What should ‘water egress’ training NOT include:
A. Hazards to aircraft and personnel during overwater
ops
B. Pre-ditching
C. Surface water survival and rescue water skills
D. How to remove all safety clothing in an emergency
D. How to remove clothing in an emergency
Water egress survival training should include: hazards to aircraft and personnel during overwater operations; pre-ditching, considerations and procedures; emergency ditching and evacuation procedures; upright emergency evacuation; emergency evacuation; surface water survival and rescue water skills. Fixed wing services that are required by FARs to carry emergency equipment, such as inflatable rafts, should provide this training.
Commission on Accreditation of Medical Transport System. 9th Edition
Accreditation Standards. Anderson: CAMTS. Pp. 04.02.01.
If a patient is to receive whole blood, which of the following is compatible with administration?
A. Dextrose 5% in water
B. Normal Saline
C. Ringer’s Lactate
D. Vasopressors
B. Normal saline
Normal saline is the fluid of choice for administering blood products. Dextrose 5% in water (D5W) causes hemolysis and Ringer’s Lactate will cause clotting. It is also not recommended to administer any vasoactive medications in the same IV line as blood products.
Pollak, A. (Ed.). Critical Care Transport. Sudbury: Jones and Bartlett. Pp. 294-295.
You respond to a high school baseball game for a 17- year-old male struck in the left chest by a wild pitch. He walked off the field and collapsed in the dugout. The patient is tachypneic and tachycardic with a decreased level of consciousness. Breath sounds are absent on the left side. You suspect:
A. A tension pneumothorax
B. A simple pneumothorax
C. A pulmonary contusion
D. A cardiac contusion
A. Tension pneumothorax
A clinical presentation of shock, respiratory distress, and decreased breath sounds are typical findings for a patient with a tension pneumothorax. A deviated trachea and jugular vein distension are late signs for a tension pneumothorax and are rarely seen in pre-hospital care. When a pneumothorax becomes large enough that cardiac output is compromised as a result of increased intrathoracic pressure, shock-like symptoms ensue.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 331-332.
While transporting a patient by rotor wing aircraft, you witness the patient’s ECG convert to ventricular fibrillation. Which of the following represents appropriate treatment?
A. 300 milligrams amiodarone IV
B. Immediate defibrillation
C. 1 milligram/kilogram lidocaine IV followed by
infusion
D. Initiate CPR until landing, then defibrillate
B. Immediate defibrillation.
Ventricular fibrillation occurs when there is chaotic depolarization from multiple areas of the ventricle. With this, there is no effective contraction of heart. It is the most common mechanism of cardiac arrest and can lead to sudden death if not converted to a normal rhythm. The best treatment for ventricular fibrillation is early defibrillation. Additional adjuncts to treating VF include CPR and pharmacologic therapy with epinephrine and vasopressin.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 412.
The normal fetal heart rate is:
A. 160-180 beats/min
B. 120-160 beats/min
C. 100-120 beats/min
D. 80-100 beats/min
B. 120-160 beats/min
The normal fetal heart rate baseline is usually between 110 to 160 beats per minute. Fetal heart rates tend to have periodic (due to contractions) and episodic (due to fetal movement) changes to rate. Baseline fetal heart rate should be assessed over a 10-minute period (in which at least two of those minutes must have no periodic or episodic changes), rounded to the nearest increment of 5.
Holleran, R. (ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 593.
Which of the following is the most important survival priority?
A. Finding or creating adequate shelter.
B. Finding adequate potable water.
C. Building an adequate fire.
D. Finding an adequate supply of food.
A. Finding or creating adequate shelter.
In a survival situation, the ‘Rule of Threes’ stipulates that the average person
can survive three minutes without oxygen, three hours without shelter in
extreme conditions, three days without water, and three weeks without food.
So once any safety and immediate medical concerns have been addressed, the next priority is to find or construct shelter from the environment. It should be big enough to protect all survivors, and as simple to construct as possible.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 128-129.
