Which nursing intervention would help an older adult experiencing urinary incontinence? Select all that apply. One, some, or all responses may be correct.
A. Provide nutritional support.
B. Provide voiding opportunities.
C. Avoid indwelling catheterization.
D. Provide beverages and snacks frequently.
E. Promote measures to prevent skin breakdown.
B, C, & E
An older adult should be provided voiding opportunities to minimize urinary incontinence. Indwelling catheterization should be avoided because this action increases the risk of infection, weakens bladder tone, and may cause discomfort. Measures to prevent skin breakdown should be taken because the client may develop skin problems due to incontinence. Nutritional support and frequent beverages and snacks should be provided to a client with malnutrition.
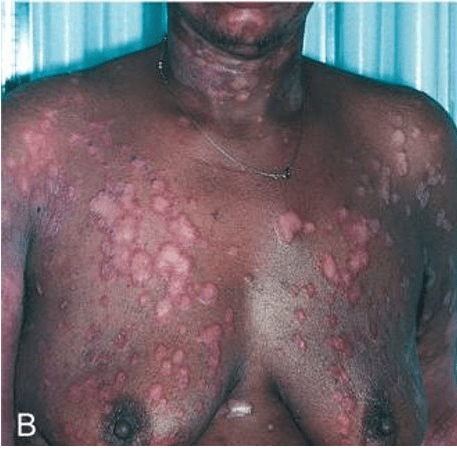
The nurse is assessing a client who presents with multiple raised, erythematous plaques on the chest and upper body as shown in the image. Based on the image, which skin disorder does the nurse suspect?
A. Atopic dermatitis
B. Chronic plaque psoriasis
C. Tinea corporis
D. Seborrheic dermatitis
Correct Answer:
B. Chronic plaque psoriasis
Rationale:
Chronic plaque psoriasis presents as well-demarcated, erythematous plaques with silvery scales, often chronic and recurrent. Common therapies include topical corticosteroids and vitamin D analogs for mild disease, with phototherapy or systemic/biologic agents
Atopic dermatitis is typically associated with pruritus, erythema, and lichenification, especially in flexural areas.
Tinea corporis (ringworm) appears as annular lesions with central clearing and raised borders.
Seborrheic dermatitis causes greasy, yellow scales, usually on the scalp, face, and chest.
The nurse is providing education to a group of nursing students about the causes of pressure injuries. Which factors directly contribute to the development of pressure injuries? (Select all that apply.)
A. Prolonged pressure over a bony prominence
B. Friction between the skin and bed linens
C. Exposure to moisture from incontinence or perspiration
D. Shearing forces when the client slides down in bed
E. High dietary sodium intake
Correct Answers:
A, B, C, D
Rationale:
Pressure: Prolonged, unrelieved pressure decreases blood flow and oxygen delivery, leading to tissue ischemia.
Friction: Skin rubbing against surfaces (linens, clothing) damages the epidermis, increasing risk.
Moisture: Incontinence, sweat, or wound drainage causes maceration, weakening skin integrity.
Shear: When the skin stays in place but underlying tissues move (e.g., sliding in bed), blood vessels stretch and tear, impairing circulation.
High sodium intake: Does not directly cause pressure injuries. It may affect fluid balance, but it is not a recognized direct risk factor.
Which type of burn injury should be followed up by scheduling the client for an electrocardiogram (ECG)?
A. Flame burn
B. Chemical burn
C. Electrical burn
d. Radiation burn
In an electrical burn injury, changes in the ECG may indicate damage to the heart. In flame burn injuries, the smoldering clothing and all metal objects are removed. If a client suffers from chemical burns, the dried chemicals present on skin should not be made wet but should be brushed off. If the client has radiation burn injuries, then the source should be removed using tongs or lead protective gloves.
Which interventions would be used as first aid for a client who has burn injuries from an electrical current until the client is transferred to a health care facility? Select all that apply. One, some, or all responses may be correct.
