Name the three findings that make up Charcot’s triad and the pathology it suggests?
2x point bonus: what additional findings would be present in Reynolds pentad?
Charcot’s triad RUQ pain, Fever, Jaundice suggests acute cholangitis
Reynolds pentad includes hypotension + altered mental status
Indicates a more severe version of acute cholangitis
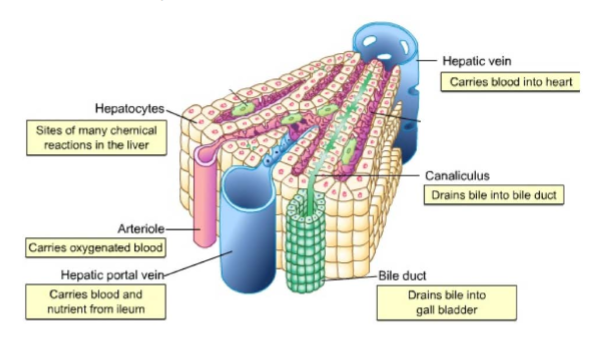
Draw and label the route bile takes from hepatocyte to duodenum, naming five distinct structures along the way.
Which of the following hormones is responsible for stimulating gallbladder contraction and bile release into the duodenum after a fatty meal?
A. Secretin
B. Gastrin
C. Cholecystokinin (CCK)
D. Glucagon
Answer: C. Cholecystokinin (CCK)
Explanation: CCK is released in response to fatty acids in the duodenum and stimulates gallbladder contraction and pancreatic enzyme secretion.
A 56-year-old woman presents with severe epigastric pain radiating to the back, nausea, and vomiting. She has a history of gallstones and hyperlipidemia. On exam, she has epigastric tenderness without rebound or guarding. Serum lipase is markedly elevated. She is diagnosed with acute pancreatitis.
Abdominal ultrasound is ordered to evaluate the cause of her condition. If gallstones are responsible for her pancreatitis, where would you expect to visualize the obstructing stone on imaging?
A) Within the body of the pancreas
B) In the fundus of the gallbladder
C) In the common bile duct near the ampulla of Vater
D) In the cystic duct
E) Intrahepatic bile ducts
C) In the common bile duct near the ampulla of Vater
Gallstone pancreatitis occurs when a gallstone migrates from the gallbladder and becomes lodged in the distal common bile duct, near the ampulla of Vater, obstructing the outflow of both bile and pancreatic enzymes.
This leads to backup of pancreatic secretions, causing inflammation of the pancreas.
The best initial imaging is right upper quadrant ultrasound, which may show:
Gallstones in the gallbladder
Dilated common bile duct
Occasionally, a stone in the common bile duct (CBD)
Describe the difference between an ERCP and a cholecystectomy.
A cholecystectomy is surgery that removes the entire gall-bladder preventing new stones and future attacks.
ERCP is an endoscopic procedure that threads a scope through the mouth into the duodenum, enters the bile duct, and clears obstructions or places stents inside the ducts.
Generally, ERCP is used first when a stone or infection is already blocking the common bile duct and cholecystectomy is done afterward to eliminate the source of stones altogether.
On the board, list four acute and four chronic etiologies for RUQ ± epigastric pain
Acute RUQ
Acute Cholecystitis, Cholangitis, Hepatitis, Hepatic abscess
Acute epigastric
Acute Pancreatitis, Peptic Ulcer Disease, Myocardial Infarction
Chronic RUQ
Chronic Cholecystitis, Chronic Hepatitis B/C
Chronic epigastric
Chronic Pancreatitis, Functional Dyspepsia/GERD
Label
2x point bonus: Describe where the sphincter of Oddi and ampulla of Vater are located?
The ampulla of Vater is where the bile and pancreatic ducts merge within the duodenal wall and is surrounded by the sphincter of Oddi. Secretions exit through the major duodenal papilla the little bump in the duodenum
A 44-year-old woman presents with RUQ pain, fever, and a positive Murphy’s sign. Imaging confirms acute cholecystitis. What is the pathophysiological event that most likely triggered the inflammatory response in acute cholecystitis?
