Cely with manic episodes is taking lithium. Which electrolyte level should the nurse check before administering this medication?
1. Calcium
2. Sodium
3. Chloride
4. Potassium
2. Sodium
Lithium is chemically similar to sodium. If sodium levels are reduced, such as from sweating or diuresis, lithium will be reabsorbed by the kidneys, increasing the risk of toxicity. Clients taking lithium shouldn’t restrict their intake of sodium and should drink adequate amounts of fluid each day. It is also important to monitor patients for dehydration and lower the dose when there are signs of infection, excessive sweating, or diarrhea. Toxic levels are when the drug level is more than 2 mEq/L.
Which question would the nurse ask to assess a patient‘s dysuria?
1. “Do you have to urinate at night?”
2. “Do you have blood in your urine?”
3.“Do you have to urinatefrequently?”
4. “Do you have pain when you urinate?”
4. “Do you have pain when you urinate?”
Dysuria is painful urination. The alternate responses can be used to assess other urinary tract symptoms: hematuria, nocturia, and frequency.
A patient vomiting blood-streaked fluid is admitted to the hospital with acute gastritis. What would the nurse ask the patient about to determine possible risk factors for gastritis?
1. The amount of saturated fat in the diet
2. A family history of gastric or colon cancer
3. Use of nonsteroidal anti-inflammatory drugs
4. A history of a large recent weight gain or loss
3. Use of NSAIDs
Use of an NSAID is associated with damage to the gastric mucosa, which can result in acute gastritis. Family history, recent weight gain or loss, and fatty foods are not risk factors for acute gastritis.
A patient with a large stomach tumor attached to the liver is scheduled for a debulking procedure. Which information would the nurse teach the patient about the expected outcome of this procedure?
1. Pain will be relieved by cutting sensory nerves in the stomach.
2. Decreasing the tumor size will improve the effects of other therapy.
3. Relieving the pressure in the stomach will promote optimal nutrition.
4. Tumor growth will be controlled by removing all the cancerous tissue.
2. Decreasing the tumor size will improve the effects of other therapy.
A debulking surgery reduces the size of the tumor and makes radiation and chemotherapy more effective. Debulking surgeries do not control tumor growth. The tumor is debulked because it is attached to the liver, a vital organ (not to relieve pressure on the stomach). Debulking does not sever the sensory nerves, although pain may be lessened by the reduction in pressure on the abdominal organs.
A patient who has just been started on enteral nutrition of full-strength formula at 100 mL/hr has 6 liquid stools the first day. Which action would the nurse plan to take?
1. Slow the infusion rate of the feeding.
2. Check gastric residual volumes more often.
3. Change the enteral feeding system and formula every 8 hours.
4. Discontinue administration of water through the feeding tube.
1. Slow the infusion rate of the feeding.
Loose stools indicate poor absorption of nutrients and indicate a need to slow the feeding rate or decrease the concentration of the feeding. Water should be given when patients receive enteral feedings to prevent dehydration. When a closed enteral feeding system is used, the tubing and formula are changed every 24 hours. High residual volumes do not contribute to diarrhea.
A patient receives aspart (NovoLog) insulin at 8:00 AM. At which time would the nurse anticipate the highest risk for hypoglycemia?
1. 10:00 AM
2. 12:00 AM
3. 2:00 PM
4. 4:00 PM
1. 10:00 AM
The rapid-acting insulins peak in 1 to 3 hours. The patient is not at a high risk for hypoglycemia at the other listed times, although hypoglycemia may occur.
Joe who is very depressed exhibits psychomotor retardation, a flat affect, and apathy. The nurse in charge observes Joe to be in need of grooming and hygiene. Which of the following nursing actions would be most appropriate?
1. Waiting until the client’s family can participate in the client’s care.
2. Asking the client if he is ready to take a shower.
3. Explaining the importance of hygiene to the client.
4. Stating to the client that it’s time for him to take a shower.
4. Stating to the client that it’s time for him to take a shower.
The client with depression is preoccupied, has decreased energy, and is unable to make decisions. The nurse presents the situation, “It’s time for a shower”, and assists the client with personal hygiene to preserve his dignity and self-esteem. Encourage the use of soap, washcloth, toothbrush, shaving equipment, make-up, etc. Being clean and well-groomed can temporarily increase self-esteem.
How will the nurse assess for flank tenderness in a patient with suspected pyelonephritis?
1. Palpate along both sides of the lumbar vertebral column.
2. Strike a flat hand covering the costovertebral angle (CVA).
3. Push fingers upward into the two lowest intercostal spaces.
4. Percuss between the iliac crest and ribs at the midaxillary line.
2. Strike a flat hand covering the costovertebral angle (CVA).
Checking for flank pain is performed by percussion of the CVA and asking about pain. The other techniques would not assess for flank pain.
A patient with a stroke is unconscious and unresponsive to stimuli. After learning that the patient has a history of gastroesophageal reflux disease (GERD), which assessment would the nurse plan to make more frequently than is routine?
1. Apical pulse
2. Bowel sounds
3. Breath sounds
4. Abdominal girth
3. Breath sounds
Because GERD may cause aspiration, the unconscious patient is at risk for developing aspiration pneumonia. Bowel sounds, abdominal girth, and apical pulse will not be affected by the patient‘s stroke or GERD and do not require more frequent monitoring than the routine.
