The hallmark tenet of a diagnosis of multiple sclerosis
What is dissemination in space and time?
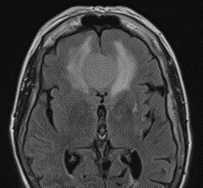
The type of edema seen on this MRI Flair scan of a mass in the right frontal lobe
What is vasogenic edema? Edema in which there is disruption of the blood brain barrier. Extracellular edema, affects white matter due to leakage of fluid from capillaries. On CT scans the grey-white differeniation is maintaind; edema involves white matter. On MRI studies, this shows up as hyperintensity on T2 and FLAIR that does not diffusion restrict
Different from cytotoxic edema in which the blood brain barrier is intact. Most commonly seen in ischemic lesions. Result of intracellular injury--cannot maintain ATP Na/K pumps, Na and Chloride accumulates in the cell and draws water in, cells swell and reduces extracellular volume, affects grey matter and white matter as well. Best seen on diffusion weighted imaging
The neurologist who coined the term asterixis with colleague Raymond Adams in the 1940s.
Who is Joseph Foley. Dr. Foley is the father and founder of the neurological division at University Hospitals; under Dr. Foley he built a division of neurology within the Department of Medicine. Story goes that he consulted a Jesuit Scholar from Boston College. Dr. Foley and Father Cadigan drank metaxa (Greek spirit, a wine with botanicals) and came up with the term an (negative) - iso (equal), and sterixis (solidity of firmness). Anisoterixis was too many syllables, and thus shortened it to asterixis.
The percentage of patients with generalized myasthenia gravis that are AchR positive?
The percentage of patients with generalized myasthenia gravis that are AchR positive?
What vessel size type is affected in giant cell arteritis? (i.e. small, medium, large....)
What are medium and large sized vessels. In the head and neck, can include superficial temporal artery, occipital artery, post auricular, facial arteries; blood vessels of the eye and optic nerve, vasculitis leading to stroke
The syndrome name for an acquired demyelinating neuropathy charachterized by opthalmoplegia, ataxia and areflexia?
What is Miller-Fisher Syndrome. Associated with ganglioside GQ1b antibody, present in 80% of those with this condition.
Bickerstaff brainstem encephalitis can overlap with some symptoms, also associated with GQ1b, includes altered conciousness, extensor plantar response and hyperreflexia due to CNS involvement.
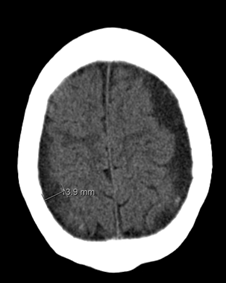
The hematoma seen in this CT Head without contrast is between which two layers?
What are the arachnoid and dura mater? Seen on this study are bilateral subdural hematomas. Blood collects between the dura and the arachnoid mater. Risk factors include head injury, atrophy, anticoagulation, CSF leaks, ETOH use, high-impact sports, diabetes mellitus, thrombocytopenia, epilepsy, arachnoid cysts, cardiovascular disease. Annual incidence is 1-5.3 cases per 100,000 population.
The physician who is given credit for describing amyotrophic lateral sclerosis.
Who is Jean-Marie Charcot? Between 1865-1874, he developed an understanding that some individuals developed a progressive weakness where on autopsy there was sclerosis of the lateral fasciculi (lateral corticospinal tract) and atrophy of muscles = amyotrophy. Coined the term amyotrophic lateral sclerosis in 1874.
In some areas of the world ALS is called Charcot's disease.
What is the unique inflammatory pathophysiology of AchR positive myasthenia gravis as compared to MuSK myasthenia gravis? In other words what innate system of the body is triggered by the AcHR antibody docking onto the muscle membrane?
What is the complement system. More specifically the classical pathway.
You will recall there are many Cs in the complement pathway including C1r, C1s, C4, C4, C4a, C5 convertase = C3C4b2a3b.
C3a, C4a, 5a are proinflammatory, increases vascular permeability, smooth muscle contraction and leucocyte recruitment.
C5b eventually helps to form Membrane attack complex, (MAC),
MAC lyses the cell via several mechanisms and causes destruction of the neuromuscular junction.
This is why complement inhibitor medications work well for myasthenia gravis. You inhibit the destruction of the neuromuscular junction by lessening the destruction of the neuromuscular junction.


Name the MRI finding and the reason why this happens?
Empty Sella Syndrome. Occurs when the arachnoid layer of the brain bulges into the sella tursica, and compresses the pituitary. Can be seen in different conditions that lead to increased ICP including IIH.
The demyelinating condition that can often present with a longitudinally extensive spinal cord lesion, aka a severe transverse myelitis
What is NMO or NMO spectrum conditions
What is the type of dementia most commonly associated with ALS?
What is frontotemporal dementia? ALS and FTD are considered a spectrum of diseases.
In some families who have a genetic form of ALS/FTD, some members will have FTD and some ALS which helped lead to this discovery that the conditions are part of the same spectrum.
