Name the 5 layers of thick skin in order from superficial to deep
1.Stratum corneum
- flattened, dessicated, anucleate cells that are filled with keratin. These cells have a thick plasma membrane that's coated with an extracellular lipid layer - this gives the epidermis its water barrier component.
2. stratum lucidum
- doesn't stain well + is seen in thick skin only. is considered a division of the stratum corneum.
3. stratum granulosum
- cells contain numerous, highly-staining keratohyalin granules of irregular shape and size within the cell cytoplasm
4. stratum spinosum
- several layers of cells with lots of short, cytoplasmic processes extending from the cells. These processes attach to other cell processes via desmosomes.
5. stratum basale (lamina lucida, lamina densa)
- single layer of cuboidal epithelial cells which are mitotically active and rest on the basement membrane
What causes acne? What are some ways you can treat it?
Acne vulgaris is a common cutaneous disorder characterized by chronic or recurrent development of papules, pustules, or nodules on the face, neck, trunk, or proximal upper extremities. The pathogenesis of acne vulgaris involves the interaction of multiple factors that result in the formation of comedones and the development of inflammation.
Acne vulgaris is most frequent among adolescents and young adults but is not limited to these ages.
4 main pathogenic factors:
●Follicular hyperkeratinization
●Increased sebum production by sebaceous glands
●Cutibacterium acnes (C. acnes, formerly Propionibacterium acnes), an anaerobic diphtheroid that is a normal component of skin flora
●Inflammation
Treatment options
- Topical retinoids
- Topical benzoyl peroxide
- Oral antibiotics (tetracyclines)
- Hormonal therapies
- Oral isotretinoin
Impetigo is a contagious, superficial bacterial infection observed most frequently in children ages two to five years, although older children and adults may also be affected. It may be classified as primary impetigo (direct bacterial invasion of previously normal skin) (picture 1A-E) or secondary impetigo (infection at sites of minor skin trauma such as abrasions, minor trauma, and insect bites, or underlying conditions such as eczema. Caused

Pyoderma gangrenosum (PG) is an uncommon neutrophilic dermatosis that presents as an inflammatory and ulcerative disorder of the skin. In contrast to its name, PG is neither an infectious nor gangrenous condition. The most common presentation of PG is an inflammatory papule or pustule that progresses to a painful ulcer with a violaceous undermined border and a purulent base. PG may also present with bullous, vegetative, peristomal, and extracutaneous lesions.
More than half of patients with PG develop the disorder in association with an underlying systemic disease. Inflammatory bowel disease, hematologic disorders, and arthritis represent the most frequent comorbidities.
A patient who received a kidney transplant several years ago was recently admitted to the hospital for worsening renal function. He was given increasing doses of prednisone and cyclosporine. Following their administration, he developed skin lesions on his chest and arms (see Figure).

Routine bacterial and fungal cultures are negative.
Which of the following is the most likely diagnosis?
a. candida sepsis
b. staphylococcal sepsis
c. steroid-induced acne
d. varicella (chicken pox)
e. acne vulgaris
steroid-induced acne
What structure is pictured here? (hint: in the epidermis)
Desmosomes
Bullous pemphigoid and mucous membrane pemphigoid (MMP) are uncommon autoimmune subepithelial blistering diseases that most frequently arise in older adults and are characterized by the presence of cutaneous bullae and erosive mucosal lesions. Significant progress has been made in understanding the pathogenesis of these diseases. Multiple events, including the binding of immunoglobulins to basement membrane zone components, the subsequent activation of complement, and the migration of inflammatory cells into the subepithelial tissue, likely contribute to the clinical manifestations of bullous pemphigoid

Rash is the most characteristic finding of secondary syphilis. The rash is classically a symmetric, papular eruption involving the entire trunk and extremities, including the palms and soles (picture 36). Individual lesions are discrete red or reddish brown and measure 0.5 to 2 cm in diameter. They are often scaly but may be smooth and rarely pustular

