This is the antidote for anticholinergic toxicity.
What is physostigmine?
A 56-year-old man is evaluated for possible smoldering myeloma. Medical history is unremarkable, and he takes no medications. Serum protein electrophoresis and immunofixation show an IgA protein spike of 3.5 g/dL (35 g/L). Bone marrow biopsy reveals 50% clonal plasma cells. Whole-body low-dose CT scan is negative for bone lesions. This is the most appropriate imaging test to perform next.
What is whole body MRI?
Smoldering multiple myeloma (MM) is characterized by a serum M protein level of 3 g/dL (30 g/L) or greater (or ≥500 mg/24 hr of urinary monoclonal free light chains) or bone marrow plasma clonal cells of 10% to 59% and no evidence of myeloma-related signs or symptoms. CT is preferred because of its relatively high sensitivity, speed, and patient convenience. If initial imaging with whole-body low-dose CT is negative, whole-body MRI is recommended. MRI has been found to be more sensitive in identifying myeloma-related bone lesions and soft tissue lesions from plasmacytoma but is more inconvenient for the patient. If more than one lesion greater than 5 mm is discovered, the patient should be considered to have MM requiring therapy. In this patient with smoldering MM, negative findings on whole-body low-dose CT scan does not exclude skeletal lesions, and MRI is needed for further evaluation.
A 60-year-old woman presents with chest pain that started today and describes it as sharp and brief. When she sits up, the pain improves. This is the most likely diagnosis.
.jpg)
What is pericarditis?
A 40-year-old man is hospitalized for acute pericarditis. He also reports pain in the wrists, ankles, and knees for 1 week but no other symptoms. He has otherwise been well and takes no medications.
On physical examination, temperature is 38.0 °C (100.4 °F); the remainder of the vital signs are normal. A pericardial friction rub is present. The wrists, knees, and ankles are tender. There are small bilateral wrist and knee effusions. The remainder of the examination is unremarkable.
Hematocrit 30%
Leukocyte count 4000/μL (4.0 × 109/L), with lymphopenia
Platelet count 72,000/μL (72 × 109/L)
C-reactive protein 5.5 mg/dL (55 mg/L)
Creatinine 1.4 mg/dL (123.8 μmol/L)
Urinalysis 1+ protein, 1+ blood; 2-3 erythrocytes; no leukocytes; no casts
This is most likely cause of this patient's pericarditis?
What is systemic lupus erythematosus (SLE)?
Factors that suggest SLE as the cause of this patient's pericarditis include joint swelling, evidence of possible kidney disease, and cytopenias, particularly thrombocytopenia. All of these are seen in SLE. Pericarditis is a relatively common manifestation of SLE and can be asymptomatic (most commonly) or can cause chest pain and myopericarditis; tamponade is rare.
These are the valves that have been replaced.
What are the aortic and mitral valves?
This patient had her mitral and aortic valves replaced with Starr-Edwards devices for severe rheumatic aortic and mitral stenosis.
This is the antidote for methemoglobinemia.
What is methylene blue?
NADPH-dependent reduction to leucomethylene blue due to action of methaemoglobin reductase -> reduces methaemoglobin -> Hb
A 70-year-old man undergoes routine follow-up evaluation of low-risk prostate cancer diagnosed 3 years ago. He reports no symptoms. He has been managed with active surveillance. His last biopsy was 18 months ago. His prostate-specific antigen (PSA) level was 4.5 ng/mL (4.5 µg/L) 1 year ago and is now 9.2 ng/mL (9.2 µg/L). He takes no medications. On physical examination, vital signs and all examination findings are unremarkable. This is the most appropriate management.
What is repeat prostate biopsy?
- In men with low-risk prostate cancer, active surveillance is a reasonable strategy because some men will never require treatment, and outcomes are no worse if men with low-grade cancer are treated at the time of progression rather than when first diagnosed.
