This image represents the normal histology of what structure/organ?
/main.jpg)
Gallbladder
(Note: mucosal layer is single layer of columnar cells; underneath is a single fibromuscular layer; underneath that is serosal fat layer with arteries, veins, nerves, and ganglia)
What zone would be injured histologically in the following circumstances?
(Example: Alcohol --> Zone 3)
a) Acetaminophen or other toxins
b) Vascular injury e.g. nutmeg liver
c) Metabolic abnormality e.g. NAFLD
d) Viral illness e.g. Hepatitis B or Autoimmune
a) Zone 3
b) Zone 3
c) Zone 3
d) Zone 1
A 67-year-old male with a history of Crohn's Disease prevents to the ED with severe, intermittent RUQ pain. His medical records are unavailable since he recently moved to the United States from Thailand. Labs in the ED reveal elevated serum WBC, elevated calcium, and normal lipid panel. Ultrasound reveals gallstones, and the patient is taken to the OR for cholecystectomy. What is the most likely appearance of his gallstones?
a) Yellow-brown, soft, and greasy
b) Dark brown, spiky, friable
c) Yellow-white, hard, faceted
d) Black, greasy, round
d) Dark brown, spiky, friable
These are likely pigment stones. (Factors: older age, elevated calcium, patient is from an Asian country where pigment stones are more common, no elevated lipids)
Why should you not give NSAIDs to a patient with early hepatorenal syndrome?
NSAIDs prohibit the formation of prostaglandins which would normally aid in vasodilation. Without vasodilation and continuous vasoconstriction of the renal arteries, the kidneys continue to fail --> late hepatorenal syndrome
A mildly elevated ALT and AST with AST > ALT by a factor of 2 implies what?
Alcoholic liver disease
A biopsy of patient A's gall bladder reveals:

Patient A is at risk of developing what pathological/clinical outcome?
Cholesterol gall stones
(Histology reveals lipid-laden foamy macrophages which implies cholesterolosis --> this often precipitates stone formation)
A patient presents to your clinic after returning from a vacation to Southeast Asia. He reports that he had unprotected intercourse while abroad, and he now is experiencing fever, weakness, joint pain, and nausea. On exam, the patient has some yellowing of the mucus membranes under his tongue. Histology is as following:

What is this finding called? What is the diagnosis?
Ground glass opacities -- Hep B
A mother brings her 8-year-old child to your clinic with concern of yellowing of the eyes and skin. Exam is positive for mild/moderate jaundice -- cardiac, respiratory, and neurological exams are all unremarkable. Labs reveal unconjugated hyperbilirubinemia and glucuronyl transferase activity at 9% of normal. What is the diagnosis?
a) Gilbert's Syndrome
b) Crigler-Najjar Type 1
c) Crigler-Najjar Type 2
d) Dubin-Johnson Syndrome
c) Crigler-Najjar Type 2
Why does effective circulatory blood volume drop in cirrhosis?
Hepatic and portal pressure increase as a result of intrahepatic fibrosis and narrowed sinusoids --> NO released from splanchnic and systemic circulation --> vasodilation --> cardiac output increases but not enough to compensate for dilated vessels throughout
Normal to mildly elevated ALT and AST with a major increase in Alk Phos suggests what kind of injury pattern?
Cholestatic injury
Assume that the aggregate of lymphoid cells is surrounding a bile duct. What is the diagnosis based on the following histology?

What is this lesion called?
Florid duct lesion associated with Primary Biliary Cholangitis -- immune attack on the bile duct marked by lymphocyte and plasma cell aggregation (may also see giant cells associated with granuloma formation)
Assume the following images are the same specimen stained with two different stains:

What is the likely error of inborn metabolism?
What gene is mutated in this condition?
What two organs may be affected?
Hereditary Hemochromatosis -- excessive absorption of iron
HFE gene
Liver and pancreas may be affected
A 28-year-old patient in her 36th week of pregnancy presents with sudden onset of fatigue, nausea, vomiting, and RUQ pain. She is admitted to the hospital and develops jaundice shortly admission. Her INR is 2.4, fibrinogen levels are decreased, and aminotransferases are moderately elevated. Liver biopsy reveals micro-vesicular fat deposits. What is her most likely diagnosis?
a) Pre-eclampsia
b) Acute Fatty Liver of Pregnancy
c) Intrahepatic Cholestasis of Pregnancy
d) Rotor's Syndrome
b) Acute Fatty Liver of Pregnancy
Why is someone on TPN at risk for gallstone formation? What are the three factors necessary for stone formation?
1) Super-saturated solution
2) Nidus
3) Stasis
Bilirubin present on a urine dip-stick may be the result of what underlying cause?
a) Crigler-Najjar Syndrome
b) Gilbert's Syndrome
c) Dubin-Johnson Syndrome
d) Hemolysis
c) Dubin-Johnson Syndrome
(conjugated bilirubin)
A 32-year-old male is seen in your clinic. Use the following histology and cholangiography to make a likely diagnosis:


Primary Sclerosing Cholangitis
(Histology: onion-skin periductal fibrosis with eventual obliteration of the bile ducts)
(Choliangography/ERCP: beads-on-a-string appearance from strictures in the bile ducts)
A patient with a history of chronic bronchitis presents to your clinic with shortness of breath, jaundice, and loss of appetite. Exam reveals pulmonary crackles and yellowing of the sclera. Liver biopsy reveals:

What is the diagnosis? What is the suspected mechanism explaining this histological finding?
Alpha 1 Antitrypsin Deficiency
Abnormal folding of A1AT molecules cause them to accumulate in the hepatocyte ER, and they cannot be secreted by the liver cell
A patient presents to your clinic post bone marrow transplantation with fever, abdominal distention, and RUQ pain. Exam is positive for RUQ tenderness, ascites, and hepatomegaly. No jaundice is visible on exam. Abdominal ultrasound most likely reveals:
a) Large collateral vessels and occlusion of the hepatic veins
b) Large stone obstructing the common bile duct
c) Gastric verices and occlusion of the portal vein
d) Nodular liver and dilated splenic vein
What is the diagnosis?
a) Large collaterals and occlusion of the hepatic vein
Budd-Chiari Syndrome
(Clues from stem: s/p bone marrow transplant; classic triad of hepatomegaly/ascites/RUQ pain; no jaundice)
Describe three factors that contribute to the formation of ascites and how they result in ascites
(Hint: The first one is decreased plasma albumin)
1) Decreased plasma albumin --> decreased osmotic pressure in vasculature --> favors fluid flow out into the tissues
2) Increased portal pressure and pressure in liver sinusoids --> increased hydrostatic pressure in vessels --> favors fluid flow out into the tissues
3) Increased aldosterone and ADH from RAAS system --> resorption of salt at distal tubule --> water retention
ALT and AST in the 1000s makes which of the following diagnoses most likely:
a) Hepatitis
b) Alcoholic cirrhosis
c) NAFLD
d) Acute Cholestasis of Pregnancy
a) Hepatitis
Levels that high point toward viral or toxic etiology
The following histological finding is called _____. It is hallmark in what etiology of liver disease? What causes this appearance?

Mallory Bodies
Hallmark of alcoholic liver disease
Injury to cytoskeletal intermediate filaments of hepatocytes -- intermediate filaments get broken down and clumped in the cytoplasm
Match the following histology with the malignancy:
a) 
b) 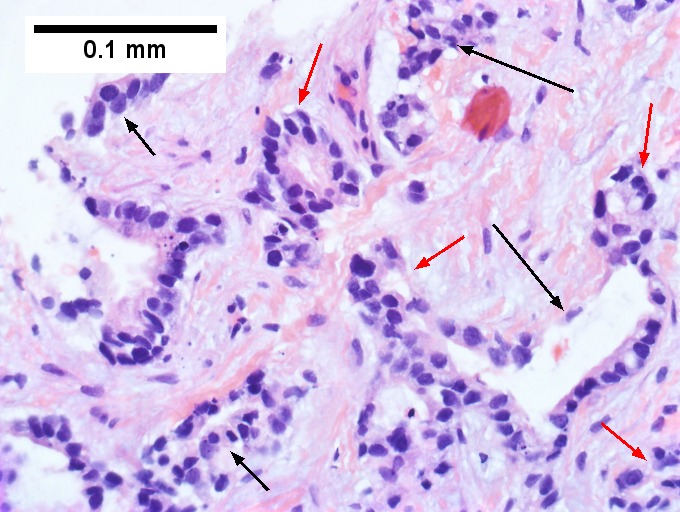
1) Cholangiocarcinoma
2) Hepatocellular Carcinoma
Explain the hallmarks of the histological findings associated with these cancers.
a) 2 (hepatocellular carcinoma) -- abnormally thickened plates of hepatocytes (thicker than standard 1-2 cells); loss of lobular structure; bile plugs
b) 1 (cholangiocarcinoma) --invasive glands and desmoplastic (fibrous) stroma
SAAG 1.8 and PMNs 276
What is the suspected diagnosis and appropriate next steps in management of this patient?
a) Sterile ascites --> start oral quinolone for prophylactic treatment
b) Peritoneal carcinomatosis --> refer to oncology
c) Bacterial peritonitis secondary to cirrhosis --> culture fluid and begin third-gen cephalosporin
d) Right heart failure --> refer to cardiology and begin beta blocker
c) SBP
Describe how the following circumstances increase the risk of hepatic encephalopathy:
1) Liver failure
2) Renal failure
1) The liver is responsible for converting ammonia to urea. If it fails, it cannot make this conversion and so serum ammonia rises. Shunts around the liver that develop during cirrhosis/liver failure also allows ammonia to circumvent the liver entirely and go to the brain.
2) The kidneys excrete urea that is delivered from the liver. If they are not filtering properly, urea can diffuse back into the intestine where it can be broken down into ammonia by intestinal bacteria --> increase in ammonia levels
Interpret the following Hep B serology:
HBsAG: Negative
Anti-HBc: Negative
Anti-HBs: Positive
Vaccinated - no acute infection
