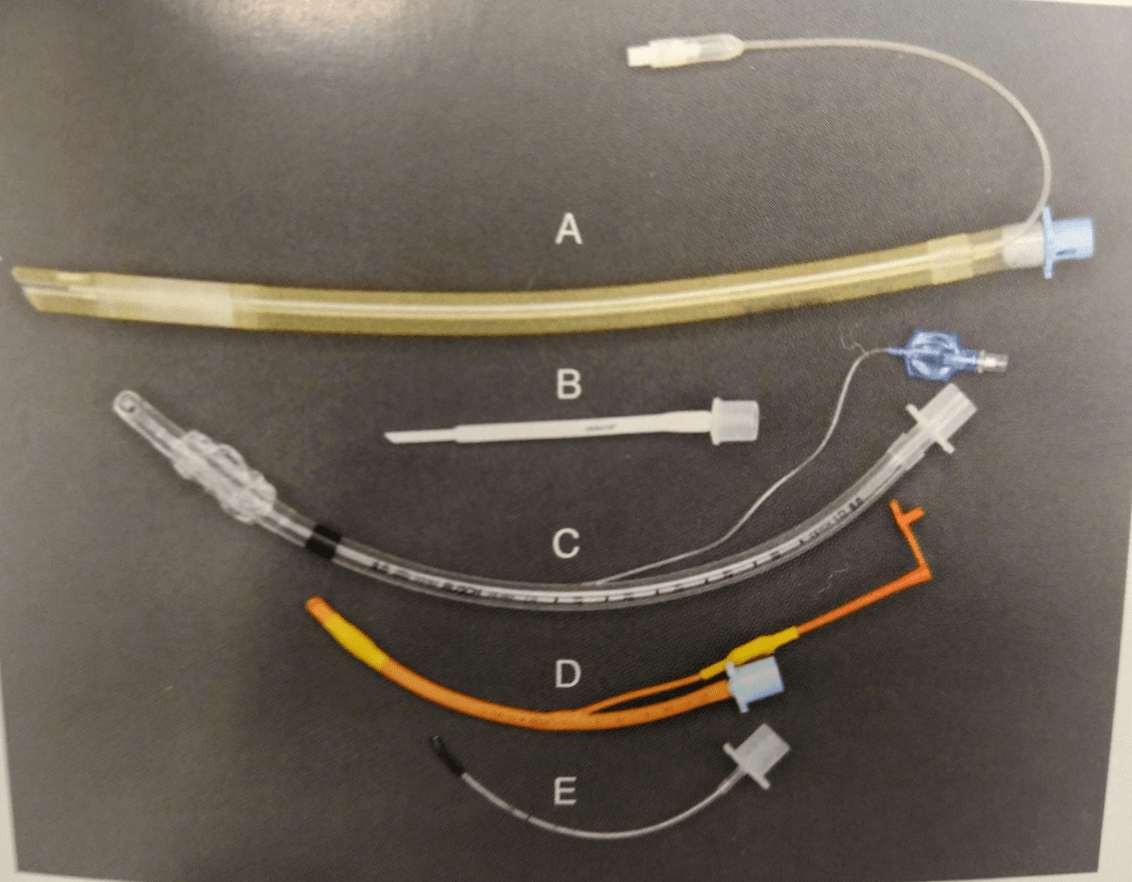
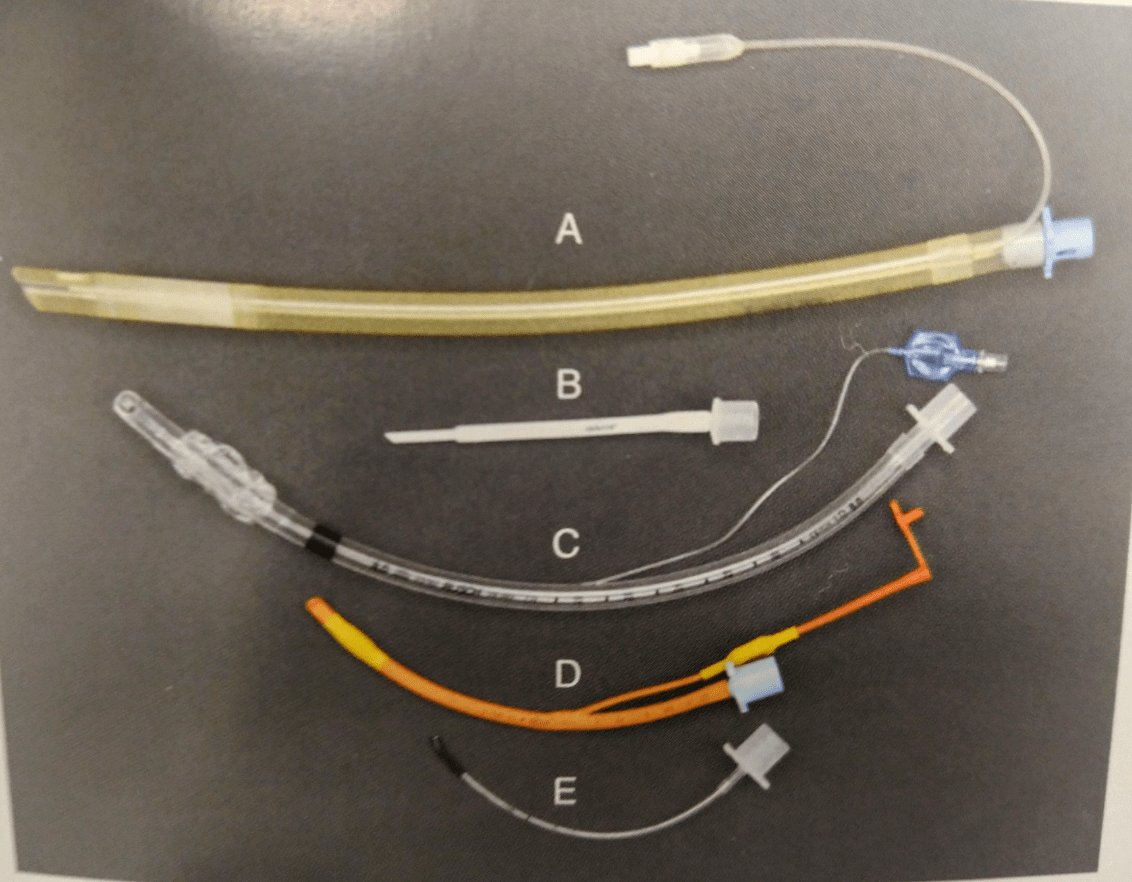
Endotracheal tubes are made out of three different types of material. Name one.
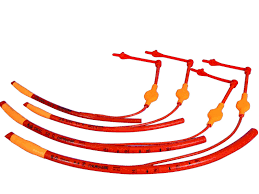
Silicone - flexible tubes, transparent
Red rubber - older style, most places do not use anymore
Polyvinyl chloride (PVC) - preformed curvature, sturdy, transparent
Name this part of the endotracheal tube.
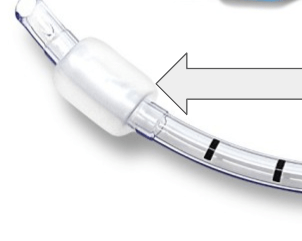
What is an endotracheal tube cuff?
A cuffed tube helps provide a sealed airway to reduce the risk of aspiration and waste anesthetic gas exposure.
Cuffed tubes can have either a high-volume, low-pressure cuff or a low-volume, high-pressure cuff.
A high-volume, low-pressure cuffed tube exerts a small amount of pressure over a wider area resulting in a reduced risk of tracheal mucosa damage.
A low-volume, high-pressure cuffed tube may cause more tracheal mucosa damage but allow a tighter seal.
You will need this piece of equipment for intubating. At least 3 size options should be prepared and available.
This helps deliver the anesthetic gases from the machine to the patient's lungs.
What is an endotracheal tube?
What position of the patient is optimal for intubation?
A. Dorsal
B. Sternal
C. Left lateral
D. Right lateral
What is
B. sternal recumbency?
Sternal recumbency provides optimal lung expansion and visualization of the trachea/glottis. This position aligns the oral, pharyngeal, and laryngeal axes.