- In men undergoing active surveillance for prostate cancer, a doubling time of less than 3 years is grounds for reassessment with a repeat biopsy.
This is the patient's diagnosis.
What is hyperkalemia?
The electrocardiogram shows a regular rhythm, with a widened QRS complex in a sine-wave configuration, and there no discernible P waves. The T waves were fused with the widened QRS complexes to form the sine-wave pattern (sinoventricular rhythm). The patient's serum potassium level was 9.1 mmol per liter. His condition stabilized after the administration of calcium chloride, bicarbonate, glucose, and insulin therapy, which was followed by hemodialysis.
A 60-year-old man is evaluated in follow-up after an episode of podagra, which was treated with colchicine. This was his first gout flare. He also has hypertension and hyperlipidemia. Current medications are hydrochlorothiazide and atorvastatin. On physical examination, blood pressure and other findings are normal. Laboratory evaluation reveals a serum urate level of 9.0 mg/dL (0.53 mmol/L).
This is the most appropriate treatment.
What is stop HCTZ and switch to another anti-hypertensive like losartan?
This patient has had a first episode of podagra (gout of the great toe) treated effectively with colchicine. He has a minimally elevated serum urate level. Hydrochlorothiazide and other loop diuretics cause hyperuricemia and may have contributed to this gout episode. For patients with gout, the American College of Rheumatology (ACR) conditionally recommends switching hydrochlorothiazide to an alternate antihypertensive, losartan preferentially, when feasible.
This is the diagnosis.
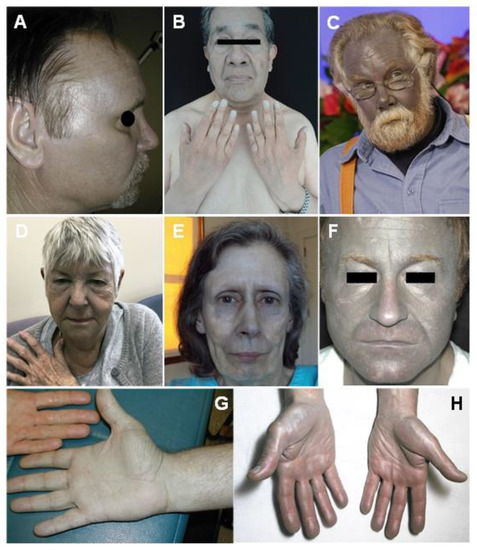
What is argyria?
Generalized argyria is caused by systemic silver exposure (heavy exposure to silver among people who worked with the metal and the use of silver to treat diseases) leading to an irreversible darkening of skin pigmentation. The changes in skin color are most prominent in sun-exposed areas, because sunlight catalyzes the reduction of elemental silver.
This is the antidote for arsenic poisoning.
What is dimercaprol?
29-year-old woman is evaluated in the emergency department for epistaxis and bleeding gums that began 3 days ago. Medical history is otherwise unremarkable, and she takes no medications.
On physical examination, temperature is 36.7 °C (98.0 °F), blood pressure is 110/80 mm Hg, pulse rate is 120/min, and respiration rate is 22/min. Dried blood is seen in her nose, and gingival bleeding is noted. No lymphadenopathy or hepatosplenomegaly is present. Petechiae are present on the lower extremities.
Laboratory studies:
Hemoglobin 8.9 g/dL (89 g/L)
Leukocyte count 14,000/μL (14 × 109/L) (19% neutrophils, 3% bands, 32% lymphocytes, 15% monocytes, and 31% “atypical” cells)
Platelet count 8000/μL (8 × 109/L)
The prothrombin time, activated partial thromboplastin time, and INR are elevated; fibrinogen level is low, and fibrin degradation products are elevated.
This is her diagnosis.

What is Acute Promyelocytic Leukemia?
Although anemia and thrombocytopenia from marrow infiltration can be associated with any acute leukemia, presentation with disseminated intravascular coagulation is characteristic of acute promyelocytic leukemia. Auer rods are seen in the peripheral smear.
