What does the "PINCH" acronym stand for?
PINCH meds are high risk meds.
*Potassium (concentrated electrolytes)
*Insulin (IV insulin & U-500)
*Narcotics
*Chemotherapy
*Heparin agents (all anticoagulants)
Your patient reports having no pain. When should this patient’s pain next be assessed and documented?
At the next change in caregiver or sooner if the patient develops pain and requires a dose of PRN pain medication.
When should a peripheral IV site be assessed?
At least once a shift and prior to accessing/ flushing the line
Your patient has a red, non-blanchable area to the coccyx. The doctor has put in a wound consult – do you think this is necessary?
No. A wound consult is not necessary for Stage 1 or Stage 2 pressure injuries (except in rare circumstances). The doctor can d/c this wound consult and this Stage 1 can be managed by floor nursing.
When you are clicking “special stream” during your patients’ hourly rounds – what are you acknowledging?
1. Bed alarm is on
2. Chair alarm is on and green light is blinking
3. Correct signage in place
4. Clear pathway in room
5. Treaded slipper socks on
6. IV pole on preferred side of bed exit
7. Bed in the lowest and locked position
8. Call light within reach
9. Instruct patient and family to call for assistance getting out of bed/ chair
True or False: Your patient is ordered for U-500, you can draw this up in an insulin syringe and administer as you would any other insulin.
False. U-500 insulin is drawn up in a TB syringe, prepared by the pharmacy, and sent to the floor.
List four non-pharmacologic methods of pain management
*ice
*heat
*relaxation
*guided imagery
*reiki
*music therapy
*distraction
*meditation
*massage therapy
How often must you document the assessment of insertion site and dressing of your venous access?
At least once daily
Your patient is admitted to the hospitalist/ medicine service with an abdominal wound vac. Surgery is not following this patient in house. The patient is due for a wound vac dressing change, who is responsible for this?
Nursing! Nurses can change wound vac dressings – wound care does not routinely follow all wound vacs. You can reach out to the wound team, UBE and/ or CNS for assistance with a wound vac dressing change – we are happy to help!
True or False: When administering meds through a G-tube, you can crush all meds and administer together.
False. Meds must be crushed individually and put through the G-tube individually.
Your patient is receiving IV fluids at 100mL/hr, and the MD just ordered a heparin drip to be started STAT. Should you obtain a second IV access?
You may Y-site heparin into the fluid if the fluid is compatible with heparin. If the fluid and heparin are not compatible, then it would be correct to get a second access.
What must you document after giving your patient a PRN albuterol nebulizer?
Document the effect in your nursing note.
Your patient has a peripheral IV in their left hand. Where should the insertion date and dressing date of this PIV be written?
a. The saline lock should be flagged with a date and the dressing change date should be documented directly on the dressing.
b. This should be documented in your daily nursing note.
How wound you describe this wound?
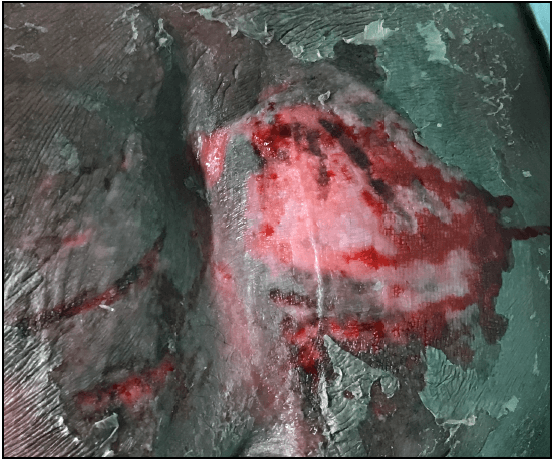
- pink, red, black
- moist/ bleeding in areas
- dry, flakey skin surrounding wound
- what does this feel like? is there an odor? how much drainage?