In a CPR situation, most patients are intubated in lateral recumbency due to initiation of chest compressions. Delaying chest compressions is never ideal during CPR, only as a last resort should a patient be in sternal recumbency.
What are the landmarks for appropriately measuring an endotracheal tube?
What are the thoracic inlet to the incisor(s) or rostrum?
Ideally, you should pre-measure your endotracheal tube prior to any drug administration. This will help decrease the delay of providing oxygen support (if needed). This may not be feasible with fractious patients.
Name 1-2 disadvantages of a red rubber endotracheal tube.
Some disadvantages of red rubber endotracheal tubes include but are not limited to:
1) flammable - laser surgeries can cause overheating
2) harden over time causing cracks
3) not transparent (red coating) - "not see through"
4) potential latex allergies
5) greater risk of tracheal irritation
Name this part of the endotracheal tube.

What is a pilot balloon?
This connects to a cuff syringe via a one-way value. This provides a visual for monitoring cuff inflation.
A cuff syringe should not be attached/connected prior to extubation. This could lead to premature deflation of the cuff and the potential of a waste anesthetic gas leakage.
This intubation supply lubricates the endotracheal tube and helps create a seal.
What is sterile lube?

The murphy eye should never be occluded!

Be aware, this lubricant packet is not the same. It contains chlorhex solution and should not be used to lubricate the endotracheal tube.
Why is pre-oxygenation important for our patients?

Pre-oxygenation should be performed at least for 5 minutes prior to drug administration with a tight-fitting mask or with flow-by technique.
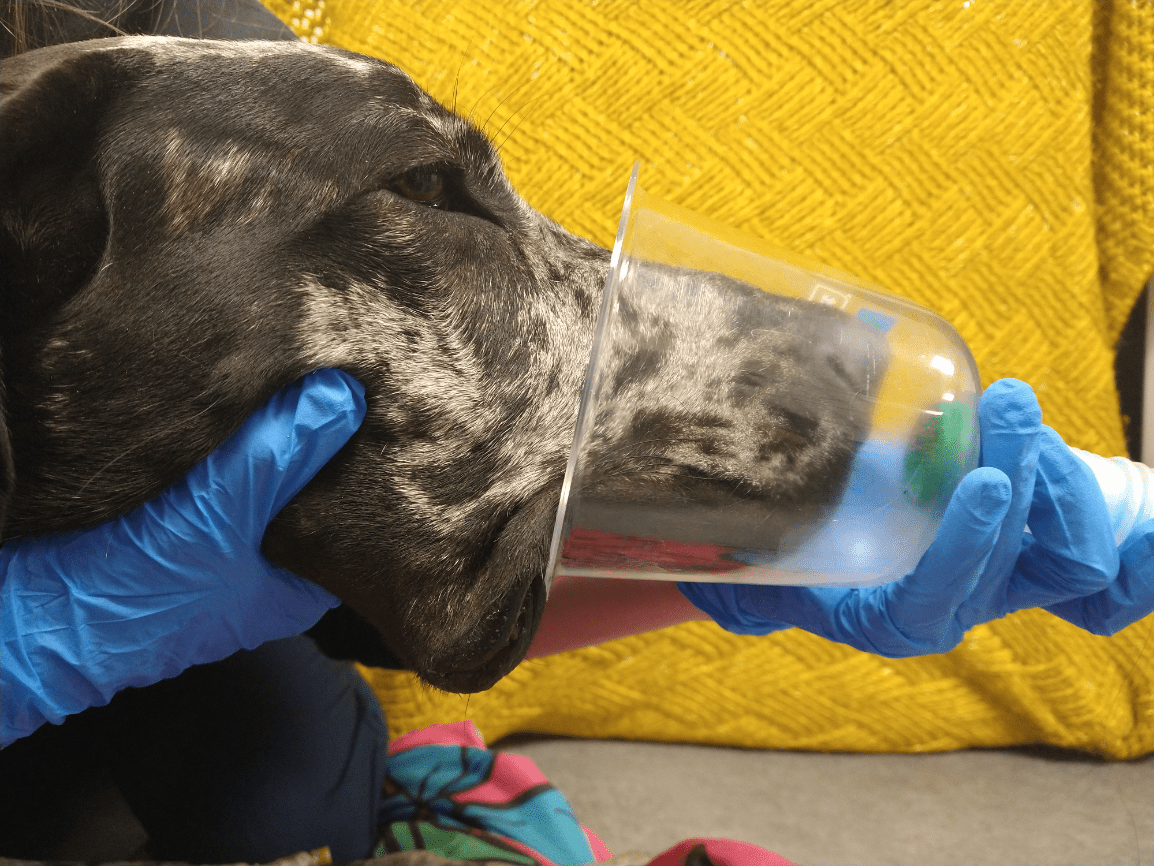
The goal of pre-oxygenation is to delay the onset of desaturation and hypoxemia should apnea occur during intubation. This is done by washing out the nitrogen within the functional residual capacity (FRC) of the lungs and temporarily "replacing" it with oxygen.