58-year-old man with coronary artery disease presented to the emergency department with a 1-day history of intermittent chest pain at rest. Based on the EKG, this is the coronary artery with complete occlusion.
What is the Left Anterior Descending artery?
The EKG raised concern for Wellens’ syndrome, a pain-free period after spontaneous reperfusion of an occluded left anterior descending artery identified by biphasic or deep precordial T-wave inversions, particularly in leads V2 and V3. Shortly after being examined, the patient began having chest pain. Emergency cardiac catheterization identified a complete occlusion of the proximal left anterior descending artery.
A 29-year-old man is evaluated after an episode of anterior uveitis. He has 2-year history of low back stiffness at night and in the morning that improves with activity. Current medication is meloxicam as needed.
On physical examination, he cannot touch his toes, and there is flattening of the normal lumbar lordosis. Internal rotation and flexion elicit pain in the right hip; range of motion of the right hip is diminished. Flexion, external rotation, and abduction of the hips cause pain in the right hip and low back.
This is the likely diagnosis and most appropriate diagnostic test to perform next.
What is ankylosing spondylitis and anteroposterior radiography of the pelvis?
This patient has had classic inflammatory low back pain for several years. Flexion, external rotation, and abduction of the hips elicit pain in this patient's right hip as well as low back pain. These findings, along with involvement of the right hip, suggest ankylosing spondylitis (AS). This patient was diagnosed with uveitis. Spondyloarthritis accounts for approximately 40% of cases of acute anterior uveitis in the United States, and most of these patients will have AS. Acute anterior uveitis has been reported to affect 27% of patients with AS and rarely causes permanent visual damage.
A 35-year-old man with IgA nephropathy presented with confusion, blurry vision, and seizures. Two weeks before presentation, he had started receiving cyclosporine. Physical examination was notable for a blood pressure of 160/80 mm Hg, drowsiness, and decreased visual acuity. A fundoscopic examinations was normal. T2-weighted magnetic resonance imaging (MRI) with fluid-attenuated inversion recovery sequencing of the head was performed. This is the most likely diagnosis.
What is posterior reversible encephalopathy syndrome?
A diagnosis of PRES due to cyclosporine use was made. One week after cyclosporine therapy was stopped, the patient’s symptoms and MRI findings had resolved.
This is the antidote for tylenol toxicity.
What is N-acetylcysteine (NAC)?
According to the 2020 American Society of Clinical Oncology guideline on VTE prevention and treatment in patients with cancer, routine pharmacologic thromboprophylaxis should NOT be offered to all outpatients with cancer. Increased thrombotic risk in patients with cancer is measured using this score. The guideline recommends that high-risk outpatients with cancer (score of 2 or higher before starting a new systemic chemotherapy regimen) may be offered thromboprophylaxis.
What is the Khorana Risk Score?
Cancer type: (Stomach and Pancreas 2 pts, Lung, Lymphoma, Gynecologic, Bladder, Testicular 1 pt, all other 0 pts)
Pre-chemotherapy platelet count ≥350x10⁹/L - 1pt
Hemoglobin level <10 g/dL or using RBC growth factors - 1pt
Pre-chemotherapy leukocyte count >11x10⁹/L - 1 pt
BMI ≥35 kg/m² - 1pt
68 year old male presenting with syncope. This is the EKG finding.