A. Cover the burns with ice.
B. Leave the adherent clothing in place.
C. Wrap the client in a dry, clean sheet.
D. Remove as much burned clothing as possible.
E. Immerse the burned body part in cool water.
When a client is injured by an electrical current, the adherent clothing should be left in place until the client is transferred to a primary health care center. Wrapping the client in a clean, dry sheet may prevent further contamination of the wound and also provide warmth. Removing as much burned clothing as possible prevents further tissue damage.
The burns should not be covered with ice because this may cause hypothermia and vasoconstriction of blood vessels. Do not immerse the burned body part in cool water because it may cause extensive heat loss.
Which expected sensory loss associated with aging would a nurse recall when designing a plan of care for an 85-year-old client admitted to a nursing home? Select all that apply. One, some, or all responses may be correct.
A. Difficulty in swallowing
B. Diminished sensation of pain
C. Heightened response to stimuli
D. Impaired hearing of high frequency sounds
E. Increased ability to tolerate environmental heat
B& D: Diminished pain and impaired hearing.
Because of aging of the nervous system, an older adult has a diminished sensation of pain and may be unaware of a serious illness, thermal extremes, or excessive pressure. As people age, they experience atrophy of the organ of Corti and cochlear neurons, loss of the sensory hair cells, and degeneration of the stria vascularis, which affects an older person’s ability to perceive high-frequency sounds. An interference with swallowing is a motor loss, not a sensory loss, and it is not an expected response to aging. There is a decreased, not heightened, response to stimuli in older adults. There is a decreased, not increased, ability to physiologically adjust to extremes in environmental temperature.
The nurse is reviewing images of common dermatologic conditions with a group of nursing students. One image shows erythematous, inflamed patches of skin with vesicles, scaling, and lichenification on the flexor surfaces of the elbows. The nurse asks the students to identify the condition.

A. Eczematous dermatitis
B. Psoriasis vulgaris
C. Tinea corporis (ringworm)
D. Seborrheic dermatitis
Answer: Eczematous dermatitis (atopic dermatitis): Pruritic, erythematous lesions often on flexor areas, with vesicles, scaling, and thickened skin due to chronic scratching.
Psoriasis: Well-demarcated plaques with silvery-white scales, often on extensor surfaces.
Tinea corporis: Annular “ring-like” lesions with central clearing.
Seborrheic dermatitis: Greasy, yellow scales, typically on scalp and nasolabial folds.
The nurse is assessing a client’s skin over the pelvis and notes an extremely reddened patch above the hip line. The area is intact, with no open skin, but remains red and does not blanch when pressed. How should the nurse stage this pressure injury?
A. Stage 1
B. Stage 2
C. Stage 3
D. Stage 4

A. Stage 1
Stage 1: Non-blanchable erythema of intact skin. Stage 2: Partial-thickness skin loss involving epidermis/dermis (abrasion, blister, or shallow crater). Stage 3: Full-thickness tissue loss with visible subcutaneous fat but not bone/tendon/muscle. Stage 4: Full-thickness tissue loss with exposed bone, tendon, or muscle.
An 85 year old client sustained burns of the extremities in a house fire. During assessment, which clinical finding would be of concern to the nurse?
A. Increased temperature
B. Increasing activity level
C. Burns around the mouth
D. Edema distal to the burns
Burns around the mouth indicate possible inhalation burns; respiratory tract injury may result in edema, causing an airway obstruction. An increase in temperature indicates the presence of an infection; it is too early for an infection to occur. Increased activity is promising because it indicates that the burns were not severe. Edema distal to burns of the extremities is an expected finding.
Which wound care is given to a client with severe burn injuries during the acute phase?
A. Assess extent and depth of burns.
B. Provide daily shower and wound care.
C. Remove dead and contaminated tissue.
D. Assess the wound daily and adjust the dressing.
Answer: D
In the acute phase, wound care is given by assessing the wound daily and adjusting the dressing if necessary according to the protocols. Assessing the extent and depth of burns is performed in the emergent phase. Providing a daily shower and removing the dead and contaminated tissue (debriding) is performed in the emergent phase.
