w 5 cm fungating mass at GEJ. Bx +poorly differentiated adeno. EUS confirms uT3N2. PET/CT wo distant disease. ECOG 1. Undergoes ccCRT w carbo/Taxol then esophagectomy. Final path ypT2N1 w neg margins. What is the most appropriate next step?
Nivolumab
Neoadj CRT followed by R0 resection w residual cancer in the resection specimen should receive adj nivolumab based on CheckMate 557.
Primary endpoint was DFS* median disease-free survival was 22.4 months (95% confidence interval [CI], 16.6 to 34.0), as compared with 11.0 months (95% CI, 8.3 to 14.3) among the 262 patients who received placebo (hazard ratio for disease recurrence or death, 0.69; 96.4% CI, 0.56 to 0.86; P<0.001).
DFS benefit irrespective of PDL1 status.
35 yo F just received C1 FOLFOX for stage III CRC. She is brought to the ED 3d after administration with altered mental status and new mouth sores. You admit her to the hospital and give her this drug.
If 5-FU toxicity such as DPD deficiency - give uridine triacetate within 96 hours of the end of fluorouracil or capecitabine administration, not within 96 hours of toxicity presentation.
10 grams orally every 6 hours for 20 doses in adults
As of Nov 2025, FDA has issued an important update to the prescribing information for capecitabine, introducing a clear recommendation for genetic testing of DPYD variants before initiating treatment.
Caris Life Sciences has emphasized the importance of comprehensive pharmacogenomic testing by incorporating DPYD analysis into every Caris Assure liquid biopsy performed for therapy selection
The chimeric CD30 antibody-drug conjugate with monomethyl auristatin E (MMAE) payload utilized in cHL and CTCL has a black box warning for what?
Brentuximab vedotin
Progressive multifocal leukoencephalopathy (PML)
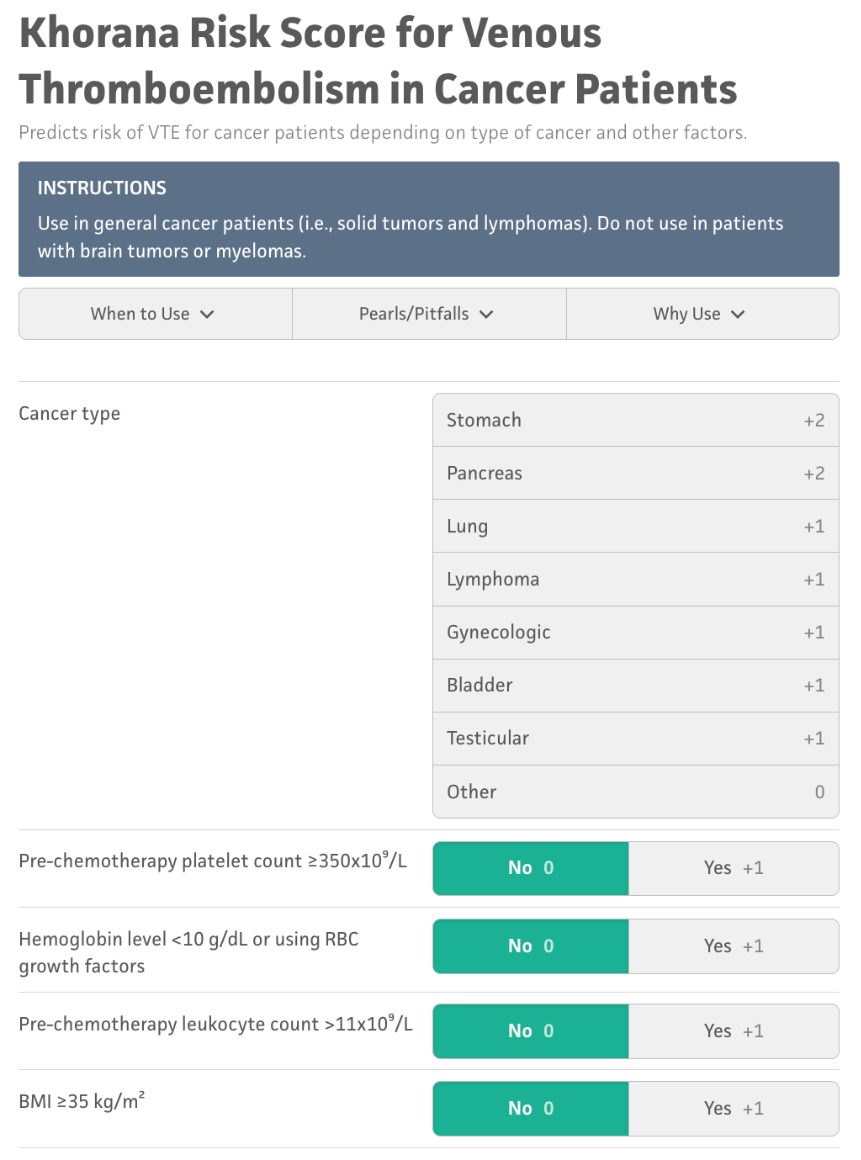
Name one validated risk assessment tool for the classification of VTE risk in people with cancer.
Khorana score (2008)
Modified Vienna CATS score (2018)
Electronic health record (EHR)-CAT score (2023)
Hypomethylating drugs (AZA, Dacogen) inhibit what enzyme?