Please note proper flow-by technique includes having the tubing directly against the snout for effective preoxygenation.
Be mindful that some patients will not tolerate any pre-oxygenation methods. In these cases, it is better to avoid any potential injuries and/or increased stress.
When performing a leak test of an endotracheal tube cuff after intubation, at what pressure should you hold to?
A. 15 cm H2O
B. 20 cm H2O
C. 6 cm H2O
D. 30 cm H2O
What is
B. 20 cm H2O?
The proper technique for performing a leak test is to temporarily close the pop-off valve and squeeze the reservoir bag until the pressure manometer reads and holds at 20 cmH2O. At the same time, the person assisting with intubation, will listen for any air sounds near the mouth and inflate the cuff as necessary. A "whooshing" sound during inhalation which may indicate a leak. If the dial does not stay at 20 cm H2O, there is a leak. Do not rely solely on sound, air sounds can be heard during exhalation!
What type of endotracheal tube is designed to prevent kinking and has spiral wire coiled inside?
A. PVC tube
B. Silicone tube
C. Red rubber tube
D. Armored tube
What is
D. Armored?

Armored tubes while great to prevent any kinks (therefore, preventing air flow obstruction), there is a higher risk if a patient bites and breaks the tube.
What does the I. D. indicate on an endotracheal tube?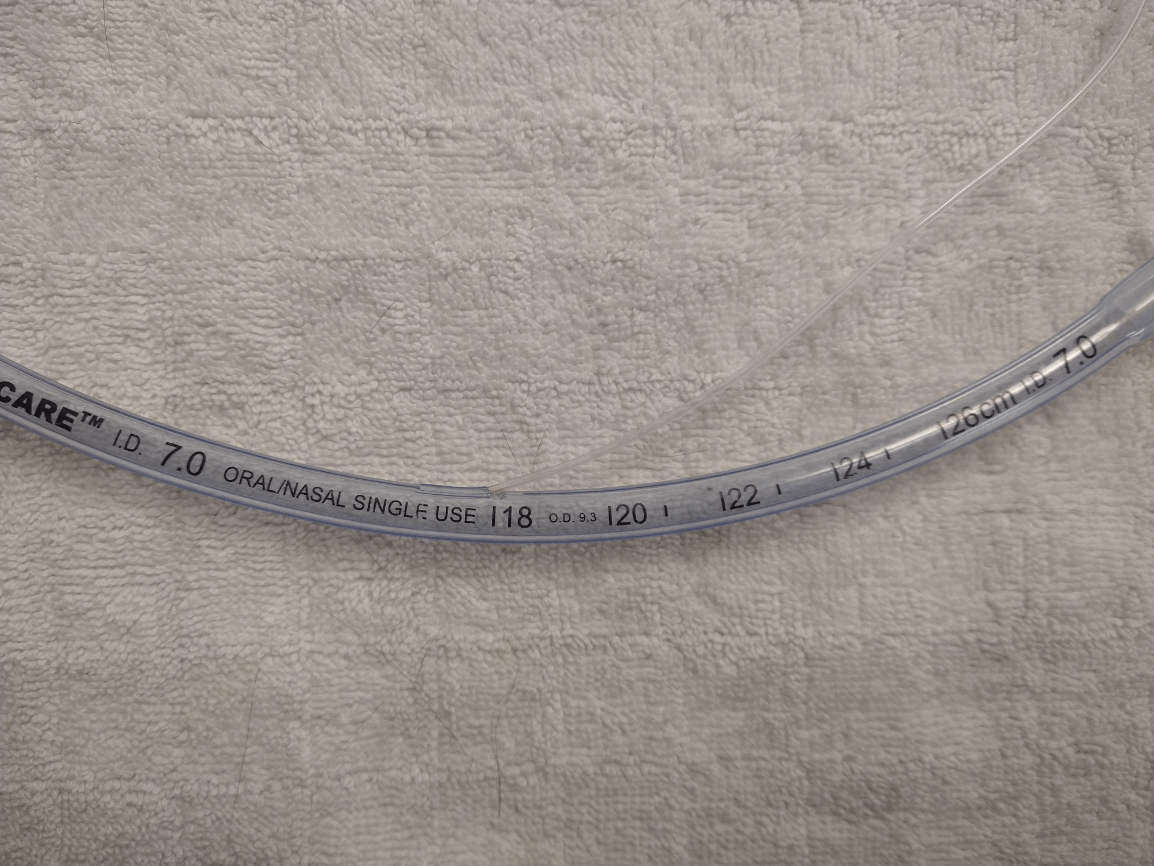
What is the internal diameter (in mm) of the endotracheal tube?
Typically, the ID number can be located near the mid-section and near the machine attachment end.
This specific endotracheal tube internal diameter is 7.0 mm.
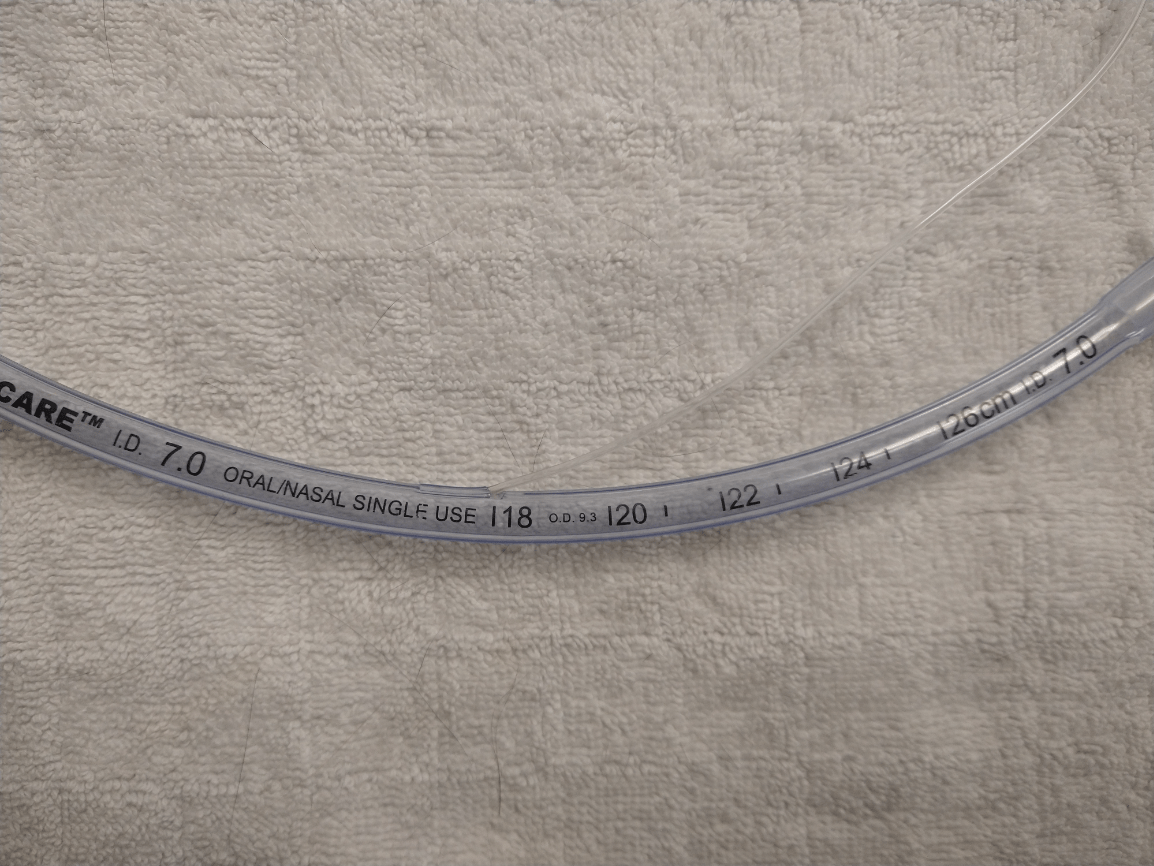
Some tubes, such as silicone tubes, be labelled differently. They are designed with an internal diameter measured in french (Fr). The size is still located at the machine attachment end.

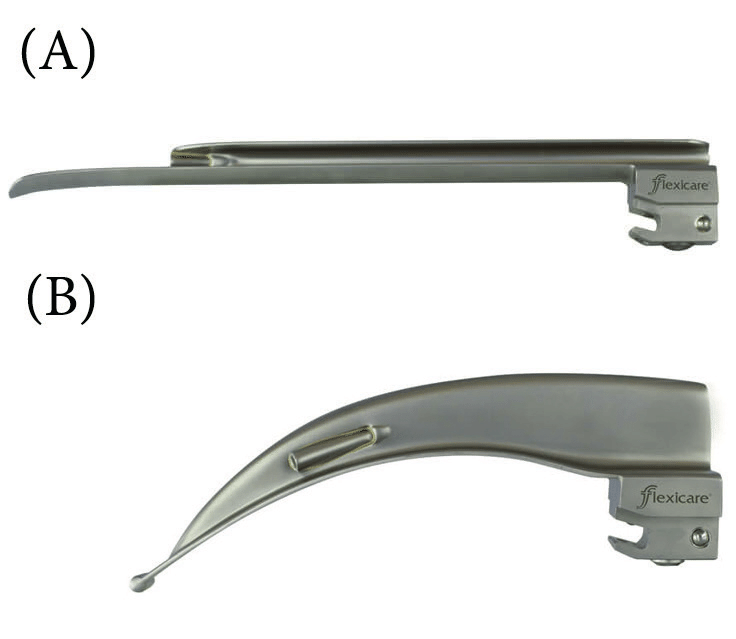
This piece of equipment helps increase the visibility of the larynx. Parts of this include a handle, a blade, and a light source.
What is a laryngoscope?