The nurse teaches a postmenopausal patient with stage III breast cancer about the expected outcomes of cancer treatment. Which patient statement indicates that the teaching has been effective?
1. “After cancer has not recurred for 5 years, it is considered cured.”
2. “The cancer will be cured if the entire tumor is surgically removed.”
3. “I will need follow-up examinations for many years after treatment before I can be considered cured.”
4. “Cancer is never cured, but the tumor can be controlled with surgery, chemotherapy, and radiation.”
3. “I will need follow-up examinations for many years after treatment before I can be considered cured.”
The risk of recurrence varies by the type of cancer. Some cancers are considered cured after a shorter time span or after surgery, but stage III breast cancer will require additional therapies and ongoing follow-up.
A severely malnourished patient reports that he is Jewish. Which initial action would the nurse take to meet his nutritional needs?
1. Have family members bring in food.
2. Ask the patient about food preferences.
3. Teach the patient about nutritious Kosher foods.
4. Order supplements that are manufactured Kosher.
2. Ask the patient about food preferences.
The nurse‘s first action would be further assessment of whether the patient follows any specific religious guidelines that impact nutrition. The other actions may also be appropriate, based on the information obtained during the assessment.
A patient is being admitted with a diagnosis of Cushing syndrome. Which finding will the nurse expect during the assessment?
1. Chronically low blood pressure
2. Bronzed appearance of the skin
3. Purplish streaks on the abdomen
4. Decreased axillary and pubic hair
3. Purplish streaks on the abdomen
Purplish-red striae on the abdomen are a common clinical manifestation of Cushing syndrome. Hypotension and bronzed-appearing skin are manifestations of Addison‘s disease. Decreased axillary and pubic hair occur with androgen deficiency.
Kathleen is admitted to the psychiatric clinic for treatment of anorexia nervosa. To promote the client’s physical health, the nurse should plan to:
1. Severely restrict the client's physical activities.
2. Weigh the client daily, after the evening meal.
3. Monitor vital signs, serum electrolyte levels, and acid-base balance.
4. Instruct the client to keep an accurate record of food and fluid intake.
3. Monitor vital signs, serum electrolyte levels, and acid-base balance.
An anorexic client who requires hospitalization is in poor physical condition from starvation and may die as a result of arrhythmias, hypothermia, malnutrition, infection, or cardiac abnormalities secondary to electrolyte imbalances. Therefore, monitoring the client’s vital signs, serum electrolyte level, and acid-base balance is crucial. Work-up includes a thorough medical history (comprehensive review of systems, family and social history, medications including non-prescribed, past medical and psychiatric history, prior abuse) and physical exam (looking for complications above).
Which nursing action is essential for a patient immediately after a renal biopsy?
1. Insert a urinary catheter and test urine for microscopic hematuria.
2. Check blood glucose to assess for hyperglycemia or hypoglycemia.
3. Apply a pressure dressing and position the patient on the affected side.
4. Monitor blood urea nitrogen (BUN) and creatinine to assess renal function.
3. Apply a pressure dressing and position the patient on the affected side.
A pressure dressing is applied, and the patient is kept on the affected side for 30 to 60 minutes to put pressure on the biopsy side and decrease the risk for bleeding. The blood glucose and BUN/creatinine will not be affected by the biopsy. Although monitoring for hematuria is needed, there is no need for catheterization.
A patient has just returned to the nursing unit after an esophagogastroduodenoscopy (EGD). Which action by assistive personnel (AP) requires that the registered nurse (RN) intervene?
1. Offering the patient a pitcher of water
2. Positioning the patient on the right side
3. Checking the vital signs every 30 minutes
4. Swabbing the patient‘s mouth with a wet cloth
1. Offering the patient a pitcher of water
Immediately after EGD, the patient will have a decreased gag reflex and is at risk for aspiration. Assessment for return of the gag reflex should be done by the RN. The other actions by the AP are appropriate.
A patient undergoing external radiation has developed a dry desquamation of the skin in the treatment area. The nurse teaches the patient about the management of the skin reaction. Which statement, if made by the patient, indicates the teaching was effective?
1. “I can use ice packs to relieve itching.”
2. “I will scrub the area with warm water.”
3. “I can apply aloe vera gel after I bathe.”
4. “I will expose my skin to a sun lamp each day.”
3. “I can apply aloe vera gel after I bathe.”
Aloe vera gel may be used on the radiated skin area. Ice and sunlamps may injure the skin. Treatment areas would be cleaned gently to avoid further injury.
A 20-yr-old woman is being admitted with electrolyte disorders of unknown etiology. Which assessment finding is most important to report to the health care provider?
1. The patient uses laxatives daily.
2. The patient‘s knuckles are macerated.
3. The patient‘s serum potassium level is 3.2 mEq/L.
4. The patient has a history of extreme weightfluctuations.
3. The patient‘s serum potassium level is 3.2 mEq/L.
The low serum potassium level may cause life-threatening cardiac dysrhythmias, and potassium supplementation is needed rapidly. The other information will also be reported because it suggests that bulimia may be the etiology of the patient‘s electrolyte disturbances, but it does not suggest imminent life-threatening complications.
Which finding indicates to the nurse that demeclocycline has been effective for a patient with syndrome of inappropriate antidiuretic hormone (SIADH)?