Which intervention is beneficial to an older adult in acute care who is at risk of skin breakdown? Select all that apply. One, some, or all responses may be correct.
a. Providing thorough skin care
b. Reducing shear forces and friction
c. Providing beverages and snacks frequently
d. Using a support surface base all the time
e. Avoiding pressure with proper positioning
A, B, & E
Providing an older adult with meticulous skin care may reduce the risk of skin breakdown. Reducing shear forces and friction prevents the development of pressure injuries. Pressure can be avoided with proper positioning. Beverages and snacks are frequently provided to clients who are hospitalized due to dehydration. A supportive surface base is used based on risk factors.
A nurse is caring for a client diagnosed with scabies. Which instruction should the nurse include in the teaching plan?
A. “Apply the scabicide cream only to the areas where scabies mites have created visable burrows.”
B. “Wash all clothing, bedding, and towels used in the past 3 days in hot water and dry on high heat.”
C. “You may stop treatment as soon as the itching resolves.”
D. “Household members only need treatment if they develop itching.”
Correct Answer:
B. Wash all clothing, bedding, and towels used in the past 3 days in hot water and dry on high heat.
Rationale:
Scabies treatment requires permethrin 5% cream applied to the entire body (not just visible burrows), from the neck down (including scalp if involved), and left on for 8–14 hours before washing off.
All close contacts must be treated, regardless of symptoms, to prevent reinfestation.
Bedding, clothing, and linens from the last 3 days should be washed in hot water and dried on high heat, or sealed in a plastic bag for at least 72 hours.
Itching may persist for 2–3 weeks after treatment due to allergic reaction to dead mites, so therapy is not discontinued prematurely.
The nurse is assessing a client’s sacral area and notes a wound with extensive tissue loss, necrotic black eschar, and slough obscuring the wound bed. The depth of the wound cannot be determined because of the necrotic tissue. How should the nurse stage this pressure injury?
A. Stage 3
B. Stage 4
C. Unstageable
D. Deep Tissue Pressure Injury
C. Unstageable
Rationale:
Unstageable: Full-thickness tissue loss where the wound bed is covered by slough and/or eschar, making depth and staging impossible until it is debrided.
Stage 3: Full-thickness loss with visible fat but no exposed bone/tendon.
Stage 4: Full-thickness with exposed bone, tendon, or muscle.
DTPI: Persistent, non-blanchable, deep red/purple discoloration of intact skin or blood-filled blister.
Which amount of lactated Ringer solution would the nurse anticipate being infused in the next 8 hours for a client weighing 132 pounds (60 kilograms) with burns over 35% of the body who arrives at the hospital an hour after being rescued from a fire?
Parkland Formula:
4mL×Body Weight (kg)×%TBSA burned
A. 2100 mL
B. 4200 mL
C. 6300 mL
D. 8400 mL
In the first 8 hours, 4200 mL should be infused. According to the Parkland (Baxter) formula, one-half of the total daily amount of fluid should be administered in the first 8 hours. Because the client weighs 60 kg (132 pounds ÷ 2.2 kg = 60 kg), the calculation is 60 kg × 4 mL/kg × 35% burns = 8400 mL per day; half of this amount should be infused within the first 8 hours. 2100 mL, 6300 mL, and 8400 mL are incorrect calculations.
A client with a Stage 4 pressure injury underwent sharp surgical debridement to remove necrotic tissue. Which nursing action is the priority during the immediate post-debridement period?
A. Apply a transparent film dressing to maintain a moist wound environment.
B. Monitor the wound bed for signs of infection, bleeding, and changes in tissue viability.
C. Encourage the client to ambulate to promote circulation.
D. Administer an emollient cream to the periwound skin to prevent dryness.
Correct Answer:
B. Monitor the wound bed for signs of infection, bleeding, and changes in tissue viability.
Rationale:
After debridement—especially sharp surgical debridement—the wound bed is more vulnerable to infection and bleeding. The nurse must frequently assess for:
Signs of infection: redness, swelling, warmth, purulent drainage, odor, fever.