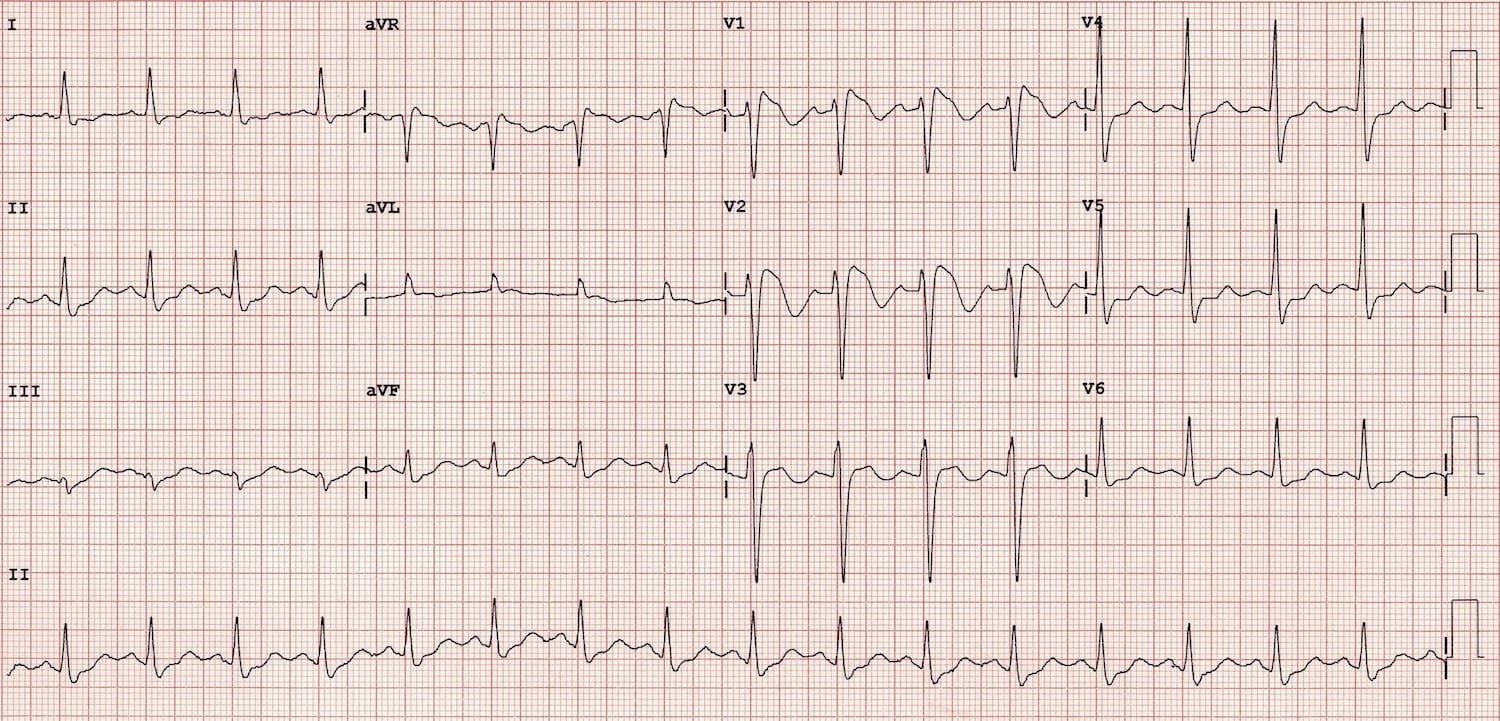
What is Brugada Type I?
- Coved ST segment elevation >2mm in >1 of V1-V3 followed by a negative T wave.
A 78-year-old woman is evaluated for constant bilateral headache of 1 week's duration. Two months ago, she was diagnosed with polymyalgia rheumatica. Symptoms were relieved with prednisone, 15 mg/d. Headache appeared shortly after the dosage was tapered to 5 mg/d. She also has experienced new-onset intermittent muscular jaw discomfort with chewing.
On physical examination, vital signs are normal. The scalp and temporal arteries are not tender to palpation. No bruit is heard over the great vessels; temporal artery pulses are intact.
Laboratory evaluation shows a blood C-reactive protein level of 12.8 mg/dL (128 mg/L).
This is the most likely diagnosis.
What is giant cell arteritis (GCA)?
