There are Four natural areas of narrowing where most foreign bodies become entrapped in the esophagus, what are they and what vertebrae facing it?
Cricopharyngeous muscle C6
Aortic Arch T4
Left Mainstem Bronchus T5
Lower Esophageal Sphincter at Diaphragmatic Hiatus T10 or T11
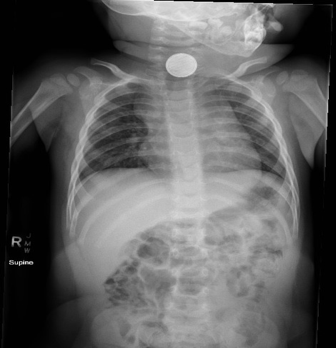
Scleral icterus becomes clinically apparent at approximately which serum bilirubin level?
(A)2 mg/dL
(B)2.5 mg/dL
(C)3 mg/dL
(D)3.5 mg/dL
Icterus is often first noted in the sublingual or subungual areas when the serum bilirubin level is above approximately 2.5 mg/dL.
Which of the following statements regarding acute pancreatitis is true?
(A)Esophageal ultrasound is the diagnostic imaging of modality of choice for the diagnosis of acute pancreatitis.
(B)Hypertriglyceridemia is the likely etiology of acute pancreatitis in those with serum triglyceride levels greater than 1000 mg/dL.
(C)The most common cause of acute pancreatitis is alcohol abuse.
(D)Acute pancreatitis is the most lethal pancreatic disease globally.
(B) Serum triglyceride levels greater than 1000 mg/dL with no other clear causes of acute pancreatitis points to hypertriglyceridemia as the etiology. Imaging is not routinely recommended in the diagnosis of acute pancreatitis. CT is the diagnostic modality of choice; endoscopic ultrasound (EUS) is invasive and not recommended as a first line imaging test.
Although acute pancreatitis is the most common pancreatic disease globally, pancreatic cancer carries the highest mortality. Pancreatic pseudocysts generally form after 4 weeks from symptom onset.
A 70 years old male known case of DM, HTN, CKD presented with history of abdominal pain , vomiting and constipation . Vitals: Temp 37.8 C, HR 110 , BP 140/80 , Oxygen sat 96% , upon assessment abdomen distended , diffuse tenderness but no rebound .
What are the cause of functional SBO?
How to Differentiate between SBO and LBO?
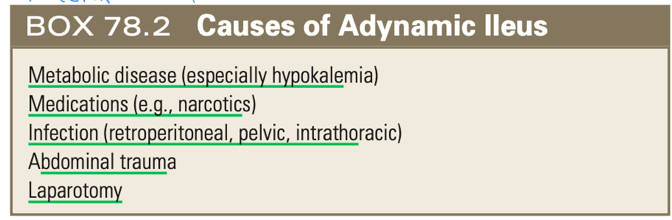
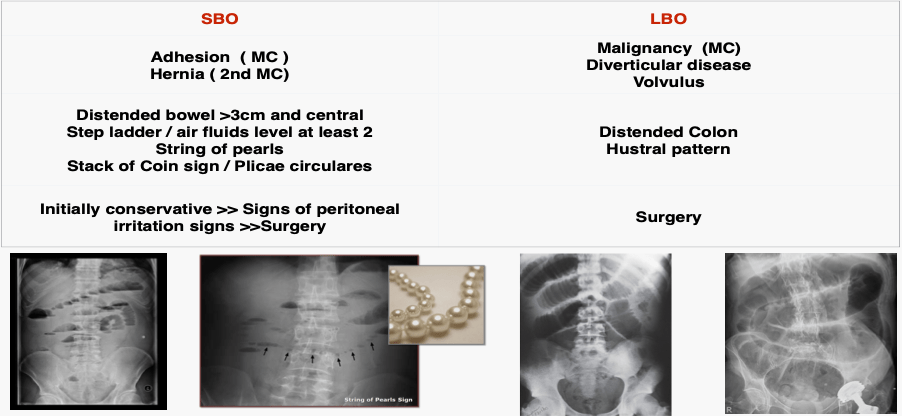
What is the FB? Mention 2 signs in Xray

Button battery
1-Double ring” appearance on PA (most of the time – absence of a double ring does not exclude the diagnosis)
2-“Step off” appearance on lateral view
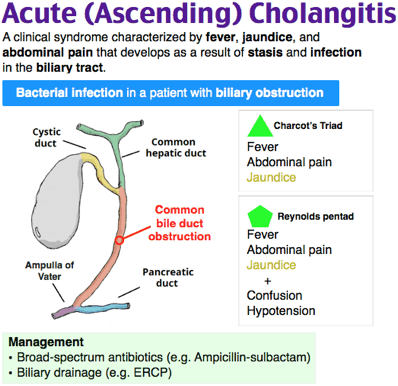
A 75-year-old man presents to the ED with fever and altered mental status. On exam, he appears slightly jaundiced and has right upper quadrant (RUQ) tenderness on palpation with a positive Murphy's sign. Serum lipase is within normal limits, while alkaline phosphatase and total bilirubin are moderately elevated. What is the most likely diagnosis?