Laryngoscope blades come in various sizes (usually small, medium, and large). The Miller and Wisconsin blades are straight (A), while the Macintosh blades are curved (B). The handle should be held in your non-dominant hand, allowing better control of your endotracheal tube with your dominant hand.
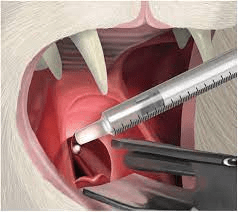
Placement of the laryngoscope should be ventral to the sensitive epiglottis to avoid causing any damage.
Directly after appropriate intubation has occurred, you notice your patient's tongue is turning a shade of a blue/purple color. What should be the next immediate step in the process?
A. Secure the endotracheal tube
B. Inflate the cuff
C. Attaching breathing circuit and provide positive pressure ventilation
D. Measure the endotracheal tube
What is
C. Attach the breathing circuit and provide positive pressure ventilation?
At this point your patient is desaturating and needs oxygen support. You should attach the machine end of the endotracheal tube to the breathing circuit and administer supplemental breaths.
This likely means that the endotracheal tube has not been secured and the cuff is not inflated yet. Be sure to keep the endotracheal tube in place to avoid an accidental extubation. Sometimes the weight of the breathing circuit could pull the endotracheal tube out of place.
Measuring the endotracheal tube for appropriate length (if pre-measurement was not performed prior), inflating the cuff balloon, and securing the endotracheal tube can be performed after the tongue returns to a normal pink color.
Lidocaine is applied topically to the larynx to decrease what?
What is laryngospasm?

Laryngospasm is a reflex where the larynx may "close" from intubation attempts. This can result in cyanosis and rapid respiratory depression leading to hypoxemia. Typically, 1 to 2 drop of topical lidocaine can help reduce laryngospasm.
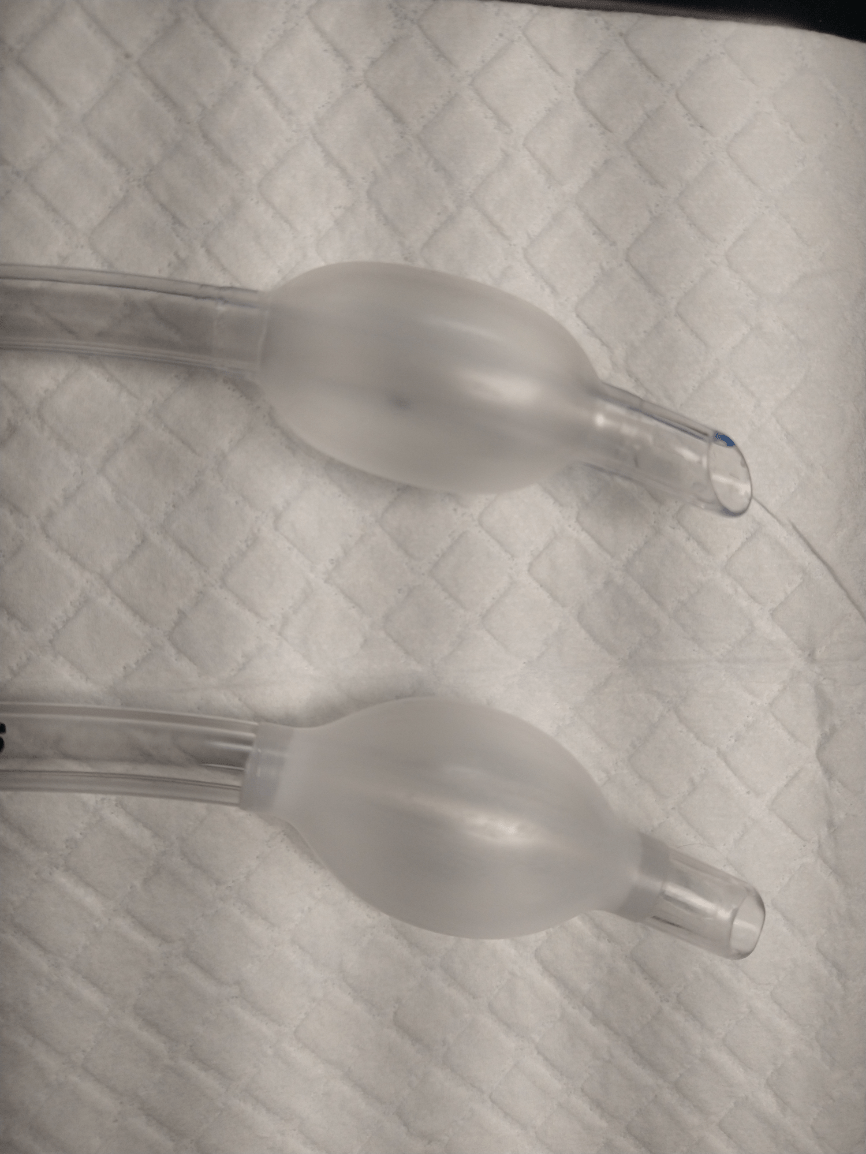
What is the difference between these endotracheal tubes?
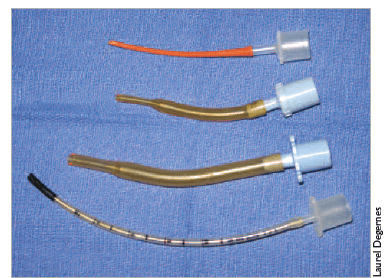
What are are non-cuffed or cuff-less endotracheal tubes?
Non-cuffed endotracheal tubes are used to prevent damage to the tracheal mucosa. Avian and reptile species have complete tracheal rings which could rupture with inflated cuffs.
Cuffed endotracheal tubes provide a better seal to avoid air leakage and reduce the risk of aspiration.
What do these numbers on an endotracheal tube indicate?
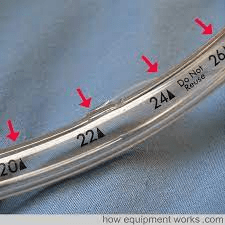
What are the length from the tip of an endotracheal tube (in cm)?
Silicone endotracheal tube lengths are not labelled with measurements.