A. Direct infection of the gallbladder wall by E. coli
B. Perforation of the gallbladder into the peritoneal cavity
C. Immune-mediated destruction of the biliary epithelium
D. Obstruction of the cystic duct by a gallstone
Answer: D. Obstruction of the cystic duct by a gallstone
Explanation: The most common cause of acute cholecystitis is cystic duct obstruction by a stone, leading to bile accumulation, distention, and subsequent inflammation of the gallbladder wall.
A 44-year-old man comes to the ED with abdominal pain and nausea for the past 24 hours. The pain started a few hours after dinner, and he describes it as a constant upper abdominal pain that radiates to his back and flanks. He also reports nausea, vomiting, and abdominal distention. Family history is significant for recurrent episodes of pancreatitis in his father and paternal uncle. He reports drinking an average of 2 alcoholic drinks per week. His temperature is (99.9ºF), pulse is 92/min, respirations are 20/min, oxygen saturation is 96%, and blood pressure is 149/94 mmHg. He appears distressed and anxious. Examination shows tenderness and rigidity over the epigastric and periumbilical regions. Bowel sounds are diminished. No bruising of the umbilicus or flanks are seen. Which of the following laboratory results is the most specific in diagnosing this patient’s condition?
A. Serum amylase > 3 times the upper limit of normal
B. Serum lipase > 3 times the upper limit of normal
C. Serum bilirubin > 4.0 mg/dL
D. Elevated blood alcohol level
E. Blood urea nitrogen level > 22 mg/dL
B. Serum lipase > 3 times the upper limit of normal
To make a diagnosis of acute pancreatitis (from any cause), one needs 2 out of 3 of the following criteria:
clinical symptoms, such as persistent, severe, epigastric pain with tenderness on palpation
laboratory studies demonstrating serum amylase or lipase greater than 3 times the upper limit of normal; lipase remains elevated for a longer period of time and has a higher specificity as compared with amylase
imaging (computed tomography, magnetic resonance (MR), ultrasonography) showing focal or diffuse enlargement of the pancreas
A 50-year-old woman presents for a routine postoperative follow-up one month after undergoing a laparoscopic cholecystectomy for symptomatic gallstones. She reports that her abdominal pain has resolved, but she occasionally experiences bloating and loose stools after eating large, fatty meals. She is concerned about how her digestion has changed since surgery and asks if her liver still produces bile.
Which of the following best explains her symptoms and bile physiology after gallbladder removal?
A. The liver no longer produces bile, resulting in fat malabsorption
B. Bile is secreted continuously into the duodenum, even in the absence of food
C. The pancreas compensates for lost bile by increasing lipase production
D. Bile secretion occurs only in response to cholecystokinin (CCK)
E. Chyme passes directly into the colon without mixing with bile
Normal Physiology (Before Cholecystectomy):
The liver continuously produces bile, which is sent through the hepatic ducts.
In the presence of a gallbladder, bile is stored and concentrated there between meals.
When a fatty meal is ingested, cholecystokinin (CCK) is released by the duodenum → this triggers gallbladder contraction and bile release into the duodenum to help emulsify fats.
After Cholecystectomy:
Bile is still produced by the liver, but without the gallbladder it’s no longer stored or concentrated.
It instead flows continuously from the liver through the common bile duct into the duodenum regardless of whether food is present.
This may lead to less efficient fat digestion, especially after fatty meals, which could lead to bloating and mild steatorrhea
Takeaway:
Patients without a gallbladder do not stop producing bile, but lose the ability to release large, concentrated amounts when needed. Advising patients to eat smaller, low-fat meals more frequently can help prevent symptoms post-cholecystectomy. Over time, the biliary system and intestine adapt to this continuous flow, and most people have minimal to no symptoms long-term.
Matching
1. AST/ALT > 1000 IU/L
2. Dilated common bile duct on US
3. Calcifications in the pancreatic head on CT
4. Thickened gallbladder wall, + Murphy
A. Chronic pancreatitis B. Viral hepatitis C. Acute cholecystitis D. Choledocholithiasis
1. B. Viral hepatitis
2. D. Choledocholithiasis.
3. A. Chronic pancreatitis
4. C. Acute cholecystitis
Pair each duct obstruction site with its clinical association, some may have more than one answer, not all answers may be used.