An appropriate RSI sequence of medications would be:
A. A Hypnotic followed by a depolarizing neuromuscular blocking agent.
B. A benzodiazepine followed by a narcotic analgesic.
C. A non-depolarizing neuromuscular blocking agent followed by a benzodiazepine.
D. A depolarizing neuromuscular blocking agent followed by a hypnotic and narcotic analgesic.
A. A Hypnotic followed by a depolarizing neuromuscular blocking agent.
Rapid Sequence Intubation (RSI) refers to the steps taken to induce anesthesia and safely intubate a patient while attempting to protect them from possible aspiration. It includes pre-oxygenation, administration of an induction agent to induce unconsciousness, use of cricoid pressure, administration of neuromuscular blocking agent and finally tracheal intubation. The only correct sequence is that of a hypnotic medication followed by a neuromuscular blocking agent. Here the choice includes a depolarizing neuromuscular blocking agent (succinylcholine is the only one). Other nondepolarizing neuromuscular blocking agents that can be used when succinylcholine is contraindicated (burns, crush injuries, underlying muscle diseases, renal failure) include pancuronium, atracurium, rocuronium, and vecuronium.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 214-213.
Pollak, A. (Ed.). Critical Care Transport. Sudbury: Jones and Bartlett. Pp. 168-171.
You are transporting a patient with a diagnosis of intractable seizures. The patient has been paralyzed and intubated. The flight crew will suspect continued seizures if:
A. Heart rate and BP acutely elevates
B. Pupils constrict
C. The patient becomes hyperthermic
D. You cannot assess for seizures after a paralytic is given
A. Heart rate and BP acutely elevates.
Intractable seizures are seizures that are difficult to control despite anticonvulsant therapy. When using paralytics to assist in the airway management of a patient with a diagnosis of intractable seizures, you should expect this problem to arise. Seizures cause autonomic changes that can produce tachycardia and blood pressure changes. Acute elevation of the heart rate and blood pressure can be either signs of continued seizure activity or the need for additional sedation. Administration of benzodiazepines work well in the management of either condition.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 394.
Which of the following signs and symptoms would you most likely see with a patient diagnosed with an acute inferior myocardial infarction?
A. Flash pulmonary edema
B. Tachycardia
C. Bundle branch block
D. Bradycardia and hypotension
D. Bradycardia and hypotension.
An acute inferior myocardial infarction is the result of occlusion of the right coronary artery. With this, symptoms of profound bradycardia (even complete heart block) and hypotension are likely. On exam, in addition to the hypotension, the patient may have distended neck veins and auscultate clear lungs. Due to the right ventricle being involved, patients are extremely volume sensitive as there is inadequate preload to the left ventricle. This type of infarction responds well to crystalloid infusion, atropine and possibly transcutaneous or transvenous pacing. Nitrates and Morphine cause a decrease in preload and are typically not recommended for patients with inferior infarcts.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 407.
What is the first sign of magnesium toxicity?
A. Decreased patellar reflexes
B. Episodic hypotension
C. Respiratory depression
D. Altered level of consciousness
A. Decreased patellar reflexes
Magnesium sulfate slows transmission of impulses at the neuromuscular junction by displacing calcium and interfering with nerve transmission to the muscles. When a therapeutic level of magnesium is achieved, a patient’s deep tendon reflexes are depressed, but not absent. A significant decrease in lower deep tendon reflexes may be the first sign of high serum magnesium levels leading to magnesium toxicity. Altered levels of consciousness and depression of the respiratory drive are late signs of magnesium toxicity but episodic hypotension can occur as a side effect of magnesium sulfate administration without magnesium toxicity. Initial treatment is to discontinue to magnesium sulfate immediately. If the patient has significant respiratory depression or compromise, the administration of calcium gluconate (1 gram of 10% solution over 3 minutes) to reverse the effects of magnesium should be considered.
Holleran, R. (ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 625-626.
