What does articular cartilage look like on radiographs?
Nothing. You cannot see it.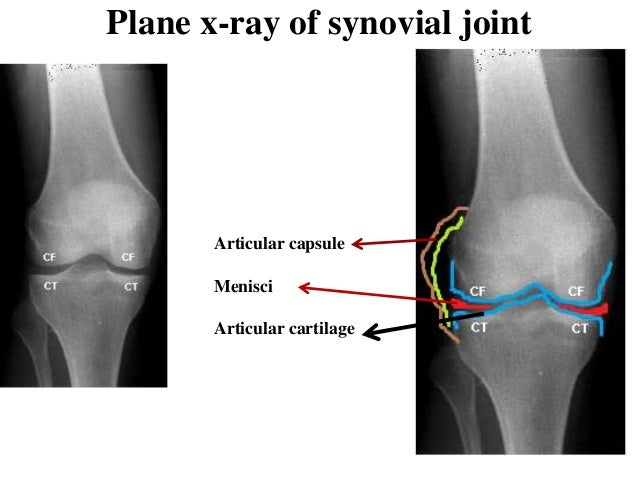
Is all joint narrowing real on rads?
No, in NWB rads there can be false changes. This is less of a problem in LA due to most rads being performed fully weight bearing.
What is the pathogenesis of patella luxation?
Usually occurs in toy and small breeds but can occur in large breeds as well. Medial is usual for small dogs. Lateral is usual for large dogs. Common in conjunction with angular limb deformity. Can be traumatic as well. Predisposes to OA.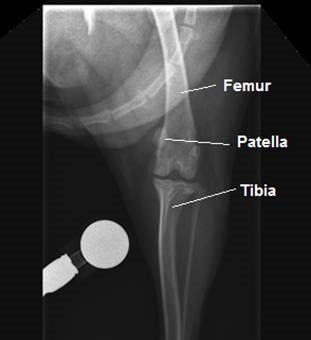
Most common joint neoplasia? Pathology?
Synovial sarcoma. Most commonly in stifle or elbow. Soft tissue mass appearance. Will eventually lyse adjacent bone on BOTH sides of the joint. Usually only one joint effected. Need biopsy to confirm.

Name and describe the portions of long bones
Epiphysis, metaphysis, physis, diaphysis, and apophysis

What hints at articular cartilage damage?
Changes in subchondral bone.
How does hip dysplasia happen?
Usually occurs in large breed, fast growing dogs. (Can happen in small dogs and cats). MULTIFACTORIAL with a genetic component. NOT congenital. Results in OA.
Examples of erosive inflammatory / infectious polyarthropathies?
Rheumatoid arthitis, feline periosteal proliferative polyarthritis, and other various infectious agents.
Radiograph views for diagnosis of fracture?
2 orthogonal views. Include joint proximal and distal to fracture. May need oblique to fully classify the fracture. SEDATE these poor animals.

Young animals due to open growth plates.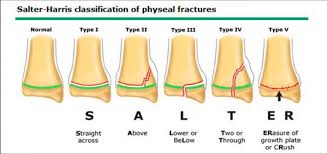
What is OA? How does it happen?
Osteoarthirits or degenerative joint disease. Primary: aging or wear & tear. Secondary: Instability, infection, developmental or acquired disease.
What are signs of hip dysplasia on rads?
Poor acetabular coverage of femoral head, joint incongruity, sub or total luxation, misshapen femoral head, thickened femoral neck, and progressive OA.
Examples of non-erosive inflammatory / infectious polyarthropathies?
Systemic lupus erythematous (SLE), canine immune mediated polyarthritis (IMPA), feline non-erosive immune mediated polyarthritis, and various other infectious agents.
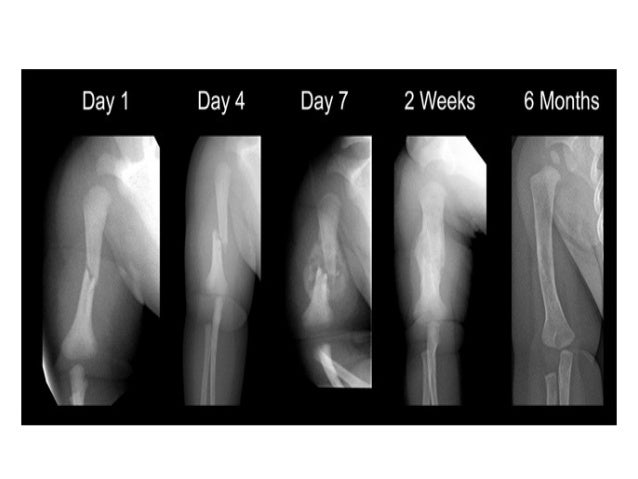
What are the most common bone lesion that are difficult to see?
Non-displaced, compression, and pathologic. If unsure retake in ~7 days due to bone resorption time.

What is an avulsion fracture?
Fracture at site of soft tissue attachment where a portion of bone is pulled away

Signs of OA
Joint effusion, osteophyte production, joint space narrowing, subchondral bone sclerosis (erosion), sunchondral bone cyst-like lesion formation.
What is CCL disease?
Common in large breed dogs, partial or complete rupture of cranial cruciate destabilizes stifle joint. It is often characterized as an acute and NWB lameness. Cranial subluxation (drawer) of the tibia occurs when WB.
Signs of erosive polyathritis
Joint distenion, multifocal lysis, destruction of articular surfaces, and joint space narrowing secondary to articular cartilage loss
Fracture naming rules?
Bones involved, location within bone, morphology of fracture, displacement of distal portion, open or closed, and articular or not.

Primary vs secondary bone healing
Primary: direct extension of bone without intermediate tissue or callus, only seen with internal plate fixation (surgery), fracture gap must be less than 1mm.
Secondary: Inflammation / hematoma, fibrous callus (10-20 days), bony callus (30+ days), and then remodeling (3+ months). Still need reduction of fracture. MOST COMMON type of healing.
Osteophytes vs. enthesophytes
Osteophytes: new bone formed at margins of joint surface. Enthesophyte: new bone formed at attachment sites of tendons, ligaments, and joint capsule. ALL ENTHESOPHYTES ARE OSTEOPHYTES BUT NOT ALL OSTEOPHYTES ARE ENTHESOPHYTES.
ARE ENTHESOPHYTES.
What are rad signs of CCL rupture?
Joint effusion, possible avulsion fragment from insertion site on tibial plateau (particularly in young dogs), and progressing OA. 
Signs of non-erosive polyarthritis
Intracapsular swelling, NO subchondral bone lysis, and multiple joints involved. Carpus and tarsus most commonly involved
Site of tendon or ligament insertion

What makes a nonunion fracture non-viable?
A lack of blood supply to the site.