Bleeding or hemostasis issues.
Changes in tissue viability: color, granulation, or necrosis returning.
Other options may be part of ongoing wound care, but the priority is wound surveillance to promptly detect complications that could threaten healing.
Which intervention would the nurse follow to prevent future falls in an older adult experiencing delirium who sustained a leg fracture caused by a fall? Select all that apply. One, some, or all responses may be correct.
A. Minimizing sedating medications
B. Modifying the home environment
C. Teaching clients about the safe use of the Internet
D. Manage foot and footwear problems
E. Providing information about the effects of using alcohol
A, B &D.
The nursing interventions followed to prevent falls are minimizing medications, modifying the home environment, and managing foot and footwear problems. Teaching clients about the safe use of the Internet may be an effective intervention for preventing delirium. Providing information about the effects of using alcohol is not an intervention for older adults; this action is more beneficial for adolescents.
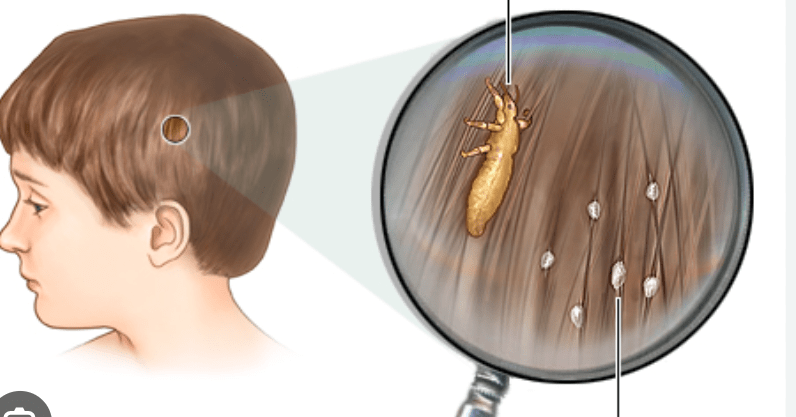
A school nurse is assessing a child who has been scratching the scalp frequently. The nurse observes findings shown in the image: small white oval structures firmly attached to the hair shaft and an adult insect visible under magnification. Which condition does the nurse recognize?
A. Seborrheic dermatitis
B. Plaque psorasis
C. Pediculosis capitis
D. Eczematous dermatitis
Correct Answer:
C. Pediculosis capitis (head lice)
Rationale:
Pediculosis capitis (head lice): Presence of live lice and nits (eggs) firmly attached to the hair shafts, often near the scalp, causing intense itching.
Seborrheic dermatitis: Greasy, yellowish scales on the scalp (“cradle cap” in infants).
Tinea capitis: Fungal infection causing round, scaly patches of hair loss.
Eczematous dermatitis: Pruritic, erythematous patches but no nits or lice present.
Treatment reminder: Management includes permethrin 1% shampoo, nit combing, washing linens/clothing in hot water & high heat, and treating all close contacts.
The nurse assesses a reddened area on a client’s hip with partial-thickness skin loss and a shallow open wound presenting with a pink-red wound bed. No slough or eschar is present. How should the nurse stage this pressure injury?
A. Stage 1
B. Stage 2
C. Stage 3
D. Unstageable

B. Stage 2
Rationale:
Stage 2: Partial-thickness skin loss with exposed dermis; wound bed is viable, pink/red, moist, may present as an intact or ruptured blister.
Stage 1: Intact skin with non-blanchable redness.
Stage 3/4: Full-thickness tissue loss with visible fat, muscle, or bone.
Unstageable: Obscured by slough/eschar.