You are dispatched to a reported MVC involving a semitanker truck. Upon arrival on scene you note an unknown substance leaking from the trailer. When parking your vehicle you should park:
A. Downwind, uphill
B. Downwind, downhill
C. Upwind, downhill
D. Upwind, uphill
D. Upwind uphill
Fumes from an overturned vehicle can be deadly. If the responder approaches from uphill and upwind, the possible contaminants in the air and on the ground will be moving away from the responder. Keep a close eye on changing conditions as winds and weather can change rapidly and put responding personnel and apparatus into the scene very quickly.
Pollak, A (Ed.). Emergency Care and Transportation of the Sick and Injured (9th ed.). Sudbury: Jones and Bartlett. Pp. 1037.
You are transporting a patient with an arterial line. How much pressure should the pressure bag be inflated to?
A. 200 mmHg
B. 250 mmHg
C. 300 mmHg
D. 350 mmHg
C. 300 mmHg
The pressure bag on an arterial catheter line should be inflated to 300mmHG, or above the blood pressure of the patient. The pressure bag should be check frequently to verify that it remains inflated to the proper pressure.
Pollak, A. (Ed.). Critical Care Transport. Sudbury: Jones and Bartlett. Pp. 584.
You respond to for a 25-year-old pedestrian struck by a vehicle moving at approximately 35 mph. She is persistently hypotensive with a blood pressure of 70/50 and pulse rate of 130. She is alert, orientated and conversing normally. Airway is clear and examination of the chest is normal. Her abdomen is obviously distended and pelvis is very unstable to clinical examination. Advanced therapy would best be accomplished by:
A. Establish IV access and rapidly infuse of 2 - 3 liters of crystalloid.
B. Establish IV access and fluid bolus patient with 1 liter of crystalloid.
C. Establish IV access, stabilize the pelvis, and initiate fluid resuscitation.
D. Establish saline lock IV access, stabilize the pelvis, and supplemental oxygen.
C. Establish IV access, stabilize the pelvis, and initiate fluid resuscitation. A significant arterial injury can occur in patients with a pelvic fracture. A major pelvic fracture has occurred when a patient has fractures in two separate places in the pelvic structure. Other complications from major pelvic injuries include damage to the lower abdominal organs. Fluid resuscitation and control of bleeding is a priority, and is accomplished with the use of pelvic stabilizing device.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 364.
Which burn area of a patient would be most concerning during the initial evaluation?
A. Fingers
B. Feet
C. Arms
D. Face
D. Face
Burns to the face are serious, and should be evaluated with a high index of suspicion for potential inhalation injury or injury to the eyes (especially in chemical burns). While burn injuries to the hands or feet can result in longterm disability, and requires treatment at a burn center, they are rarely life threatening on their own.
Bledsoe, B. (Ed.). Critical Care Paramedic. Upper Saddle River: Pearson. Pp. 509.
The most common cause of non-traumatic cardiac arrest in
children is
A. Dysrhythmias
B. Post-surgical complications
C. Undetected cardiac lesion
D. Respiratory Failure
D. Respiratory Failure
The most common cause of cardiac arrest in the non-trauma pediatric patient is related to inadequate oxygenation and ventilation. Respiratory failure is characterized as inadequate gas exchange, and untreated respiratory failure will lead to cardiovascular collapse as pediatric patients have limited compensatory mechanisms.
Pollak, A., M.D. (ed.). Critical Care Transport. Sudbury: Jones and Bartlett. Pp. 928, 943.
Holleran, R. (ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 663.
During international transports, if medical crewmembers exit the aircraft in a foreign country, they should:
A. Contact the embassy of their home country.
B. Utilize local handlers to act as interpreters.
C. Secure and leave controlled substances in the aircraft.
D. Behave and dress to blend in with the locals.
C. Secure and leave controlled substances in the aircraft.
International law prohibits bringing controlled substances onto foreign soil, they must be secured and kept in the aircraft. Although the use of local resources or handlers is recommended, it is not required. Contacting the embassy of the program’s home country may be beneficial if an extended stay, such as a rest period, is needed; but there is no requirement to do so. Dressing and behaving in a manner to blend in with the locals is an example of exceeding compliance and is not required.