Skin changes associated with dermatomyositis (DM) include pathognomonic findings, such as Gottron's papules (pink-violaceous papules overlying interphalangeal and metacarpophalangeal joints), Gottron's sign (macular, pink-violaceous erythema overlying other joints, such as the elbows or knees), and the heliotrope eruption (pink-violaceous erythema, with or without edema, involving the periorbital skin). Pink-violaceous erythema of the scalp, V of the neck, shoulders, extensor surfaces of the upper extremities, upper chest, and upper back are additional characteristic findings. Scale may or may not be present but is typically prominent on the scalp, where it may be accompanied by diffuse alopecia
What is the optimal treatment for cellulitis that follows a cut on the hand and is associated with fever, chills, purulence, erythema, and failure to respond to oral dicloxacillin? No recent hospitilizations.
A. IV bactrim
B. Oral clindamycin
C. IV ampicillin
D. IV vancomycin
E. Oral levofloxacin
D. IV vancomycin
Severity of infection and failure to respond to initial therapy warrants IV therapy with an agent that covers S. aureus and S. pyogenes. MRSA coverage isn't necessarily needed without any risk factors.
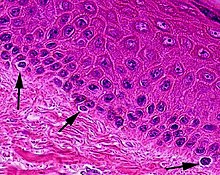
What type of cells are pictured?
Melanocytes
What is the pathogenesis of leukocytoclastic vasculitis?

Cutaneous vasculitis comprises a diverse group of conditions characterized by acute, relapsing, or chronic inflammatory damage to small or medium-sized blood vessels in the skin or subcutaneous tissue. Cutaneous vasculitis can occur as a feature of multiple disorders and exhibits a wide variety of clinical manifestations. Examples of clinical findings include petechiae, palpable purpura, hemorrhagic bullae, nodules, ulcers, livedo reticularis, livedo racemosa, and urticaria.
Although cutaneous vasculitis can be a benign, transient condition, it may also be an indicator of underlying disease or systemic vasculitis. Careful assessment is essential for accurate diagnosis and optimal management. A typical initial evaluation includes a skin biopsy to confirm vasculitis, careful review of the patient history to assess for the etiology of vasculitis, and laboratory tests to assess for systemic involvement. When the cause of vasculitis is uncertain, additional tests may be helpful.

The clinical presentations associated with parvovirus B19 infection vary greatly, ranging from benign to life threatening. The clinical presentation is influenced by the infected individual's age and hematologic and immunologic status.
The five well-established syndromes associated with parvovirus B19 are:
●Fifth disease/erythema infectiosum in children
●Arthropathy
●Transient aplastic crisis in those with chronic hemolytic disorders
●Fetal infection leading to non-immune hydrops fetalis, intrauterine fetal death, miscarriage, or cardiomyopathy
●Pure red blood cell aplasia in immunocompromised individuals

Rash in Rocky Mountain Spotted fever occurs in approximately 88 to 90 percent of patients, but is uncommonly seen at initial clinical presentation. Most patients with RMSF develop a rash between the third and fifth days of illness. Only 14 percent of patients have rash on the first day, and less than one-half develop a rash in the first 72 hours of illness. As a result, rash is often absent when patients first contact a clinician for evaluation
The hallmark of RMSF is a blanching erythematous rash with macules (1 to 4 mm in size) that become petechial over time. However, the evolution of skin rash may vary; some patients may suddenly develop a petechial rash without a prior maculopapular eruption. The appearance of the rash usually begins on the ankles and wrists and spreads to the trunk; rash that appears on the palms and soles is highly characteristic of RMSF, but usually occurs in later-stage disease.
Which of the following treatments is most appropriate for treating a tinea infection involving the hair follicles?
a. oral nystatin
b. topical 1% clotrimazole cream
c. topical 1% clotrimazole cream + 0.05% betamethasone cream
e. oral griseofulvin
E. Oral Griseofulvin
Which structure is pictured here?
Hemidesmosomes are multiprotein complexes that facilitate the stable adhesion of basal epithelial cells to the underlying basement membrane
What is the difference between Stevens-Johnson syndrome and toxic epidermal necrolysis?

Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe mucocutaneous reactions, most commonly triggered by medications, characterized by extensive necrosis and detachment of the epidermis. Mucous membranes are affected in over 90 percent of patients, usually at two or more distinct sites (ocular, oral, and genital).
According to a widely accepted classification, SJS and TEN are considered a disease continuum and are distinguished chiefly by severity, based upon the percentage of body surface affected by blisters and erosions
●SJS is the less severe condition, in which skin detachment is <10 percent of the body surface
●TEN involves detachment of >30 percent of the body surface area (BSA)

Ecthyma is an ulcerative form of impetigo in which the lesions extend through the epidermis and deep into the dermis. They consist of "punched-out" ulcers covered with yellow crust surrounded by raised violaceous margins.