MOA: Cell cycle specific – S phase
Directly incorporate into DNA & form covalent adducts with DNA methyltransferase, leading to enzyme inhibition and subsequent DNA hypomethylation
+ Reduced protein synthesis via incorporation into RNA (AZA only)
52 yo M w newly diagnosed adenocarcinoma of distal common bile duct extending into pancreatic head. Undergoes pancreaticoduodenectomy w bile duct resection. He is found to have poorly differentiated disease inc N1 nodal involvement with extensive lymphovascular and perineural invasion. Which of these features is the strongest prognostic factor on final path?
LN involvement
and tumor depth are the strongest predictors of disease recurrence in distal bile duct cancer. Poor histologic features (PD, LV/PNI) are unfavorable but less impact on prognosis compared to TNM staging. +LN or +margins can be offered adj CRT.
The Phase III _______ trial in BRAF V600E-mutant mCRC found that the combination of encorafenib and cetuximab (with or without the MEK inhibitor binimetinib) improved ORR compared to the standard of care (irinotecan/cetuximab or FOLFIRI/cetuximab).
BEACON
The triplet regimen showed a higher rate of severe adverse events; therefore, the doublet regimen of encorafenib and cetuximab has been established as a new standard of care for previously treated BRAF V600E mCRC patients due to its improved efficacy and manageable toxicity.

What is the humanized IgG1k monoclonal antibody targeting C-C chemokine receptor 4 (CCR4) approved for RR mycosis fungoides and RR sezary syndrome?
Mogamulizumab aka POTELIGEO (MAVORIC trial)
Increased transplant complications (grade 3-4 GVHD and transplant-related death) in patients who proceed to allogeneic SCT, particularly if a shorter timeframe (~50 days) between mogamulizumab and SCT
30379-6/asset/51b62de3-59c5-4823-86bd-4d0232a05105/main.assets/gr2_lrg.jpg)
Name (3) causes of acquired Protein C, Protein S, and Antithrombin Deficiency:
• Liver disease (C, S, AT)
• Warfarin therapy (C, S)
• Estrogens, pregnancy (S)
• Inflammatory diseases (S)
• Heparin therapy (AT)
• Acute thrombosis (S, AT)
Pentostatin and fludarabine should never be combined due to a high risk of severe and potentially fatal ___________.
This combination is explicitly contraindicated by the FDA and not recommended by the NCCN for any hematologic malignancy
Pulmonary toxicity
The contraindication stems from clinical experience showing fatal pulmonary toxicity when these agents were combined. In a clinical investigation of patients with refractory CLL using pentostatin at recommended doses in combination with Fludara, 4 of 6 patients developed severe or fatal pulmonary toxicity. This led to a black box warning specifically prohibiting their concurrent use.
Randomized, phase 3 study of perioperative durvalumab plus 5-fluorouracil, leucovorin, oxaliplatin and docetaxel chemotherapy (FLOT) demonstrated superior EFS over FLOT plus placebo in patients with resectable, early-stage gastric or gastroesophageal junction (G/GEJ) cancer.
MATTERHORN
D+FLOT demonstrated a statistically significant improvement in EFS vs P + FLOT in pts with resectable GC/GEJC (stage II-IVA), with an encouraging OS and pCR trend. These results support D+FLOT as a potential new global SoC for resectable GC/GEJC. Specifically did not require PD-L1 testing for enrollment.

Randomized trial of standard chemotherapy alone (mFOLFOX6) or combined with atezolizumab as adjuvant therapy for patients with stage III deficient DNA mismatch repair (dMMR) colon cancer
Alliance A021502; ATOMIC (June 2025)
The primary endpoint was DFS; secondary endpoints were OS and adverse event (AE) profile. 3y DFS was 86.4% (95% CI, 81.8 to 89.9) in the atezo arm and 76.6% (95% CI, 71.3 to 81.0) in the mFOLFOX6 arm (HR, 0.50; 95% CI, 0.35 to 0.72). p <0.0001 = new adjuvant standard of care for patients with dMMR stage III colon cancer
What was the first effective cancer immunotherapy?
The administration of high-dose IL-2 represented a seminal breakthrough in cancer treatment. Described in 1985, it was the first clear demonstration that immune manipulations could cause regression of invasive metastatic disease. IL-2 was approved by the FDA for metastatic renal cancer in 1992 and for metastatic melanoma in 1998.
IL-2's ability to expand T cells while maintaining their functional activity enabled the development of subsequent immunotherapies, including tumor-infiltrating lymphocyte therapies and genetically modified T-cell approaches.
A low therapeutic index and suboptimal efficacy restricted its widespread use and impact. These constraints, along with the development of more effective and better-tolerated agents, led to the evolution of modern cancer immunotherapy.
___________'s development of blood staining techniques using coal tar dyes in 1879-1880 revolutionized hematology by enabling the first accurate classification of white blood cells and ending years of speculation about their types, heralding the modern era of leukocyte biology and pathology.
Paul Ehrlich
His use of acidic and basic dyes allowed him to identify eosinophil and basophil granules, respectively, and he developed neutral dyes to recognize neutrophils, which he called "cells with polymorphous nuclei".