Commission on Accreditation of Medical Transport System. 9th Edition Accreditation Standards. Anderson: CAMTS. Pp. 04.03.06.
Which of the following is not an absolute contraindication for the use of Succinylcholine?
A. Critical burns 72 hours ago
B. Upper airway obstruction
C. History of myasthenia gravis
D. History of anesthesia induced fever
B. Upper airway obstruction
Absolute contraindications for the use of Succinylcholine include disorders with a potential developing hyperkalemia which include: upper or lower motor neuron defects; prolonged chemical denervation (muscle relaxants, magnesium, clostridial toxins); direct muscle trauma (crush injuries); thermal injuries (critical burns); tumor or inflammation; acute or chronic renal failure.
Additionally, Succinylcholine is known to be a trigger for inducing malignant hyperthermia.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 215-217.
A 25-year-old male was brought into the emergency department with a suspected head injury. The patient was riding his bicycle when a motorist opened a vehicles door into his path. The patient was observed to strike the edge of the door with the side of his face, and was forcibly ejected from the bicycle, traveling a distance of 10 feet (3 meters) where he impacted the ground. He was observed by bystanders to lie motionless on the ground for approximately 30-45 seconds, then rose to his feet and began to walk around the scene. Upon arrival at the Emergency Department, the patient’s vital signs were heart rate 110, respirations 20, blood pressure 130/70, pupils equal and reactive, and mental status alert / oriented to person, place, and time. An emergent CT without contrast was completed. Approximately 45 minutes later, the patient became less responsive, was not following commands, and left side weakness had developed. What is the most likely cause of the above patient’s deterioration?
A. Subdural hemorrhage
B. Epidural hemorrhage
C. Subarachnoid hemorrhage
D. Intracerebral hemorrhage
B. Epidural Hemorrhage
This Scenario supports the diagnosis of an epidural hemorrhage. Although only seen in one third of cases, the classic presentation of epidural bleeding involves a transient loss of consciousness, a recovery to a normal neurologic state or lucid period (that can last for hours), and finally a decline in level of consciousness. Other symptoms include headache, contralateral weakness of extremities, ipsilateral pupillary changes, complete loss of pupillary reflex, bradycardia and death. Epidural bleeds usually result from the tearing of the middle meningeal artery. This arterial bleeding causes an onset of symptoms within the first few hours following the injury.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 313.
The end tidal CO2 waveform below may indicate:

A. Esophageal intubation
B. Cuff deflation
C. An obstructed exhalation valve
D. Auto-PEEP
B. Cuff deflation
This waveform is representative of an inadequate seal around the endotracheal tube. This results in a blunted or rounded plateau that may blend into the downward slope. Possible causes of an inadequate seal are a leaky or deflated endotracheal cuff, or an endotracheal tube that is too small for the patient.
CareFusion. Capnography Handbook. Carefusion: Yorba Linda. 2010. Pp. 32.
Increased intra-thoracic pressure secondary to overzealous bag-mask ventilation contributes to an increased:
A. Cardiac output
B. Pulmonary vascular resistance
C. Cerebral perfusion pressure
D. Intracellular potassium
B. Pulmonary vascular resistance
Over-ventilation is a common problem during resuscitative efforts, and results in increased intrathoracic pressure. This increased intrathroacic pressure is significant in pediatric patients, and will decrease cardiac output, decrease venous return, increase pulmonary vascular resistance, and increase the chances of barotrauma.
Mejía, R., Fields, A., Greenwald, B., & Stein F. (Eds.). Pediatric Fundamental Critical Care Support. Mt. Prospect: Society of Critical Care Medicine. Pp. 3-4.