This patient has polymyalgia rheumatica, and 10% to 20% of patients with polymyalgia rheumatica have concomitant GCA at presentation or develop GCA later in the disease course. Headache is present in more than 60% of patients with GCA and may be frontal, occipital, unilateral, or generalized; it may be constant, intermittent, or waxing and waning. The important point is that the headache is new. A frequent nonheadache manifestation of GCA is jaw claudication, owing to decreased blood flow to the muscles of mastication. Jaw claudication is found in nearly 50% of patients with GCA, and this symptom should always be explored on review of systems in a patient with polymyalgia rheumatica. Other key questions to ask such patients include whether they have recent changes in vision (e.g., short-lived episodes of amaurosis fugax, diplopia, or blurriness) and scalp tenderness (e.g., with hair brushing). A blood C-reactive protein level of 12.8 mg/dL (128 mg/L) would be unusual for polymyalgia rheumatica alone; this degree of systemic inflammation is more in keeping with a vasculitis, such as GCA.
What is spontaneous coronary-artery dissection?
Spontaneous coronary-artery dissection is an uncommon cause of acute coronary syndrome that predominantly affects women without typical cardiovascular risk factors. Most patients with the condition can be treated medically when there is normal flow in the distal artery, as in this case in which no stent was placed.
This is the antidote for digoxin toxicity.
What is Digibind or Digoxin-specific antibody Fab fragments?
62-year-old woman undergoes follow-up evaluation for epithelial ovarian cancer. She underwent surgical debulking with optimal cytoreduction, and the primary tumor and visible metastases were all resected. She completed platinum-taxane chemotherapy and has no evidence of disease recurrence. Germline genetic testing revealed a BRCA1 mutation. Her medical history is otherwise unremarkable, and she takes no medications. On physical examination, vital signs are normal. There is a well-healed laparotomy incision. This is most appropriate additional treatment for this patient.
What is a poly (ADP-ribose) polymerase (PARP) inhibitor?
This patient has advanced epithelial ovarian cancer and a germline BRCA1 mutation and should receive maintenance therapy with a poly (ADP-ribose) polymerase (PARP) inhibitor. For BRCA1 or BRCA2 mutation carriers with complete or partial response to first-line platinum-based chemotherapy, the addition of a maintenance PARP inhibitor is associated with substantial improvements in progression-free survival. PARPs are involved in repair of single-strand breaks. PARP inhibition leads to DNA breaks that activate homologous recombination (HR) repair. Patients with BRCA mutations have defective HR repair, which results in an error-prone repair mechanism that cannot repair these breaks, leading to cell death. In this way, PARP inhibitors are cytotoxic for cancer cells, especially those with a germline or somatic BRCA1/2 mutation.
35 year old female with sudden onset of palpitations. The administration of adenosine caused the patient to go into ventricular fibrillation. This is the most likely diagnosis. 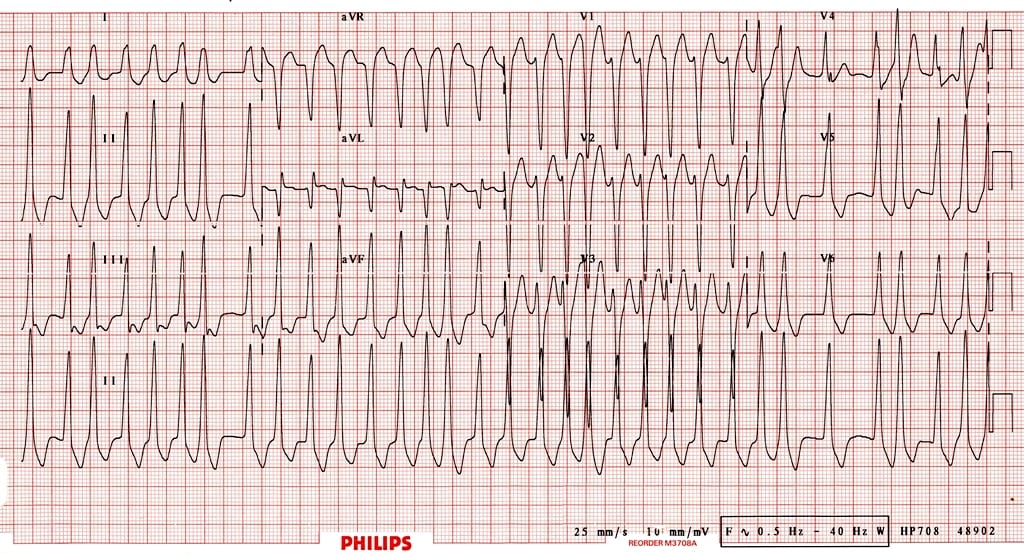
What is atrial fibrillation with Wolff-Parkinson-White (WPW) pattern?