Your patient is ordered for a fixed dose of Humalog at lunch time, as well as a sliding scale dose of Humalog. The patient is ordered for a regular diet but is not going to eat lunch. Which insulin should you give?
In most circumstances it is recommended to give the sliding scale insulin, but it is important to have a conversation with the physician to confirm.
Your patient is ordered for a Fentanyl patch q72 hours and is due for a new patch at the start of your shift. When you remove the old Fentanyl patch, what should you do with it?
The old patch should be cut in half, disposed of in the sharps container, witnessed by another nurse, and recorded in the Omnicell.
(Even though this patch is due to be removed, there may still be a scant amount of Fentanyl left on the patch. When wasting this in the Omnicell, you can write "one patch", as we don't know the exact amount left on the patch.)
You just gave your patient 10mg of PO Oxycodone for 7/10 back pain. When should you re-assess the patient’s pain?
Consider the onset of action. You should re-assess this patient’s pain within an hour. Patients who receive IV pain medication should be reassessed in 15- 20 minutes.
When is IV tubing due to be changed?
a. every four days
b. with a new venous access
c. if tubing is left uncapped, linked back into itself, or has been contaminated in some way
What would you do for this wound?
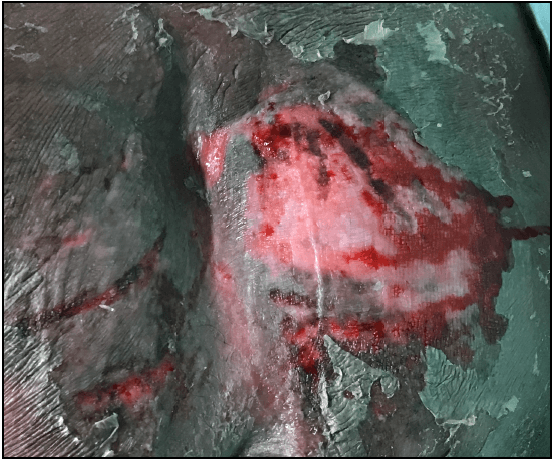
-clean it
-measure it
-dress it (*there are many options!)
-alert MD
-wound consult
-safety report if thought to be pressure related
Your patient’s PICC was inserted yesterday in IR. Dressing is C/D/I at this time – when is dressing due to be changed?
a. If there is a pressure dressing with insertion site covered, dressing should be changed in 24 hours from placement of dressing.
b. If no pressure dressing, dressing should be changed every seven days or sooner with the presence of old blood.
Your patient is admitted to the hospitalist/ medicine service and is ordered for an oral chemo regimen - what must be done prior to administering this medication?
a. For initial order verification or any change in dosage, two chemo-competent nurses are required to verify the signed order. (You may call 11R or 7F for assistance with this).
b. Confirm the patient has consent for administration of oral chemo.
What are some medications that require documentation of a reassessment?
PRN medications (including pain meds, sleeping meds, nausea meds, bowel meds, etc) & STAT/ 1x medications
Your patient has a PICC line, what must you assess prior to using?
a. correct order for line
b. X-ray confirmation of tip placement
c. “okay to use” order
d. What type of PICC – power? Non-power? Heparin dependent? Non-heparin dependent? Single lumen? Double lumen?
e. How does site look – is dressing c/d/i? Dressing change protocol followed?
This is a patient’s sacral area, how would you classify this wound?
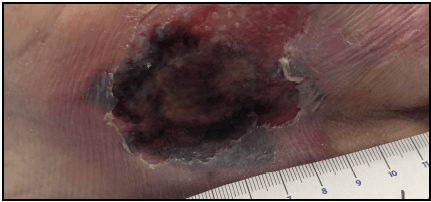
This is a DTI (deep tissue injury) with non-intact skin.
Your patient with a trach is ordered for a cat scan. What does this patient need to travel off the floor?
1. Patient must be accompanied by an RN
2. Portable suction and suction catheters
3. Continuous O2 sat monitoring off the floor