1. Weight has increased.
2. Urinary output has increased.
3. Peripheral edema has increased.
4. Urine specific gravity has increased.
2. Urine output has increased
Demeclocycline blocks the action of antidiuretic hormone (ADH) on the renal tubules and increases urine output, producing more dilute urine. An increase in weight or an increase in urine specific gravity indicates that the SIADH is not corrected. Peripheral edema does not occur with SIADH. A sudden weight gain without edema is a common clinical manifestation of this disorder.
Mr. Garcia, an attorney who throws books and furniture around the office after losing a case, is referred to the psychiatric nurse in the law firm’s employee assistance program. Nurse Beatriz knows that the client’s behavior most likely represents the use of which defense mechanism?
1. Regression
2. Projection
3. Reaction-formation
4. Intellectualization
1. Regression
An adult who throws temper tantrums, such as this one, is displaying regressive behavior, or behavior that is appropriate at a younger age. Adapting one’s behavior to earlier levels of psychosocial development. For example, a stressful event may cause an individual to regress to bed-wetting after they have already outgrown this behavior.
What glomerular filtration rate (GFR) would the nurse estimate for a 30-yr-old patient with a creatinine clearance result of 60 mL/min?
1. 60 mL/min
2. 90 mL/min
3. 120 mL/min
4. 180 mL/min
1. 60 ml/min
The creatinine clearance approximates the GFR. The other responses are not accurate.
The nurse has completed teaching a patient with newly diagnosed eosinophilic esophagitis about the management of the disease. Which patient action indicates that the teaching has been effective?
1. Patient orders nonfat milk for each meal.
2. Patient uses the prescribed corticosteroid inhaler.
3. Patient schedules an appointment for allergy testing.
4. Patient takes ibuprofen (Advil) to control throat pain.
3. Patient schedules an appointment for allergy testing
Eosinophilic esophagitis is frequently associated with environmental allergens, so allergy testing is used to determine possible triggers. Corticosteroid therapy may be prescribed, but the medication will be swallowed, not inhaled. Milk is a frequent trigger for attacks. NSAIDs are not used for eosinophilic esophagitis.
An IV vesicant chemotherapeutic agent is prescribed for a patient. Which action is would the nurse plan to take?
1. Infuse the medication over a short period of time.
2. Stop the infusion if swelling is observed at the site.
3. Administer the medication through a small-bore catheter.
4. Hold the medication until a central venous line is available.
2. Stop the infusion if swelling is observed at the site.
Swelling at the site may indicate extravasation, and the IV should be stopped immediately. The medication generally should be given slowly to avoid irritation of the vein. The size of the catheter is not as important as administration of vesicants into a running IV line to allow dilution of the chemotherapy drug. These medications can be given through peripheral lines, although central vascular access devices are preferred.
A patient hospitalized with chronic heart failure eats only about 50% of each meal and reports “feeling too tired to eat.” Which action would the nurse take first?
1. Teach the patient about the importance of good nutrition.
2. Serve multiple small feedings of high-calorie, high-protein foods.
3. Consult with the health care provider about parenteral nutrition (PN).
4. Obtain an order for enteral feedings of liquid nutritional supplements.
2. Serve multiple small feedings of high-calorie, high-protein foods.
Eating small amounts of food frequently throughout the day is less fatiguing and will improve the patient‘s ability to take in more nutrients. Teaching the patient may be appropriate but will not address the patient‘s inability to eat more because of fatigue. Enteral nutrition or PN may be needed if the patient is unable to take in enough nutrients orally but increasing the oral intake should be attempted first.
A patient who is disoriented and reports a headache and muscle cramps is hospitalized with syndrome of inappropriate antidiuretic hormone (SIADH). Which initial laboratory result would the nurse expect?
1. Elevated hematocrit
2. Decreased serum sodium
3. Increased serum chloride
4. Low urine specific gravity
2. Decreased serum sodium
When water is retained, the serum sodium level will drop below normal, causing the clinical manifestations reported by the patient. The hematocrit will decrease because of the dilution caused by water retention. Urine will be more concentrated with a higher specific gravity. The serum chloride level will usually decrease along with the sodium level.
Isabel with a diagnosis of depression is started on imipramine (Tofranil), 75 mg by mouth at bedtime. The nurse should tell the client that:
1. This medication may be habit-forming and will be discontinued as soon as the client feels better.
2. This medication has no serious adverse effects.
3. The client should avoid eating such foods as aged cheeses, yogurt, and chicken livers while taking the medication.
4. This medication may initially cause tiredness, which should become less bothersome over time.
4. This medication may initially cause tiredness, which should become less bothersome over time.
Sedation is a common early adverse effect of imipramine, a tricyclic antidepressant, and usually decreases as tolerance develops. Since imipramine acts on various receptors in the body, it presents with adverse effects on some organs and systems. In the central and autonomic nervous system, the antihistaminic effects of imipramine can lead to dizziness, sedation, confusion, delirium, seizures, increased appetite, and weight gain.
Which topic would the nurse include when teaching the patient ways to prevent the recurrence of kidney stones?