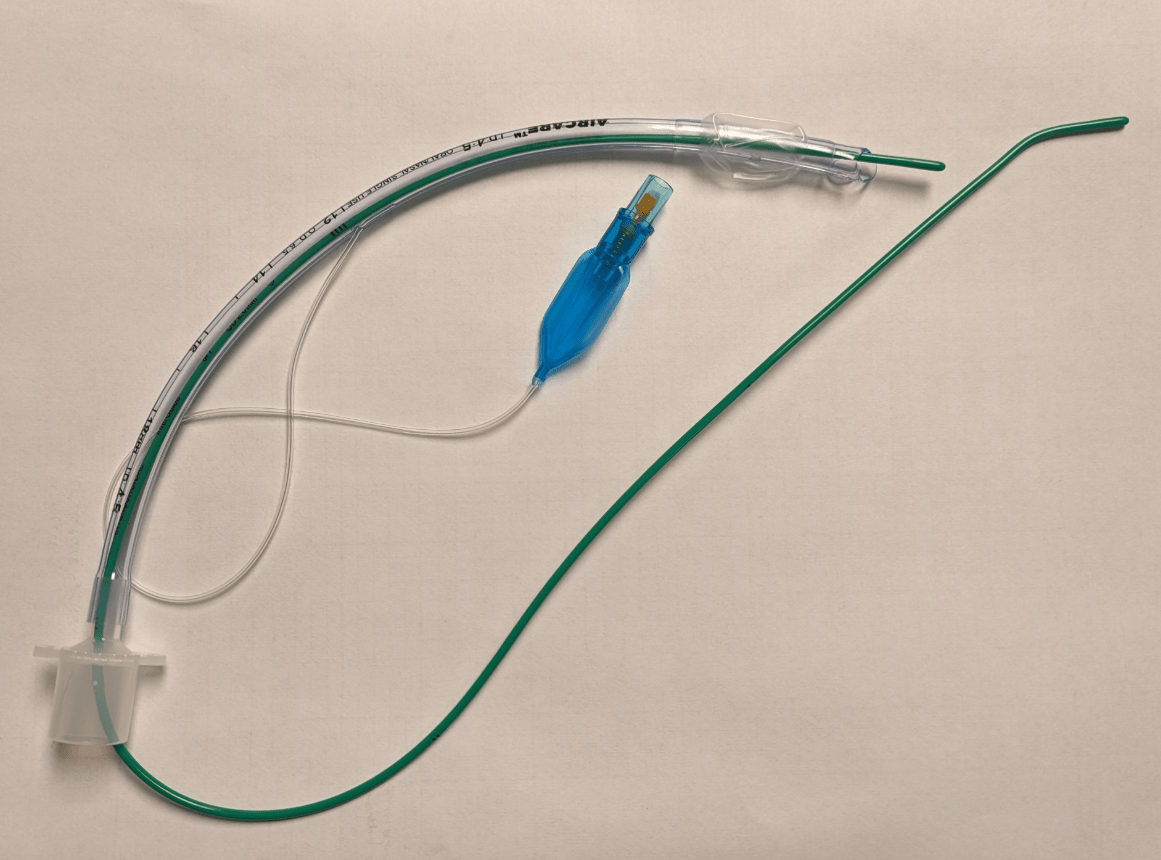
This equipment is used to help provide rigidity to endotracheal tubes that are flimsy and flexible.
What is a stylet?
Stylets are metal rods and should never extend past the beveled end of an endotracheal tube. This can cause damage to the trachea. Usually, stylets are used with silicone tubes.
A Which of the following are examples of areas to secure your endotracheal tube in place to avoid an accidental extubation?
A. behind the ears
B. over the muzzle/snout
C. under the jaw
D. all of the above
What is
D. all of the above?
Securing the tie behind the ears is ideal for patients with smaller or flatter faces (such as cats and brachycephalic breeds) .

Over the muzzle/snout can be ideal for longer nosed patients.