The build-up of metabolites that stimulate nerve endings as a result of an imbalance between myocardial oxygen supply and demand is best described as:
A. Angina pectoris
B. Acute myocardial infarction
C. Transient ischemic attack
D. Coronary artery disease
A. Angina pectoris
Angina is a symptom of coronary artery disease. It occurs when there is an imbalance between the supply of and demand for oxygen in the myocardium. This results in the cardiac muscle becoming ischemic and switching to anaerobic metabolism. There is a buildup of metabolites which then activates nerve endings and results in anginal pain.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 401-402.
Pollak, A. (Ed.). Critical Care Transport. Sudbury: Jones and Bartlett. Pp. 511-512.
The most reliable indicator that a burn patient is being under-resuscitated with fluids is:
A. Increased hemoglobin and hematocrit
B. Oliguria
C. Tachycardia
D. Hypotension
B. Oliguria
Oliguria or low urine output is the most reliable indicator that a burn patient is not getting enough fluids. The goal of fluid resuscitation is to maintain perfusion of vital organs. The goal for urinary output in adults is 30-50 milliliters/hour and 1.0-1.5 milliliters/kilogram/hour in pediatrics.
Holleran, R. (Ed.). ASTNA Patient Transport: Principles and Practice (4th ed.). St. Louis: Elsevier. Pp. 381.
You have been requested to a rural hospital to transport a patient that was in a motor vehicle accident 24 hours ago and the patient refused transport at the scene. The patient came to the emergency department today with increasing difficulty breathing. When you arrive, the patient is in obvious respiratory distress and has the following vital signs: heart rate 110, blood pressure 88/56, respirations 26, SpO2 90% on 15 liters per minute oxygen via non-rebreather mask, side stream ETCO2 49. You auscultate the patient’s lungs to find diminished lung sounds bilaterally with rhonchi present. You should suspect what injury?
A. Tension pneumothorax
B. Diaphragmatic rupture
C. Pulmonary contusion
D. Tracheobronchial injury
C. Pulmonary contusion