A nurse is caring for a client in the resuscitation phase of a major burn injury. The provider orders labs, and the nurse reviews the results:
Hematocrit: 55% (normal 36–50%)
Serum albumin: 2.2 g/dL (normal 3.5–5.0 g/dL)
Serum sodium: 128 mEq/L (normal 135–145 mEq/L)
Serum potassium: 5.8 mEq/L (normal 3.5–5.0 mEq/L)
Which set of lab results is most consistent with this stage of burn injury?
a. Hematocrit 55%, albumin 2.2 g/dL, sodium 128 mEq/L, potassium 5.8 mEq/L
b. Hematocrit 28%, albumin 2.2 g/dL, sodium 128 mEq/L, potassium 3.0 mEq/L
c. Hematocrit 28%, albumin 4.5 g/dL, sodium 145 mEq/L, potassium 5.8 mEq/L
d. Hematocrit 55%, albumin 4.5 g/dL, sodium 128 mEq/L, potassium 3.0 mEq/L
a. Hematocrit 55%, albumin 2.2 g/dL, sodium 128 mEq/L, potassium 5.8 mEq/L
Rationale:
During the resuscitation phase of burn injury, increased capillary permeability allows fluid, sodium, and plasma proteins (albumin) to leave the intravascular space and shift into interstitial spaces. This leads to low sodium and low albumin.
Serum potassium rises because injured cells and hemolyzed red blood cells release potassium into circulation, and the sodium-potassium pump is disrupted by tissue damage.
Hematocrit increases due to plasma volume loss into interstitial tissue, causing hemoconcentration.
The other answer choices are incorrect because they reflect combinations of values that do not match the typical physiologic response in the early burn phase.
A nursing student is assessing an immobile patient with a stage 3 pressure injury (see below). The nurse's notes state. "the previous dressing was saturated with copious amounts of serisangenous exudate. Which type of dressing is most appropriate for this wound?

a. Wet-to-damp saline moistened gauze
b. None, thid wound should be left open to the air
c. A thin transparent film
d. Multi-fiber superabsorbent dressing
Correct Answer:
d. Multi-fiber superabsorbent dressing
Detailed Rationale:
Multi-fiber superabsorbent dressing: Best for wounds with heavy drainage/exudate. These dressings absorb large amounts of fluid, maintain a moist wound environment, and prevent maceration of surrounding skin. This makes them appropriate for a Stage 3 wound with copious exudate.
Wet-to-damp saline moistened gauze: Used for mechanical debridement of necrotic tissue, not ideal for managing heavy exudate since it dries out and requires frequent changes.
No dressing (open to air): Not appropriate because a moist environment promotes faster healing and reduces infection risk.
Transparent film: Thin, non-absorbent covering best for Stage 1 or superficial Stage 2 pressure injuries with minimal drainage. It allows visualization of the wound but cannot handle heavy exudate.
The nurse is providing education about pressure injury prevention to a group of nursing students. Which interventions DOES NOT demonstrate appropriate prevention strategies?
A. Teaching a client to shift weight every 15 minutes while in a wheelchair.
B. Performing a Braden scale risk assessment on admission
C. Providing physical therapy and wound care to a client with a Stage 3 pressure injury
D. Recommending that clients avoid salty foods to reduce edema
Answer: D.
Dietary sodium restriction may be useful for other conditions (e.g., hypertension, edema) but is not a primary factor in pressure injury prevention.
Primary prevention (before injury occurs): Interventions like repositioning, pressure-redistribution mattresses, and skin care education are aimed at preventing breakdown.
Secondary prevention (early detection): Screening tools such as the Braden scale identify clients at risk before injuries develop.
Tertiary prevention (reduce complications of existing disease): Includes treatment and rehabilitation for clients with established pressure injuries, such as wound care and mobility programs.