Tying under the jaw is ideal with specific procedures such as endoscopic, ophthalmologic, or involving the maxilla. 
Ensure the pilot balloon line and tongue are not tied in or occluded when securing the endotracheal tube in place.
True or False? One way to confirm tracheal intubation is to visualize a normal capnograph waveform.
What is TRUE?
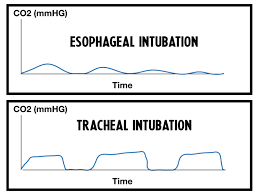
During esophageal intubation, a capnograph waveform will show little to no CO2 present. A normal capnograph waveform is present with correct tracheal intubation.
Name this device? 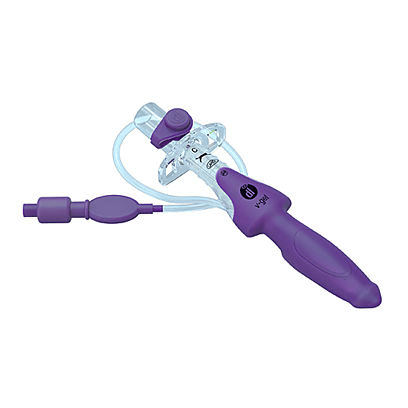
What is a V-gel?
V-gels are also known as a supraglottic airway device (supra- above, glottic- glottis = above the glottis).
This piece of equipment is an alternative form to provide an open airway for anesthetized patients (commonly used with rabbits/cats) by creating a seal around the larynx without invading the trachea. An advantage of this includes reduction of laryngospasm and decreased tracheal irritation.
Name this endotracheal tube part.
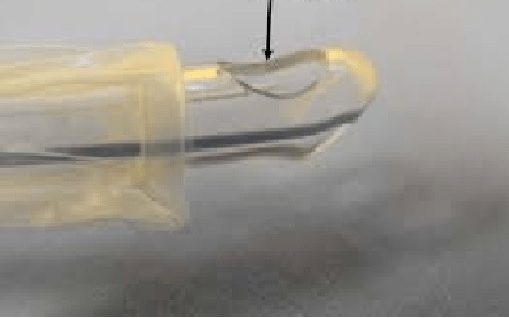
What is a murphy eye?
The murphy eye was designed to enable the passage of airflow should the beveled end of the tube ever becomes obstructed or blocked.
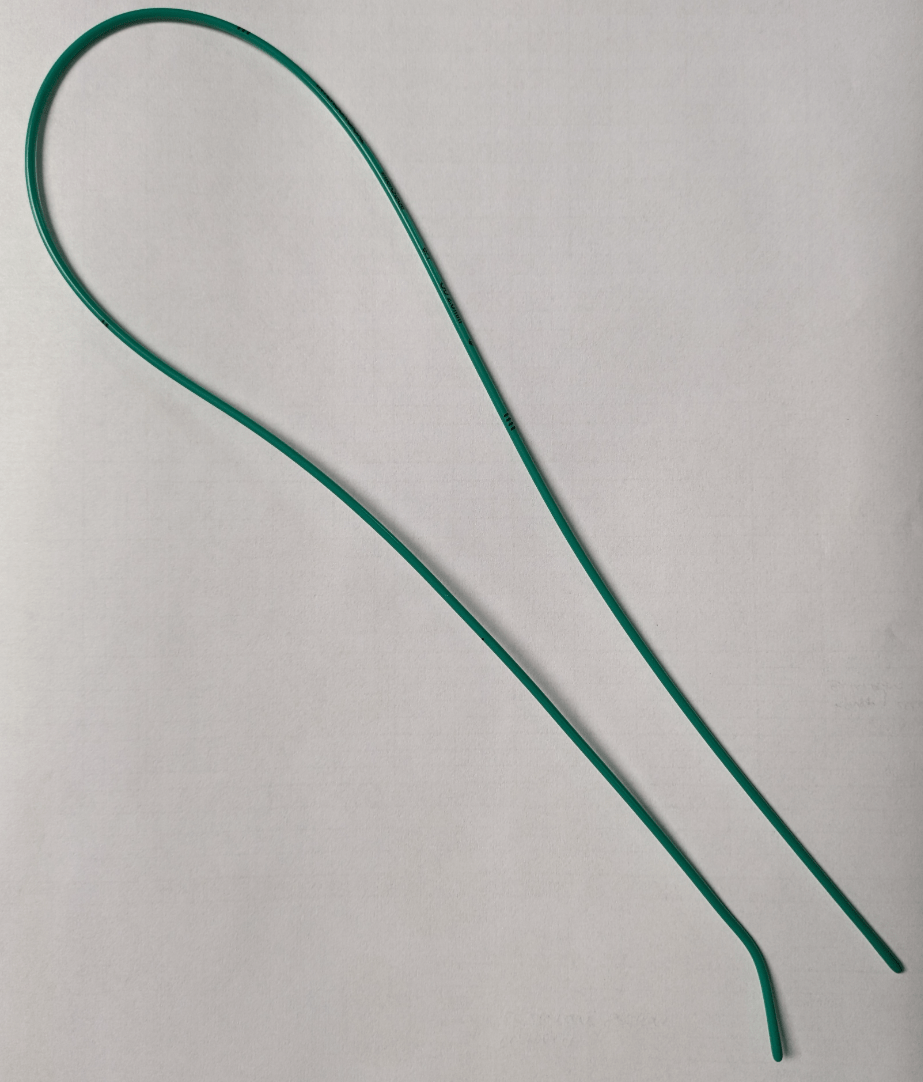
This flexible device is used to help facilitate difficult intubations by inserting directly into the trachea.
What is a bougie?


Look at these pictures. What is concerning with the hand placements?
What are fingers inside the mouth?


Avoid having your hands or fingers directly within the mouth. Even though these patients are losing consciousness, there is still the potential risk a patient could clamp down and cause some bodily injury.
True or False? Brachycephalic breeds (French bulldogs, Boston Terriers, Pugs, etc) can typically have smaller tracheal diameters. Therefore, smaller than "normal" endotracheal tube sizes are recommended for use.