1. Using a filter to strain all urine
2. Drinking 3000 mL of fluid each day
3. Avoiding dietary sources of calcium
4. Choosing diuretic fluids such as coffee
2. Drinking 3000 mL of fluid each day
A fluid intake of 2000 to 3000 mL/day is recommended to help flush out minerals before stones can form. Avoidance of calcium is not usually recommended for patients with kidney stones. Coffee tends to increase stone recurrence. Straining all urine routinely after a stone has passed will not prevent stones.
Which test would the nurse anticipate using for a patient who has a new report of heartburn?
1. Radionuclide tests
2. Barium swallow exam
3. Endoscopy procedures
4. Proton pump inhibitors
4. Proton pump inhibitors
Because diagnostic testing for heartburn that is probably caused by gastroesophageal reflux disease (GERD) is expensive and uncomfortable, proton pump inhibitors are frequently used for a short period as the first step in the diagnosis of GERD. The other tests may be used but are not usually the first step in diagnosis.
A patient with leukemia is considering whether to have hematopoietic stem cell transplantation (HSCT). Which information would the nurse include in the patient‘s teaching plan?
1. Donor bone marrow is transplanted through a sternal or hip incision.
2. Protective isolation is required for several weeks after the stem cell transplant.
3. The transplant procedure takes place in a sterile operating room to decrease the risk for infection.
4. Transplant of the donated cells can be very painful because of the nerves in the tissue lining the bone.
2. Protective isolation is required for several weeks after the stem cell transplant.
The patient requires strict protective isolation to prevent infection for 2 to 4 weeks after HSCT while waiting for the transplanted marrow to start producing cells. The transplanted cells are infused through an IV line so the transplant is not painful, nor is an operating room or incision required.
A young adult with extensive facial injuries from a motor vehicle crash is receiving continuous enteral nutrition through a percutaneous endoscopic gastrostomy (PEG). Which action will the nurse include in the plan of care?
1. Keep the patient positioned lying on the left side.
2. Flush the tube with 30 mL of water every 4hours.
3. Crush and mix medications in with the feeding formula.
4. Obtain a daily abdominal radiograph to verify tube placement.
2. Flush the tube with 30 mL of water every 4hours.
The tube is flushed every 4 hours during continuous feedings to avoid tube obstruction. The patient should be positioned with the head of the bed elevated. Crushed medications mixed in with the formula are likely to clog the tube. An x-ray is obtained immediately after placement of the PEG tube to check position, but daily x-rays are not needed.
A patient who takes metformin (Glucophage) to manage type 2 diabetes developed an allergic rash from an unknown cause and the health care provider prescribed prednisone. Which change in the plan of care at would the nurse anticipate?
1. The patient may need a diet higher in calories while receiving prednisone.
2. The patient may develop acute hypoglycemia while taking the prednisone.
3. The patient may require administration of insulin while taking prednisone.
4. The patient may have rashes caused by metformin-prednisone interactions.
3. The patient may require administration of insulin while taking prednisone
Glucose levels increase when patients are taking corticosteroids, and insulin may be required to control glucose. Hypoglycemia is not a side effect of prednisone. Rashes are not an adverse effect caused by taking metformin and prednisone simultaneously. The patient may have an increased appetite when taking prednisone but will not need a diet that is higher in calories.
When teaching Mario with a typical depression about foods to avoid while taking phenelzine(Nardil), which of the following would the nurse in charge include?
1. Roasted chicken
2. Fresh fish
3. Salami
4. Hamburger
3. Salami
Foods high in tyramine, those that are fermented, pickled, aged, or smoked must be avoided because when they are ingested in combination with MAOIs a hypertensive crisis will occur. MAOIs prevent the breakdown of tyramine found in the body as well as certain foods, drinks, and other medications. Patients that take MAOIs and consume tyramine-containing foods or drinks will exhibit high serum tyramine level. A high level of tyramine can cause a sudden increase in blood pressure, called the tyramine pressor response. Even though it is rare, a high tyramine level can trigger a cerebral hemorrhage, which can even result in death.
A 28-yr-old male patient has just been diagnosed with polycystic kidney disease. Which information would the nurse include during the first teaching session?
1. Complications of renal transplantation
2. Methods for treating severe chronic pain
3. Options to consider for genetic counseling
4. Differences between hemodialysis and peritoneal dialysis
3. Options to consider for genetic counseling
Because a 28-yr-old patient may be considering having children, the nurse would include information about genetic counseling when teaching the patient. A patient with good health- management will not need to choose between hemodialysis and peritoneal dialysis or know about the effects of transplantation for many years. There is no indication that the patient has chronic pain.
Which action would the nurse take after assisting with a needle biopsy of the liver at a patient‘s bedside?
1. Elevate the head of the bed to facilitate breathing.
2. Place the patient on the right side with the bed flat.
3. Check the patient‘s post biopsy coagulation studies.
4. Position a sandbag over the liver to provide pressure.
2. Place the patient on the right side with the bed flat.
After a biopsy, the patient lies on the right side with the bed flat to splint the biopsy site. Coagulation studies are checked before the biopsy. A sandbag does not exert adequate pressure to splint the site.
Interleukin-2 (IL-2) is used as adjuvant therapy for a patient with metastatic renal cell carcinoma. Which information would the nurse include when explaining the purpose of this therapy to the patient?