- Irregular rhythm, with extremely high rates in some places — up to 300 bpm (this is too rapid to be conducted via the AV node)
- Wide QRS complexes due to abnormal ventricular depolarization via accessory pathway
- Subtle beat-to-beat variation in QRS morphology
- The administration of AV nodal blocking drugs preferences conduction via the AP, and may precipitate ventricular arrhythmias and cardiac arrest
A 46-year-old man is evaluated for a 5-year history of pain in the lower spine, knees, and hands. The hand pain is associated with occasional swelling. Morning stiffness lasts less than 30 minutes. Type 2 diabetes mellitus was diagnosed 2 years ago. His only medication is metformin.
On physical examination, there is bilateral enlargement of the second, third, and fourth metacarpophalangeal joints as well as all proximal and distal interphalangeal joints. The medial joint line of each knee is tender to palpation.
Alanine aminotransferase 48 U/L
Aspartate aminotransferase 52 U/L
Calcium Normal
C-reactive protein Normal
Ferritin Elevated
Transferrin saturation Elevated
This is the most appropriate diagnostic test to perform next.

What is HFE gene testing?
Underlying disorders can predispose patients to the development of secondary osteoarthritis (OA) and should be suspected when OA occurs at an early age or involves joints not typical for OA, such as the metacarpophalangeal (MCP) or shoulder joints. This patient has hook-shaped osteophytes of the second, third, and fourth MCP joints; onset of type 2 diabetes mellitus in the last few years; abnormal aspartate and aminotransferase levels; and elevated serum ferritin and transferrin saturation levels, all suggesting hereditary hemochromatosis. The HFE gene mutation is diagnostic for this condition, and testing should be performed.
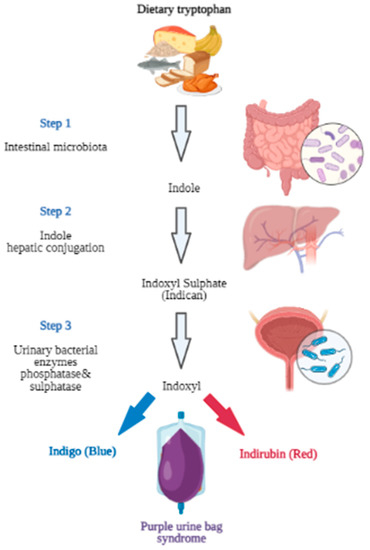
This amino acid is responsible for this phenomenon.

What is tryptophan?
The characteristic purple color is the result of the presence of predominantly Gram-negative bacteria in the urine. The mechanism of the characteristic discoloration of the Foley bag and the urine involves specific microbial enzymes. Bacteria-derived indoxyl sulfatase and phosphatase cause blue (indigo)- and red (indirubin)-pigmented breakdown products of dietary amino acid tryptophan metabolite (indoxyl sulfate). The different proportions of these two pigmented metabolites produce various shades of discoloration, ranging from purple and blue to a reddish color.