Necrolytic migratory erythema (NME) is the presenting feature of glucagonoma syndrome in approximately 70 to 80 percent of patients. Although the rash can occasionally be the only symptom, in most cases patients have associated systemic symptoms. NME characteristically begins as erythematous papules or plaques involving the face, perineum, and extremities. Over the ensuing 7 to 14 days, the lesions enlarge and coalesce. Central clearing then occurs, leaving bronze-colored, indurated areas centrally, with blistering, crusting, and scaling at the borders. The affected areas are often pruritic and painful. The same process often affects the mucous membranes, resulting in glossitis, angular cheilitis, stomatitis, and blepharitis
Glucagonoma syndrome is thought to be directly related to elevated glucagon levels. Glucagon, acting on the liver, increases both amino acid oxidation and gluconeogenesis from amino acid substrates. The weight loss characteristic of glucagonoma may result from the catabolic action of glucagon and through glucagon-like peptides such as GLP-1. Necrolytic migratory erythema probably results from hyponutrition and amino acid deficiency
A 67 y.o M with DM2 presents with a chronic skin ulcer that began as a 2-cm laceration 3 months ago. It has worsened despite initial therapy with mechanical debridement and is now 10cm x 6cm with a necrotic, bloody, yellowish, ragged base and edematous, dusky purplish-gray overhanging borders. He has normal pulses. What is the most appropriate next step in management?
A. Angiography
B. Admission for broad spectrum antibiotics
C. Vacuum assisted closure dressing
D. Perform a skin biopsy for histopathology and tissue culture
E. Sharply debride any necrotic-appearing tissue
D. Perform a skin biopsy for histopathology and tissue culture
Chronic ulcers that do not respond to conventional therapy should be evaluated for atypical causes such as mycobacterium, vasculitis, fungal infections, malignancy, and pyoderma.
What is the function of Langerhans cells and what layer of skin are they found in?
Langerhan cells are involved in the immune response:
recognize, phagocytose, and process antigen processing cells
found in the basal layer of cells
Explain the pathophysiology of atopic dermatitis

Atopic dermatitis is a chronic, pruritic, inflammatory skin disease that occurs most frequently in children but also affects adults. Atopic dermatitis is often associated with an elevated serum level of immunoglobulin E (IgE) and a personal or family history of atopy, which describes a group of disorders that includes eczema, asthma, and allergic rhinitis.
The epidermal barrier function primarily resides in the stratum corneum, which consists of vertical stacks of anucleate corneocytes packed with keratin filaments embedded in a matrix of filaggrin breakdown products, ceramides, cholesterol, and free fatty acids. The stratum corneum provides the first line of defense against the environment, including pathogens and allergens, and controls water homeostasis. An altered stratum corneum, therefore, results in increased transepidermal water loss, increased permeability, reduced water retention, and altered lipid composition
Epidermal barrier dysfunction is the key abnormality in the pathophysiology of atopic dermatitis, hence the importance of moisturizers and emollients in the management of atopic dermatitis.
Epidermal barrier dysfunction is caused by multiple factors, including reduced filaggrin production, imbalance between stratum corneum protease and antiprotease activity, and tight junction abnormalities.

Granuloma annulare (GA) is an often self-limited disorder that can affect both children and adults. Localized GA, which classically presents as an erythematous or skin-colored, annular plaque without scale, is the most common form of GA. The generalized form of GA, which accounts for approximately 15 percent of cases, typically presents with numerous papules and plaques on the trunk and extremities. Less common forms of GA include subcutaneous, perforating, and patch variants. Many cases of GA resolve spontaneously within a few years

An evanescent, macular, salmon-pink rash is frequently present in Systemic juvenile idiopathic arthritis. It usually consists of multiple round to oval macules that are slightly raised and are of differing sizes. The smaller ones have a slight pallor surrounding them, and the larger ones commonly exhibit central pallor. The rash may not be noticed, because it is often only in scattered locations, is fleeting, and may not be very prominent. Additionally, the rash may be difficult to see in darker-skinned individuals. Thus, careful inspection of the skin is important when sJIA is suspected. The rash is brought out by heat and touch and is often found in the axillae and around the waist but may be present anywhere on the body. It is most prominent when the child is febrile. Unlike viral exanthems, which persist, the rash often fades as the temperature returns to normal, only to reappear with the next fever spike. The rash also may appear following stroking of the skin or other minor trauma (Koebner phenomenon). The rash can be intensely pruritic in some patients. It can become somewhat confluent and become urticarial in appearance, especially in those patients who scratch themselves because of the pruritus
What is the most appropriate work up for a patient who presents with chronic xerosis, erythema, and lichenification over the anticubital fossa and popliteal fossa?
A. Skin allergy testing
B. Skin scraping and KOH prep
C. Measure serum IgE levels
D. Blood testing for food alergies
E. Nothing
E. Nothing