1. IL-2 enhances the body‘s immunologic response to tumor cells.
2. IL-2 prevents bone marrow depression caused by chemotherapy.
3. IL-2 protects normal cells from harmful effects of chemotherapy.
4. IL-2 stimulates cancer cells in their resting phase to enter mitosis.
1. IL-2 enhances the body‘s immunologic response to tumor cells.
IL-2 enhances the ability of the patient‘s own immune response to suppress tumor cells. IL-2 does not protect normal cells from damage caused by chemotherapy, stimulate cancer cells to enter mitosis, or prevent bone marrow depression
A malnourished patient is receiving a parenteral nutrition (PN) infusion containing amino acids and dextrose from a bag that was hung with a new tubing and filter 24 hours ago. The nurse observes that about 50 mL remain in the PN container. Which action would the nurse take?
1. Add a new container of PN using the current tubing and filter.
2. Hang a new container of PN and change the IV tubing and filter.
3. Infuse the remaining 50 mL and then hang a new container of PN.
4. Ask the health care provider to clarify the written PN prescription.
2. Hang a new container of PN and change the IV tubing and filter.
All PN solutions and tubings are changed at 24 hours. Infusion of the additional 50 mL will increase patient risk for infection. The nurse (not the health care provider) is responsible for knowing the indicated times for tubing and filter changes.
Which assessment finding in a patient who had a bilateral adrenalectomy requires the most rapid action by the nurse?
1. The blood glucose is 192 mg/dL.
2. The lungs have bibasilar crackles.
3. The patient reports 6/10 incisional pain.
4. The blood pressure (BP) is 88/50 mm Hg.
4. The blood pressure (BP) is 88/50 mm Hg.
The decreased BP indicates possible adrenal insufficiency. The nurse would immediately notify the health care provider so that corticosteroid medications can be administered. The nurse would also address the elevated glucose, incisional pain, and crackles with appropriate collaborative or nursing actions, but prevention and treatment of acute adrenal insufficiency are the priorities after adrenalectomy.
Which information is most important for the nurse Trinity to include in a teaching plan for a male schizophrenic client taking clozapine (Clozaril)?
1. Monthly blood tests will be necessary.
2. Report a sore throat or fever to the physician immediately.
3. Blood pressure must be monitored for hypertension.
4. Stop the medication when symptoms subside.
2. Report a sore throat or fever to the physician immediately.
A sore throat and fever are indications of an infection caused by agranulocytosis, a potentially life-threatening complication of clozapine. The risk of developing agranulocytosis is around 1% in patients who take clozapine, which may be independent of dosing. Most cases occur early in the treatment, within six weeks to six months, and require extensive monitoring of blood absolute neutrophil counts. The definition of neutropenia is an ANC level below 1500/mm, and agranulocytosis is an ANC level below 500/mm.
Which information will the nurse monitor to determine the effectiveness of prescribed calcium carbonate (Caltrate) for a patient with chronic kidney disease (CKD)?
1. Blood pressure
2. Phosphate level
3. Neurologic status
4. Creatinine clearance
2. Phosphate level
Calcium carbonate is prescribed to bind phosphorus and prevent mineral and bone disease in patients with CKD. The other data will not be helpful in evaluating the effectiveness of calcium carbonate.
Four hours after a bowel resection, a 74-yr-old male patient with a nasogastric tube to suction reports nausea and abdominal distention. Which action would the nurse take first?
1. Auscultate for hypotonic bowel sounds.
2. Notify the patient‘s health care provider.
3. Check for tube placement and reposition it.
4. Remove the tube and replace it with a new one.
3. Check for tube placement and reposition it.
Repositioning the tube will frequently facilitate drainage. Because this is a common occurrence, it is not appropriate to notify the health care provider unless other interventions do not resolve the problem. Information about the presence or absence of bowel sounds will not be helpful in improving drainage. Removing the tube and replacing it are unnecessarily traumatic to the patient, so that would only be done if the tube was completely occluded.
The nurse receives change-of-shift handoff report on the oncology unit. Which patient would the nurse assess first?
1. A 35-yr-old patient who has wet desquamation associated with abdominal radiation
2. A 42-yr-old patient who is sobbing after receiving a new diagnosis of ovarian cancer
3. A 24-yr-old patient who received neck radiation and has blood oozing from the neck
4. A 56-yr-old patient who developed a new pericardial friction rub after chest radiation
3. A 24-yr-old patient who received neck radiation and has blood oozing from the neck
Because neck bleeding may indicate impending carotid artery rupture in a patient who is receiving radiation to the neck, this patient should be seen first. The diagnoses and clinical manifestations for the other patients are not immediately life threatening.
After change-of-shift report, which patient will the nurse assess first?
1. A 40-yr-old woman whose parenteral nutrition infusion bag has 30 minutes of solution left
2. A 40-yr-old man with continuous enteral feedings who has developed crackles
3. A 30-yr-old man with 4+ generalized pitting edema and severe protein-calorie malnutrition
4. A 30-yr-old woman whose gastrostomy tube is plugged after crushed medications were administered
2. A 40-yr-old man with continuous enteral feedings whohas developed crackles
The patient data suggest aspiration may have occurred, and rapid assessment and intervention are needed. The other patients should also be assessed soon, but the data about them do not suggest any immediately life-threatening complications.
Which finding by the nurse when assessing a patient with Hashimoto‘s thyroiditis and a goiter will require the most immediate action?