The syndrome named after the person who spoke these words. "How the theater of the mind could be generated by the machinery of the brain."
What is Charles Bonnet Syndrome. Charles Bonnet, a lawyer with a strong hobby in studying natural science, described this condition based on observations of his own 87 year old grandfather, who had vision loss due to cataracts.
A simplistic explanation of Charles Bonnet Syndrome is that as vision is lost, the visual system cannot process new images correctly. However the visual processing portions of the brain are still working and will create visual hallucinations.
Patients with AchR positive generalized myasthenia gravis who are more difficult to control and require long term immunosuppression will obtain a thymectomy. What is the most common histopathological diagnosis of the removed thymus tissue?
What is thymic hyperplasia?
About 65%-70% of AchR positive MG patients have thymic follicular hyperplasia.
About 10%-15% of AcHR positive MG patients have a thymoma.
Overall for many patients, they will need less immunosuppression post-thymectomy than without thymectomy. Some will even achieve remission.
The most common cause of papilledema.
What is IIH. Affects 1 in 100K, 20X more likely in women of childbearing age
The brain region that if hurt can be involved in severe nausea, can be preferentially involved in NMO
What is the area postrema
What type of brain cell is the target of the condition that is most likely represented by the below images? 
What are astrocytes. Inflammation in NMO spectrum disorders primarily seem to target astrocytes. AQP4 is a water channel that is present in the foot processes of astrocytes. It is concentrated in the spinal cord gray mater, periaqueductal and periventrical areas.
The "classic" name of a rapidly progressive neurodegenerative condition, caused by the abnormal isoform of prion protein
What is Creutzfeldt-Jakob disease (CJD). In the US it is estimated to be one case per million. Most will die within 1 year of onset of symptoms. In about 85% of cases, this occurs as sporadic disease without any family history or known genetics. In about 5-15% they develop CJD due to mutations in the prior protein gene. The disease was first described in the 1920s by the German neurologists Hans Gerhard Creutzfeldt and Alfons Maria Jakob.
Clues towards this diagnosis can be a rapidly progressive neurodegenerative condition, startle myoclonus, periodic sharp waves on EEG.
To diagnose, testing is done of CSF fluid and through the national prion center which is outside the door of our adult EMU, they arrange for autopsies to confirm tissue diagnosis.
We are careful not to confuse classic CJD with variant CJD. Variant CJD initially described in 1996 in the UK, with strong evidence supporting that the agent responsible for prion disease in cows (Mad Cow disease) is the same agent responsible for vCJD in humans.
The Greek/Latin translation of the condition myasthenia gravis?
mys--muscle
Asthenia--weakness
Gravis--severe
What is Grave muscle weakness or severe muscle weakness?
The percent range of those with GCA have PMR?
What is about 60% (58%). PMR affects proximal, axial joints, with elevated ESR as well. Responds to low dose steroids. PMR prevalence is 1 in 133. ~ 15-20% with PMR develop GCA. ~ 60% of individuals with GCA, have PMR.
A chronic motor only demyelinating acquired condition that involves classically conduction blocks that can be asymmetric in presentation
What is Multifocal Motor Neuropathy
The percentage of patients with NMDA encephalitis that make a substantial neurological recovery?
~ 80% in a trial following a large cohort of patients for 24 months. Recovery can take up to 2 years to achieve. Reviewed 577 patients.
Treating with second line rituximab or cyclophosphamide improved outcomes for those that did not respond to first-line and decreased frequency of relapses.
What is the eponym of JC Virus? Aka..what is the full name of JC?
Who is John Cunningham? JC virus is also known as human polyomavirus 2. Virus was named after the patient in whom this virus was first identified in 1971.
The below is a picture of repetitive stimulation. This is an EMG test commonly used to evaluate for neuromuscular junction disorders such as myasthenia gravis. What is the reason for the classic "U" shaped seen as is the case below? In other words, why does the amplitude increase again at the 4th or 5th shock in a particular train?
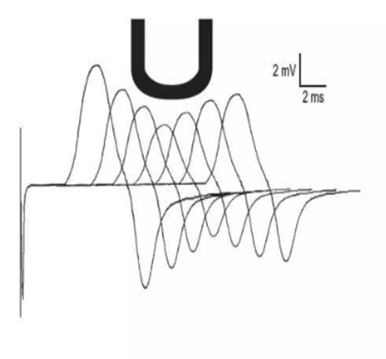
What is the axon utilizing the secondary or mobilization store of Acetycholine?
Acetylcholine is stored as a primary, secondary and tertiary storage in the nerve.
Primary--beneath the pre-synpatic nerve terminal membrane
Secondary--located toward the axon, starts to replenish the immediately available store after 1-2 seconds of rep stim and is responsible for the classic U-shaped of rep stim where the amplitude increased again after the 4th or 5th shock.
Tertiary store--also available in the axon and cell body.
The most common opthalmic manifestation of systemic sarcoidosis?
What is anterior uveitis. The exact incidence is widely variable depending on studies, some citing 10-50%.