What is TRUE?
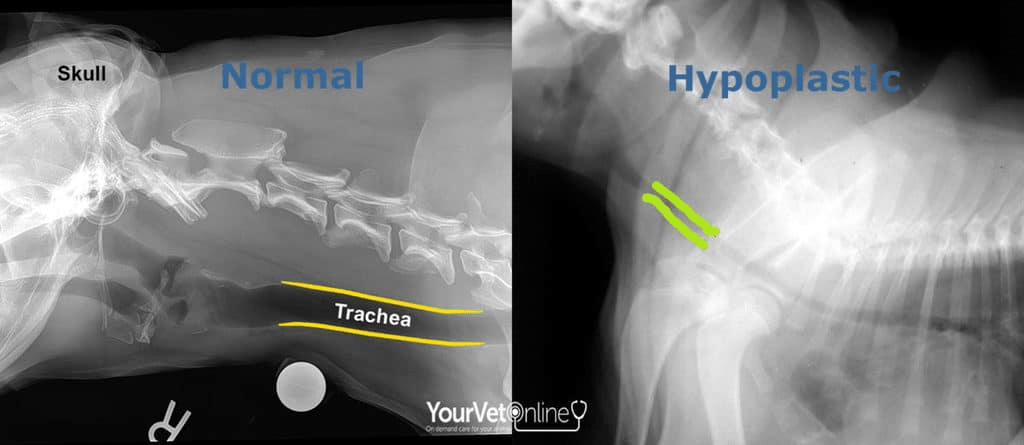
Brachycephalic breeds are commonly associated with brachycephalic airway syndrome (BAS). They are born with flatter faces and noses resulting with alterations of soft tissue structures which could affect their breathing by increasing airway resistance and increased effort during inhalation.
True or False? An endotracheal tube cuff is leak tested prior to intubation.
What is TRUE?
You should also leak test the cuff! This ensures a functional endotracheal tube before placement and prevents possibility of reintubating the patient. You do not have to add an abundance of air into the cuff. Only enough to visualize it holds air appropriately as needed.
Endotracheal tubes that have a defective cuff (does not hold air) should be discarded and replaced with a new tube.
While capnography is the gold standard for ensuring proper tracheal intubation, there are some other method for confirmation. Can you name any?
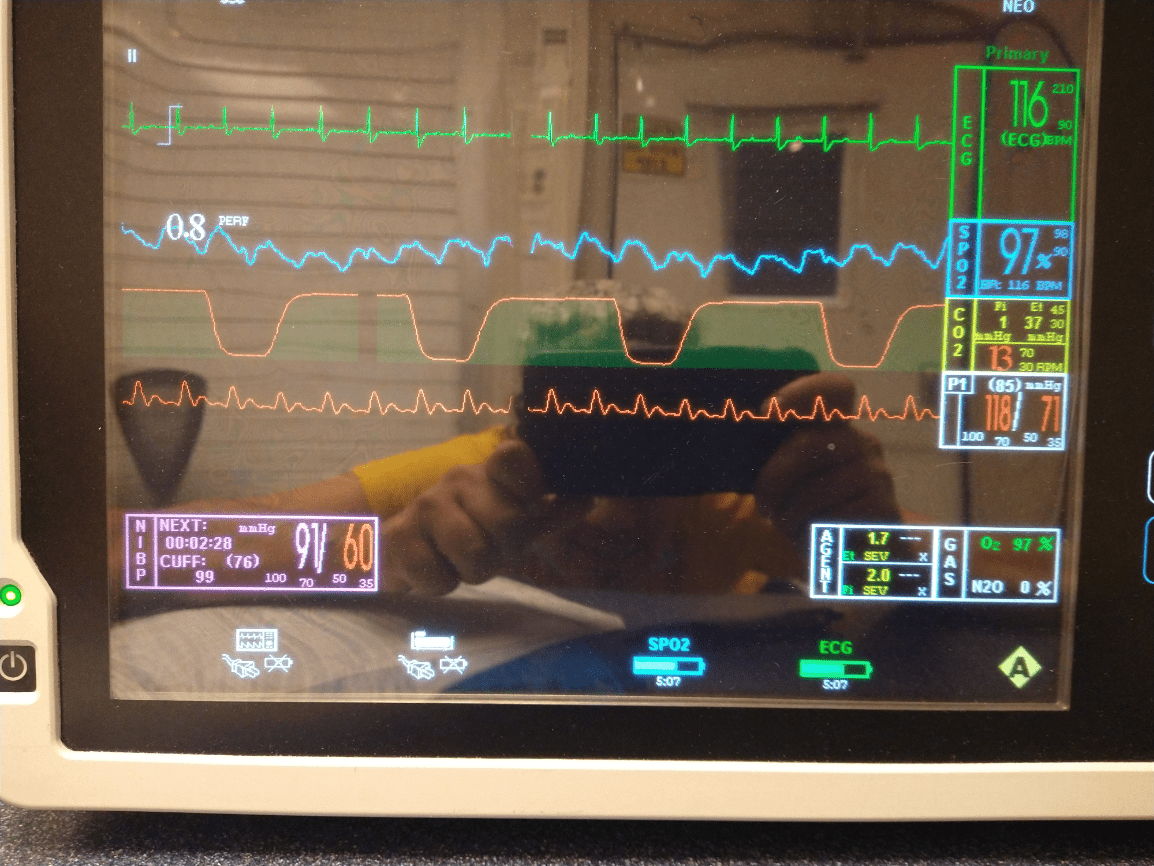
Capnography is the gold-standard way to confirm tracheal intubation. This provides monitoring of end-tidal CO2.
Other tips and tricks can include:
1) palpation of the trachea and endotracheal tube
2) detection of water vapor and/or air flow on a mirror or microscope slide
3) direct visualization
4) visualization of movement with the reservoir bag and patient's thorax
5) unidirectional valves will flutter upon inhalation and exhalation
6) visual condensation (could also mean esophageal intubation)
True or False? This button should be used to deliver a breath (positive pressure ventilation) to the patient WHILE attached to the breathing circuit.

What is FALSE?
The oxygen flush valve should NEVER be pressed when a patient is DIRECTLY attached to the anesthesia machine.
This button is located within the high pressure system and will result in barotrauma of the lungs.
Some ways to fill the reservoir bag are
1) detach the breathing circuit from the endotracheal tube and occluded the end. You may now press the O2 flush valve to adequately fill the reservoir bag. Keep in mind, this method requires the inhalant vaporizer to be turned off!
2) temporarily occluded the pop-off valve and increase the O2 flow rate for a short period until the reservoir bag fills.