1. New-onset changes in the patient‘s voice
2. Elevation in the patient‘s T3 and T4 levels
3. Resting apical pulse rate 112 beats/min
4. Bruit audible bilaterally over the thyroid gland
1. New-onset changes in the patient‘s voice
Changes in the patient‘s voice indicate that the goiter is compressing the laryngeal nerve and may lead to airway compression. The other findings will also be reported but are expected with Hashimoto‘s thyroiditis and do not require immediate action.
Danny, who is diagnosed with bipolar disorder and acute mania, states the nurse, “Where is my daughter? I love Louis. Rain, rain go away. Dogs eat dirt.” The nurse interprets these statements as indicating which of the following?
1. Echolalia
2. Neologism
3. Clang associations
4. Flight of ideas
4. Flight of ideas
Flight of ideas is a speech pattern of rapid transition from topic to topic, often without finishing one idea. It is common in mania. A nearly continuous flow of accelerated speech with abrupt changes from topic to topic that are usually based on understandable associations, distracting stimuli, or plays on words. When severe, speech may be disorganized and incoherent. It is part of the DSM-5 criteria for Manic episodes.
Option 1: People with echolalia repeat noises and phrases that they hear. They may not be able to communicate effectively because they struggle to express their own thoughts. For example, someone with echolalia might only be able to repeat a question rather than answer it. In many cases, echolalia is an attempt to communicate, learn language, or practice language.
Option 2: In a neurological or psychopathological context, neologisms, whose origins and meanings are usually nonsensical and unrecognizable (e.g., klipno for watch), are typically associated with aphasia or schizophrenia.
Option 3: Clang associations are groups of words chosen because of the catchy way they sound, not because of what they mean. Clanging word groups don’t make sense together. People who speak using repetitive clang associations may have a mental health condition such as schizophrenia or bipolar disorder.
Which information in the patient history would indicate a possible cause of acute glomerulonephritis?
1. Recent bladder infection
2. History of kidney stones
3. Recent sore throat and fever
4. History of high blood pressure
3. Recent sore throat and fever
Acute glomerulonephritis frequently occurs after a streptococcal infection such as strep throat. It is not caused by kidney stones, hypertension, or urinary tract infection.
A patient has peptic ulcer disease associated with Helicobacter pylori. Which medications will the nurse plan to teach the patient?
1. Sucralfate (Carafate), nystatin, and bismuth (Pepto-Bismol)
2. Metoclopramide (Reglan), bethanechol, and promethazine
3. Amoxicillin (Amoxil), clarithromycin, and omeprazole (Prilosec)
4. Famotidine (Pepcid), magnesium hydroxide (Mylanta), and pantoprazole
3. Amoxicillin (Amoxil), clarithromycin, and omeprazole (Prilosec)
The drugs used in triple drug therapy include a proton pump inhibitor such as omeprazole and the antibiotics amoxicillin and clarithromycin. The other combinations listed are not included in the protocol for H. pylori infection.
The nurse assesses a patient who is receiving interleukin-2. Which finding would the nurse report immediately to the health care provider?
1. Generalized muscle aches
2. Crackles at the lung bases
3. Report of nausea and anorexia
4. Oral temperature of 100.6F (38.1C)
2. Crackles at the lung bases
Capillary leak syndrome and acute pulmonary edema are possible toxic effects of interleukin-2. The patient may need oxygen and the nurse should rapidly notify the health care provider. Common side effects of interleukin-2 are flu-like symptoms, including headache, fever, chills, myalgias, fatigue, malaise, weakness, photosensitivity, anorexia, and nausea.
A patient‘s peripheral parenteral nutrition (PN) bag is nearly empty, and a new PN bag has not arrived yet from the pharmacy. Which action would the nurse take?
1. Monitor the patient‘s capillary blood glucose every 6 hours.
2. Infuse 5% dextrose in water until a new PN bag is delivered.
3. Decrease the PN infusion rate to 10 mL/hr until a new bag arrives.
4. Flush the peripheral line with saline until a new PN bag is available.
2. Infuse 5% dextrose in water until a new PN bag isdelivered.
To prevent hypoglycemia, the nurse should infuse a 5% dextrose solution until the next peripheral PN bag can be started. Decreasing the rate of the ordered PN infusion is beyond the nurse‘s scope of practice. Flushing the line and then waiting for the next bag may lead to hypoglycemia. Monitoring the capillary blood glucose every 6 hours would not identify hypoglycemia while awaiting the new PN bag.
The nurse is planning postoperative care for a patient who is being admitted to the surgical unit from the recovery room after transsphenoidal resection of a pituitary tumor. Which nursing action would be included?
1. Palpate extremities for edema.
2. Measure urine volume every hour.
3. Check hematocrit every 2 hours for 8 hours.
4. Monitor continuous pulse oximetry for 24 hours.
2. Measure urine volume every hour
After pituitary surgery, the patient is at risk for diabetes insipidus caused by cerebral edema. Monitoring of urine output and urine specific gravity is essential. Hemorrhage is not a common problem. There is no need to check the hematocrit hourly. The patient is at risk for dehydration, not volume overload. The patient is not at high risk for problems with oxygenation, so continuous pulse oximetry is not needed.