The nurse assesses a client’s skin lesion as shown in the image. Client reports the skin lesion is concerning because it is getting darker over time. Using the ABCDE rule for melanoma, what would note nurse document for the following:
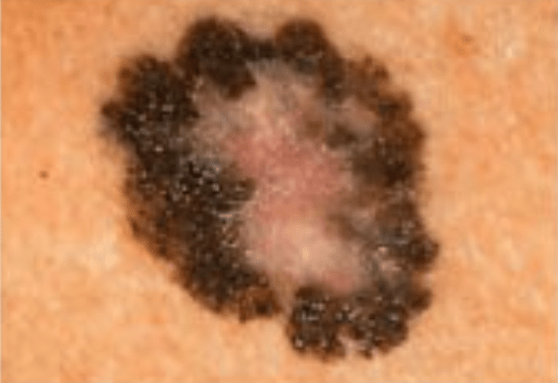
A (Asymmetry): B (Border): C (Color): D (Diameter): E (Evolving):
Based on the findings, how should the nurse classify this lesion?
A. Benign mole
B. Malignant melanoma
C. Basal cell carcinoma
D. Actinic keratosis
A (Asymmetry): One half does not match the other.
B (Border): Irregular and poorly defined.
C (Color): Multiple colors (black, brown, pink, white).
D (Diameter): Approximately 8 mm.
E (Evolving): Patient reports recent changes in size and color.
B. Malignant melanoma
Rationale:
The lesion meets all five concerning criteria of the ABCDE rule: asymmetry, irregular borders, multiple colors, diameter >6 mm, and evolution in appearance. This is strongly suspicious for malignant melanoma. Benign moles are usually symmetric, uniform in color, and <6 mm. Basal cell carcinoma and actinic keratosis appear differently and do not typically match the ABCDE criteria.
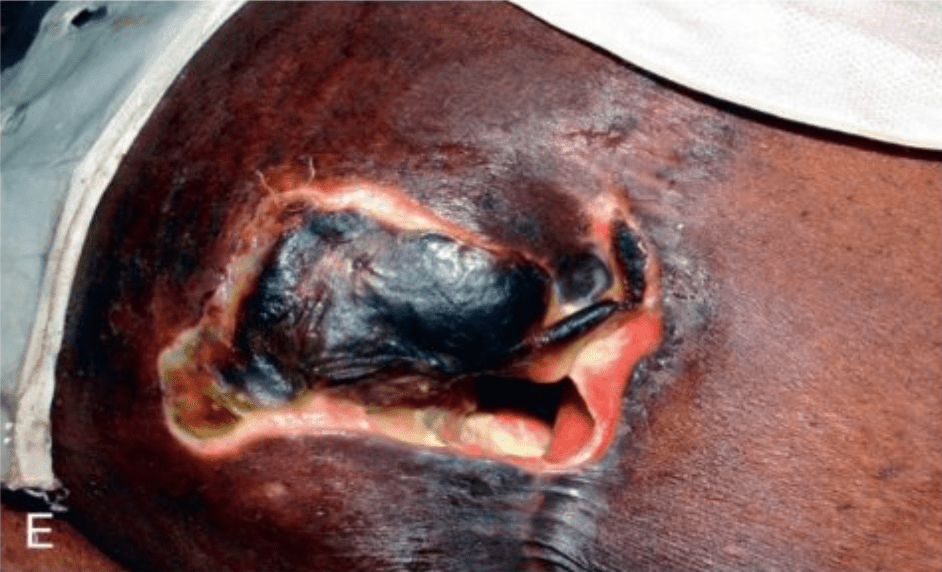
A nurse is caring for a client with the wound shown in the image. The wound extends deep into muscle with exposed tissue, slough present. How should the nurse stage this wound?