1. Cystic duct
2. Common bile duct
3. Ampulla of Vater
4. Ileo-cecal valve
A. Rigler triad B. Acute pancreatitis C. Biliary colic D. Charcot’s triad E. cholecystitis F. Reynold’s pentad G. Mcburney's sign H. Murphy’s sign I. air in the biliary tree J. Mcdonald's sign
Cystic duct → C. E. H.
Common bile duct → D. F.
Ampulla of Vater →B.
Ileo-cecal valve → A. I.
G. J. not used
A 39-year-old woman comes to the clinic complaining of recurrent RUQ pain for the past several months. She describes the pain as sharp and cramping, occurring mostly after meals, especially when she eats fried or greasy foods. The pain usually lasts about 30–60 minutes and then subsides on its own. She denies fever, jaundice, vomiting, or changes in bowel movements. Her BMI is 34, and she has had three pregnancies. Murphy’s sign is negative. Ultrasound reveals the presence of gallstones.
Which of the following is the most likely diagnosis?
A. Acute cholecystitis
B. Choledocholithiasis
C. Symptomatic cholelithiasis (biliary colic)
D. Ascending cholangitis
Answer: B. Symptomatic cholelithiasis (biliary colic)
Explanation: Biliary colic refers to an acute pain that occurs due to temporary obstruction of the gallbladder outlet or cystic duct. It typically presents with RUQ pain lasting <6 hrs that can be triggered by fatty meals which stimulate CCK production, leading to gallbladder contraction against the blocking stone. No systemic signs of infection or inflammation are present.
A 56-year-old woman presents with severe epigastric pain, nausea, and vomiting. Her labs reveal a lipase level elevated to 8x the upper limit of normal. Vital signs are stable, and her abdominal exam is consistent with pancreatitis. Which of the following is the most appropriate next step in management?
A. Order contrast-enhanced CT abdomen to confirm diagnosis
B. Perform endoscopic retrograde cholangiopancreatography (ERCP)
C. Begin supportive care without imaging
D. Order abdominal ultrasound to evaluate for pancreatic necrosis
E. Order MRI abdomen with MRCP
C. Begin supportive care without imaging
In a patient with classic clinical presentation and lipase >3x ULN, imaging is not required to diagnose pancreatitis. Supportive care should be initiated immediately. CT is reserved for unclear cases or if the patient does not improve after 48–72 hours.
A 47-year-old woman presents to her primary care provider for follow-up after an abdominal ultrasound revealed multiple small, non-calcified gallstones. She has mild intermittent right upper quadrant discomfort after meals but declines surgical intervention. She is started on a medication that is commonly used in patients with cholesterol gallstones who are not candidates for surgery. This medication improves gallbladder emptying, decreases intestinal absorption of cholesterol, and promotes dissolution of stones by increasing the solubility of bile components.
Which of the following describes the mechanism of action of the medication prescribed?
A. Inhibits HMG-CoA reductase to reduce bile cholesterol
B. Disrupts bile acid reabsorption in the terminal ileum
C. Solubilizes cholesterol in bile and reduces hepatic cholesterol secretion
D. Stimulates gallbladder contraction by activating CCK receptors
E. Inhibits enterohepatic circulation of bile salts
C. Solubilizes cholesterol in bile and reduces hepatic cholesterol secretion
The drug described is ursodeoxycholic acid, which works by solubilizing cholesterol in bile, thereby promoting gallstone dissolution. It also reduces cholesterol absorption and hepatic secretion, improving bile flow and gallbladder function.
A 52-year-old man with a 20-year history of drug and alcohol use presents with weight loss and a dull pain in his upper abdomen and back. The pt states he is currently sexually active with multiple partners. HBsAb: reactive
Ultrasound: homogeneous liver with well-defined borders, patent intrahepatic and extrahepatic biliary ducts, pancreas normal size, shape with hyperechoic foci
Which diagnosis best explains this clinical picture?