Ricky with chronic schizophrenia takes neuroleptic medication and is admitted to the psychiatric unit. Nursing assessment reveals altered mental status, fever, hypertension, and diaphoresis. These findings suggest which life-threatening reaction:
1. Tardive dyskinesia
2. Dystonia
3. Neuroleptic malignant syndrome
4. Akathisia
3. Neuroleptic malignant syndrome
The client’s signs and symptoms suggest neuroleptic malignant syndrome, a life-threatening reaction to neuroleptic medication that requires immediate treatment. Neuroleptic malignant syndrome (NMS) is a life-threatening idiosyncratic reaction to antipsychotic drugs characterized by fever, altered mental status, muscle rigidity, and autonomic dysfunction. It has been associated with virtually all neuroleptics, including newer atypical antipsychotics, as well as a variety of other medications that affect central dopaminergic neurotransmission.
Option 1: Tardive dyskinesia causes involuntary movements of the tongue, mouth, facial muscles, and arm and leg muscles. Tardive dyskinesia (TD) is a syndrome which includes a group of iatrogenic movement disorders caused due to a blockade of dopamine receptors. The movement disorders include akathisia, dystonia, buccolingual stereotypy, myoclonus, chorea, tics, and other abnormal involuntary movements which are commonly caused by the long-term use of typical antipsychotics.
Option 2: Dystonia is characterized by cramps and rigidity of the tongue, face, neck, and back muscles. Dystonia is defined by involuntary maintained contraction of agonist and antagonist muscles yielding abnormal posturing, twisting, and repetitive movements or tremulous and can be initiated or worsened by attempted movement.
Option 4: Akathisia causes restlessness, anxiety, and jitteriness. Akathisia is defined as an inability to remain still. It is a neuropsychiatric syndrome that is associated with psychomotor restlessness. The individual with akathisia will generally experience an intense sensation of unease or an inner restlessness that usually involves the lower extremities. This results in a compulsion to move. In most cases the movement is repetitive. The individual may cross, uncross, swing, or shift from one foot to the other. To the observer, this may appear as a persistent fidget.
A patient has been diagnosed with urinary tract stones that are high in uric acid. Which foods will the nurse teach the patient to avoid or limit? (Select all that apply.)
1. Milk
2. Liver
3. Spinach
4. Chicken
5. Cabbage
6. Chocolate
2,4: Liver and Chicken
Meats contain purines, which are metabolized to uric acid. The other foods might be restricted in patients who have calcium or oxalate stones.
The health care provider prescribes antacids and sucralfate (Carafate) for treatment of a patient‘s peptic ulcer. Which medication schedule would the nurse teach the patient?
1. Sucralfate at bedtime and antacids before each meal
2. Sucralfate and antacids together 0 minutes before meals
3. Antacids 30 minutes before each dose of sucralfate is taken
4. Antacids after meals and sucralfate 30 minutes before meals
4. Antacids after meals and sucralfate 30 minutes before meals
Sucralfate is most effective when the pH is low and should not be given with or soon after antacids. Antacids are most effective when taken after eating. Administration of sucralfate 30 minutes before eating and antacids just after eating will ensure that both drugs can be most effective. The other regimens will decrease the effectiveness of the medications.
The home health nurse is caring for a patient who has been receiving interferon therapy for treatment of cancer. Which statement by the patient indicates a need for further assessment?
1. “I have frequent muscle aches and pains.”
2. “I rarely have the energy to get out of bed.”
3. “I experience chills after I inject the interferon.”
4. “I take acetaminophen (Tylenol) every 4 hours.”
2. “I rarely have the energy to get out of bed.”
Fatigue can be a dose-limiting toxicity for use of immunotherapy. Flu-like symptoms, such as muscle aches and chills, are common side effects with interferon use. Patients are advised to use acetaminophen every 4 hours.
A healthy adult woman who weighs 145 lb (66 kg) asks the clinic nurse about the minimum daily requirement for protein. How many grams of protein will the nurse recommend?
1. 53
2. 66
3. 79
4. 98
1. 53
The recommended daily protein intake is 0.8 to 1 g/kg of body weight. Therefore, the minimum for this patient is 66 kg 0.8 g = 52.8 or 53 g/day.
A patient who had a subtotal thyroidectomy earlier today develops laryngeal stridor and a cramp in the right hand upon returning to the surgical nursing unit. Which collaborative action will the nurse anticipate next?
1. Plan for emergency tracheostomy.
2. Administer IV calcium gluconate.
3. Prepare for endotracheal intubation.
4. Begin thyroid hormone replacement.
2. Administer IV calcium gluconate
The patient‘s clinical manifestations of stridor and cramping are consistent with tetany caused by hypocalcemia resulting from damage to the parathyroid glands during surgery. Endotracheal intubation or tracheostomy may be needed if the calcium does not resolve the stridor. Thyroid hormone replacement may be needed eventually but will not improve the symptoms of hypocalcemia.
The nurse calls security and has physical restraints applied when a client who is admitted voluntarily becomes both physically and verbally abusive while demanding to be discharged from the hospital. Which represents the possible legal ramifications for the nurse associated with these interventions? Select all that apply.