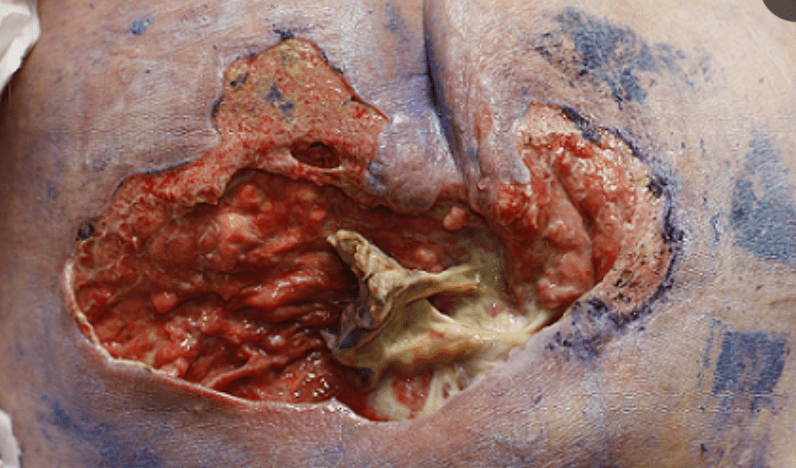
A. Stage 2 pressure injury
B. Stage 3 pressure injury
C. Stage 4 pressure injury
D. Unstageable pressure injury
Correct Answer:
C. Stage 4 pressure injury; prepare the wound bed with debridement and apply appropriate advanced dressings.
Rationale:
Stage 4 pressure injury: Full-thickness skin and tissue loss with exposed muscle, tendon, or bone. Slough and eschar may also be present. Requires aggressive management including debridement, infection surveillance, moist wound healing dressings, and often surgical consult.
Stage 2: Shallow, partial-thickness loss of dermis (blister or abrasion).
Stage 3: Full-thickness skin loss with visible fat but no exposed muscle, tendon, or bone.
Unstageable: Depth is obscured by slough/eschar; in this image, depth is visible → not unstageable.
When assessing the entrance and exit wounds of this client with an electrical burns, which fact should the nurse remember?

A. Electrical burns always cause severe skin destruction that is easy to trace externally.
B. Electrical current travels through nerves and blood vessels, the least resistant tissues.
C. The burn path can always be tracked visually from the contact point to the grounding point.
D. Direct current causes less tissue destruction than alternating current.
Correct Answer:
B. Electrical current travels through nerves and blood vessels, the least resistant tissues.
Rationale (condensed):
Nerves and blood vessels conduct electricity easily, so injury is often deeper and more severe internally than it appears on the skin. Entrance and exit wounds may not show the true extent of tissue damage.
The nurse is performing wound care on a 65 year old client with a large abdominal wound. The physician's orders: wet-to-dry dressing twice daily and as needed. Clean with 0.9% Normal Saline, pack with sterile 4x4 gauze, Santyl to wound edges and cover with abdominal (ABD) pads.
Put the following wound care steps in order:
A. Don clean gloves, open sterile gauze packs and moisten with normal saline.
B. Cover entire wound area with abdominal (ABD) pad and tape using the window-pane technique.
C. Assess drainage on old dressing for COCA (color, odor, consistency and amount). Discard old dressing and doff gloves. Perform hand hygiene.
D. Using a clean cotton tip, apply Santyl to the wound edges avoiding the center of the wound.
E. Perform hand hygiene, collect necessary supplies, and don clean gloves and remove old wound dressing.
F. Clean wound starting with least contaminated area and moving outward.
G. Moisten sterile 4x4 gauze until fully saturated and apply to center of wound bed.
Correct Order: E, C, A, F, D, G, B
A. Perform hand hygiene, collect necessary supplies, and don clean gloves and remove old wound dressing.
B. Assess drainage on old dressing for COCA (color, odor, consistency, and amount). Discard old dressing and doff gloves. Perform hand hygiene.
C. Don clean gloves, open sterile gauze packs and moisten with normal saline.
D. Clean wound starting with least contaminated area and moving outward.
E. Using a clean cotton tip, apply Santyl to the wound edges avoiding the center of the wound.
F. Moisten sterile 4x4 gauze until fully saturated and apply to center of wound bed.
G. Cover entire wound area with abdominal (ABD) pad and tape using the window-pane technique.