A. Chronic calculous cholecystitis
B. Chronic pancreatitis
C. Functional dyspepsia / GERD
D. Chronic viral hepatitis B
B. Chronic pancreatitis, epigastric-to-back pain, steatorrhea, weight loss, and pancreatic calcifications on imaging are the classic triad of chronic pancreatitis
A 48-year-old woman with chronic cholelithiasis develops worsening jaundice and pruritus. Ultrasound shows a 2-cm stone impacted in the cystic duct. The intrahepatic ducts and common hepatic duct are dilated, but the distal common bile duct is normal size and stone-free.
Which structure is responsible for the worsening symptoms
A. Cystic duct
B. Common hepatic duct
C. Common Bile duct
D. Right hepatic duct
B. Common hepatic duct In Mirizzi syndrome a cystic-duct stone sits directly beside and compresses the common hepatic duct, producing upstream dilation while the distal CBD remains normal.
You’re at your LIC clinic, and your preceptor asks you to evaluate a 56-year-old woman who presents with a 2-day history of RUQ pain, fever, nausea, and vomiting. You respond, “Sure! I’m actually in GI right now and look forward to seeing what’s going on with this patient.”
Your preceptor gets excited and says, “That’s great! Feel free to do a focused physical exam if you’d like.”
You have several differentials in mind at this point.
Demonstrate and describe the physical exam maneuver you would perform next to narrow your differential. What constitutes a positive result, and what diagnosis would this suggest?
Murphy’s sign is a clinical test used during a physical exam to assess for gallbladder inflammation. A positive Murphy’s sign is a hallmark physical exam finding in acute cholecystitis and can help distinguish it from other causes of RUQ pain.
How to Perform It:
Ask the patient to exhale completely.
Palpate just under the right costal margin
Ask the patient to take a deep breath in.
If patient suddenly stops inhaling midway due to sharp RUQ pain -> Positive Murphy's Sign
Why Does This Happen?
During inspiration, the diaphragm descends, pushing the inflamed gallbladder down into the examiner’s palpating hand
In acute cholecystitis, the inflamed gallbladder is hypersensitive to touch.
As it contacts the examiner’s hand, it triggers sharp localized pain, causing the patient to reflexively stop inhaling.
At her 3rd day in the hospital a woman with gallstone pancreatitis is found to have the following: lipase 600 U/L, WBC 16,000/µL, creatinine elevated, bicarbonate 21 mmol/L, O₂ sat 92%, and hypotension (BP 92/50 mmHg). According to the Revised Atlanta Classification, what is the severity of her pancreatitis and why?
Correct Answer: Severe acute pancreatitis
According to the Revised Atlanta Classification, acute pancreatitis is categorized into three severity levels based on the presence and duration of organ failure and local/systemic complications:
Severity Grading of Acute Pancreatitis (Based on Revised Atlanta Classification)
Mild: No organ failure. No complications.
Moderately Severe: Transient organ failure < 48 hrs and/or local/systemic complications
Severe: Persistent organ failure > 48 hrs (respiratory, renal, or cardiovascular)
In this case, the patient shows signs of organ failure:
Hypotension (BP 92/50 mmHg) suggests cardiovascular failure
Elevated creatinine suggests renal involvement
Low oxygen saturation (92%) suggests respiratory compromise
A 56-year-old woman presents for a routine follow-up. She was recently hospitalized for acute gallstone pancreatitis. She has a history of obesity (BMI 33 kg/m²), hypertension, and osteoarthritis. She reports often eating at fast food restaurants due to her busy work schedule and struggles to find time for physical activity. She expresses interest in making dietary and lifestyle changes to prevent recurrence of gallstone-related issues.
Which of the following is the most appropriate lifestyle counseling for this patient to reduce her risk of gallstone formation?