1. Libel
2. Battery
3. Assault
4. Slander
5. False Imprisonment
2, 3, and 5: Battery, Assault, and False Imprisonment
Battery is the intentional act of causing physical harm to someone. Unlike assault, one doesn’t have to warn the victim or make him fearful before hurting them for it to count as a battery. Assault and battery are related to the act of restraining the patient in a situation that did not meet the criteria for such an intervention. If the mental health professional evaluates the patient and feels that he/she is at risk of harm to self/others or unable to care for self, the mental health professional can convert the admission to involuntary admission. A false imprisonment is an act with the intent to confine a person to a specific area. The nurse can be charged with false imprisonment if the nurse prohibits a patient from leaving the hospital if the patient has been admitted voluntarily and if no agency or legal policies exist for detaining the patient.
Option 1: Libel is the publication of writing, pictures, cartoons, or any other medium that exposes a person to public hatred, shame, disgrace, or ridicule, or induce an ill opinion of a person, and are not true.
Option 4: Slander is not applicable here since the nurse did not verbally make untrue statements about the patient. If the patient later requests discharge, the hospital can hold the patient on the unit for up to 72 hours until a mental health professional can evaluate the patient for safety concerns. The patient will be discharged if the evaluating mental health professional determines that the patient is safe for discharge.
Which menu choice by the patient who is receiving hemodialysis indicates that the nurse‘s teaching has been successful?
1. Split-pea soup, English muffin, and nonfat milk
2. Poached eggs, whole-wheat toast, and apple juice
3. Oatmeal with cream, half a banana, and herbal tea
4. Cheese sandwich, tomato soup, and cranberry juice
2. Poached eggs, whole-wheat toast, and apple juice
Poached eggs would provide high-quality protein, and apple juice is low in potassium. Cheese is high in sodium and phosphate, and tomato soup is high in potassium. Split-pea soup is high in potassium, and dairy products are high in phosphate. Bananas are high in potassium, and cream is high in phosphate.
Which information will the nurse include when teaching a patient how to avoid chronic constipation? (Select all that apply.)
1. Stimulant and saline laxatives can be used regularly.
2. Bulk-forming laxatives are an excellent source of fiber.
3. Walking or cycling frequently will help bowel motility.
4. A good time for a bowel movement may be after breakfast.
5. Some over-the-counter (OTC) medications cause constipation.
2,3,4,5
2. Bulk-forming laxatives are an excellent source of fiber.
3. Walking or cycling frequently will help bowel motility.
4. A good time for a bowel movement may be after breakfast.
5. Some over-the-counter (OTC) medications cause constipation.
Stimulant and saline laxatives should be used infrequently. Use of bulk-forming laxatives, regular early morning timing of defecation, regular exercise, and avoiding many OTC medications will help the patient avoid constipation.
The nurse assesses a patient with non-Hodgkin‘s lymphoma who is receiving an infusion of rituximab (Rituxan). Which assessment finding would require the most rapid action by the nurse?
1. Shortness of breath
2. Shivering and chills
3. Muscle aches and pains
4. Temperature of 100.2Fo (37.9Co)
1. Shortness of breath
Rituximab (Rituxan) is a monoclonal antibody. Shortness of breath should be investigated rapidly because anaphylaxis or capillary leak syndrome are possible reactions to monoclonal antibody administration. The nurse will need to rapidly take actions such as stopping the infusion, assessing the patient further, and notifying the health care provider. The other findings will also require action by the nurse but are not indicative of life-threatening complications.
Which patients would the nurse refer to the dietitian for a complete nutritional assessment? (Select all that apply.)
1. A 35-yr-old patient who reports intermittent nausea for the past 2 days
2. A 48-yr-old patient with rheumatoid arthritis who takes prednisone daily
3. A 23-yr-old patient who has a history of fluctuating weight gains and losses
4. A 64-yr-old patient who is admitted for debridement of an infected surgical wound
5. A 52-yr-old patient admitted with chest pain and possible myocardial infarction (MI)
2, 3, and 4
A 48-yr-old patient with rheumatoid arthritis who takes prednisone daily
A 23-yr-old patient who has a history of fluctuating weight gains and losses
A 64-yr-old patient who is admitted for debridement of an infected surgical wound
Weight fluctuations, use of corticosteroids, and draining or infected wounds all suggest that the patient may be at risk for malnutrition. Patients with chest pain or MI are not usually poorly nourished. Although vomiting that lasts 5 days places a patient at risk, nausea that has persisted for 2 days does not always indicate poor nutritional status or risk for health problems caused by poor nutrition.
After obtaining the information shown in the accompanying figure regarding a patient with Addison‘s disease, which prescribed action will the nurse take first?
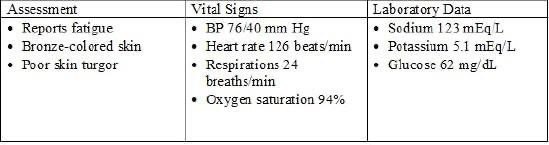
1. Give 4 oz of fruit juice orally.
2. Recheck the blood glucose level.
3. Administer O2 therapy as needed.
4. Infuse 5% dextrose and 0.9% saline.
4. Infuse 5% dextrose and 0.9% saline.
The patient‘s poor skin turgor, hypotension, and hyponatremia indicate an Addisonian crisis. Immediate correction of the hypovolemia and hyponatremia is needed. The other actions may also be needed but are not the most crucial action for maintaining perfusion in the patient.