Pulmonary contusions occur as a result of blunt trauma to the chest. Intralveolar bleeding occurs as a result of the blunt injury to the lung tissue when the alveolar-capillary integrity is damaged. The result is intersistal bleeding and edema, leading to decreased lung compliance and hypoxia. Pulmonary contusions develop slowly, and may take 12-48 hours (or longer) for symptoms specific to the pulmonary contusion to develop (sometimes initial discomfort or dyspnea may be obscured by skeletal/muscle soreness from the blunt trauma).
During transport, the displayed end tidal CO2 waveform changed to what is shown below. This end tidal CO2 waveform may indicate:
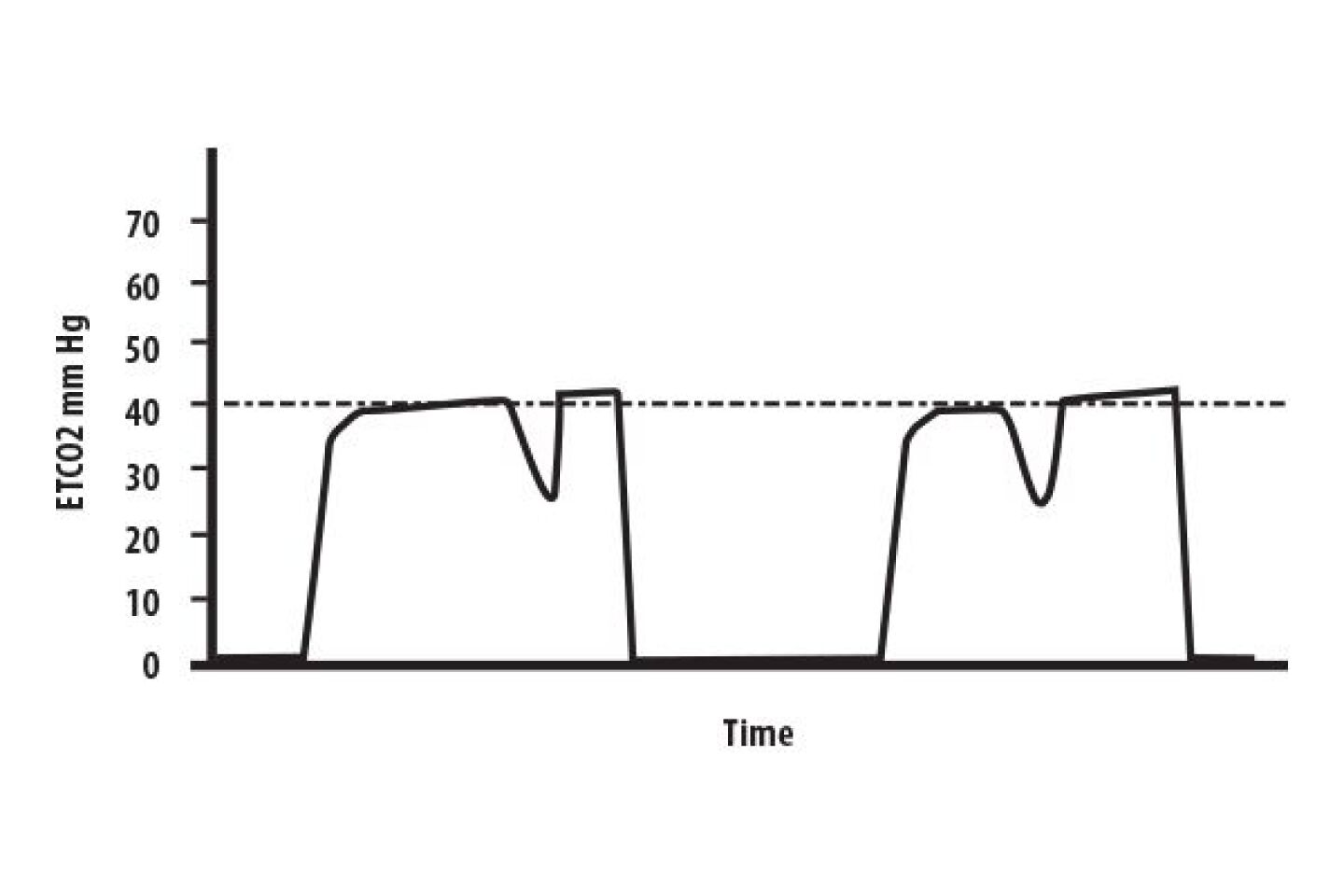
A. The ventilator tubing is leaking
B. The ETT cuff is leaking
C. There is an obstruction in the exhalation tubing
D. There is inadequate sedation
D. There is inadequate sedation.
The tracing on the waveform shows a cleft in the plateau portion. This waveform, called a curare cleft, signifies decreased sedation and/or paralytics as the patient is taking small spontaneous breaths. The cleft’s depth is inversely proportional to the degree of sedation / paralytic agent effect, but may not occur with each breath. The presence of curare cleft waveform may be the first indicator of loss of effective sedation.
CareFusion. Capnography Handbook. Carefusion: Yorba Linda. 2010. P. 28, 30.
Appropriate pharmacological management of the premature infant with respiratory distress may include:
A. PRBC Transfusion
B. Exogenous surfactant
C. Theophylline
D. Dexamethasone
B. Exogenous surfactant
Neonatal Respiratory Distress Syndrome (aka Hyaline membrane disease) primarily affects the lungs of premature infants and causes significant difficulty in breathing. This disorder is rarely seen in full term infants. The cause is lack of pulmonary surfactant in the alveoli. Surfactant is a mixture of proteins and phospholipids that reduce the surface tension within the alveoli and keep the alveoli from collapsing. Administration of surfactant is part of the long-term management of neonatal respiratory distress syndrome. For transport, focus is mainly on assessment and management of the ABCs including administration of a high concentration of oxygen with ventilatory support.
Bledsoe, B. (Ed.). Critical Care Paramedic. Upper Saddle River: Pearson. Pp. 882-884.