A) Recommend a ketogenic diet with intermittent fasting for rapid weight loss
B) Encourage three balanced meals daily that are high in fiber, calcium, and low in saturated fats
C) Suggest skipping breakfast to reduce caloric intake and promote weight loss
D) Advise a high-protein, low-carbohydrate diet with daily saturated fat intake
E) Recommend rapid weight loss of >2.5 kg per month to minimize gallbladder sludge
B) Encourage three balanced meals daily that are high in fiber, calcium, and low in saturated fats
Patients at risk of gallstone disease, particularly those who are overweight or obese, benefit from gradual weight loss, regular meal schedules, and a diet low in saturated fat, high in fiber, and high in calcium.
Skipping meals or undergoing rapid weight loss can increase the risk of gallstone formation due to gallbladder stasis and changes in bile composition. High fat diets like the keto diet can also increase the likelihood for gallstone development.
A 29-year-old man presents with dull RUQ discomfort, fatigue, low-grade fever, and tea-colored urine. Pt states the symptoms started yesterday.
Exam: Erythematous fluctuant mass at right cubital fossa, mild icterus, Murphy sign negative.
Labs: AST 2300 U/L, ALT 2600 U/L, ALP 170 U/L, Total Bilirubin 3.4 mg/dL, INR 1.4.
Ultrasound is unremarkable
What is the most likely diagnosis?
A. Acute viral hepatitis
B. Acute cholecystitis
C. Choledocholithiasis with ascending cholangitis
D. Acute alcoholic hepatitis
A. Acute viral hepatitis, The AST/ALT values in the thousands, recent IV-drug exposure (erythematous mass), and a normal gallbladder/ductal ultrasound point to an acute viral hepatitis rather than biliary disease. Acute cholecystitis would give a positive Murphy sign with only mild transaminase increase; ascending cholangitis would raise alkaline phosphatase and direct bilirubin more and show ductal dilation. Alcoholic hepatitis keeps an AST: ALT ratio of 2:1
A 55-year-old woman with a history of gallstones is brought to the ED shortly after a fried-seafood dinner with colicky pain in the right upper quadrant. She is afebrile and hemodynamically stable and hasn't noticed any weight change.
Labs: WBC 8200 /µL, Direct bilirubin 3.8 mg/dL, ALP 350 U/L, AST 82 U/L, ALT 88 U/L
Which diagnosis best accounts for this presentation?
A. Cholelithiasis
B. Choledocholithiasis
C. Cholestasis
D. Cholangitis
E. Cholangiocarcinoma
B. Choledocholithiasis
↑ direct bilirubin and ALP with colicky RUQ pain but no fever and normal WBC and weight
List and explain the four classic risk factors ("Four Fs") for cholesterol gallstone formation. For each factor, briefly describe how it contributes to gallstone development.
Female
Estrogen increases cholesterol secretion into bile and reduces bile acid secretion, leading to supersaturation of bile with cholesterol — a key step in cholesterol stone formation.
Fat (Obesity)
Increased body weight is associated with higher cholesterol production and secretion into bile. Obesity also slows gallbladder motility, promoting bile stasis and stone nucleation.
Forty
Aging is associated with a natural decline in 7-alpha-hydroxylase, the rate-limiting enzyme in bile acid synthesis. Less bile acid means less solubilization of cholesterol, increasing the risk of crystallization.
Fertile (Pregnancy)
Progesterone reduces gallbladder contractility, promoting bile stasis. Estrogen increases cholesterol secretion, contributing to gallstone formation.
A 58-year-old woman named Jane presents to the emergency department with severe epigastric and right upper quadrant pain that radiates to her back. She has a history of symptomatic gallstones, but a cholecystectomy was not performed due to financial constraints.
Calculate Jane’s total Ranson score using the information provided. Based on this score, estimate her mortality risk.

A 64-year-old man presents with RUQ pain, jaundice, and fever. Ultrasound shows a dilated common bile duct and gallstones in the gallbladder. After stabilization, which of the following sequences of procedures is most appropriate?
A. ERCP only
B. Cholecystectomy only
C. ERCP followed by cholecystectomy
D. Cholecystectomy followed by ERCP
E. Observation and pain management
Answer: C. ERCP followed by cholecystectomy
Explanation: In complicated gallstone disease, such as cholangitis, the first step is ERCP to relieve obstruction and infection. This is followed by cholecystectomy to prevent recurrence.