(A)Ascending cholangitis
(B)Biliary colic
(C)Cholecystitis
(D)Choledocolithiasis
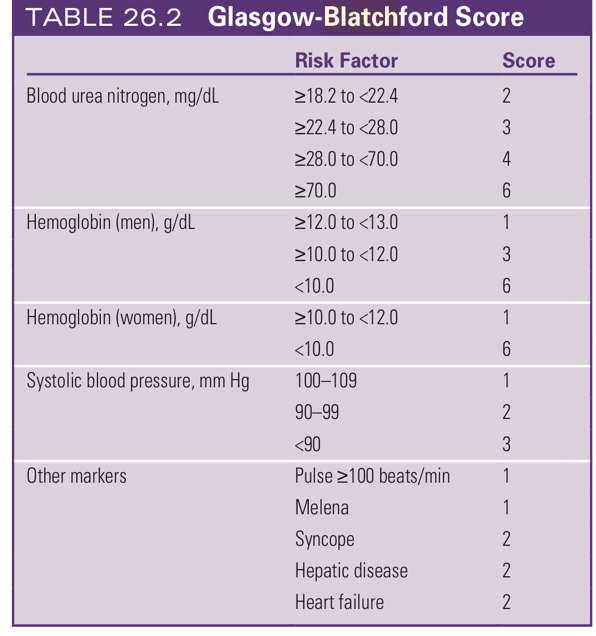
A 42 years old man, medically free presents to the ED after 2 episodes of dark stools in the last week, He has no other complaints, Vitally stable. Rectal exam reveals soft brown stool that is guaiac positive. Otherwise his exam is normal. Laboratory testing indicates a hg of 14 g/dl and BUN 6 mg/dl. Which of the following is the most appropriate next step in the management of this patient?
1- CT scan with contrast
2- Immediate Endoscopy
3- Discharge home with follow up to a Gastroenterologist
4- Placement of NGT for lavage :)
-(3) GBBS of our patient was 0 and he can be safely managed as an outpatient
This patient is concerning for an UGIB.The Glasgow Blatchford bleeding score is a useful tool to use in emergency department to risk stratify such patient and to idenfy those who can be safely discharged from ED and managed as outpatient basis
A score is assigned by assessing the urea, hg , SBP , HR , stool exam and other comorbidities
For low risk patient who are candidate for Outpatient management
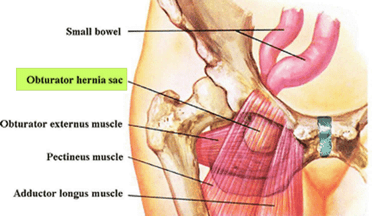
Which of the following patients is at the highest risk of developing an obturator hernia?
(A)2-year-old boy with no known medical problems
(B)45-year-old woman with a 1year history of hysterectomy
(C)67-year-old man with a history of metastatic prostate cancer
(D)80-year-old woman with a 3month history of rapid weight loss
(D) This type of hernia is especially common in older women who have recently lost a significant amount of weight. The female pelvis is wider, and the obturator canal is more oblique in women. This, in combination with a loss of preperitoneal fat, predisposes to its development. Because an external mass is absent, diagnosis is especially challenging and explains why it carries the highest mortality of any abdominal hernia nearly 70% when incarcerated.
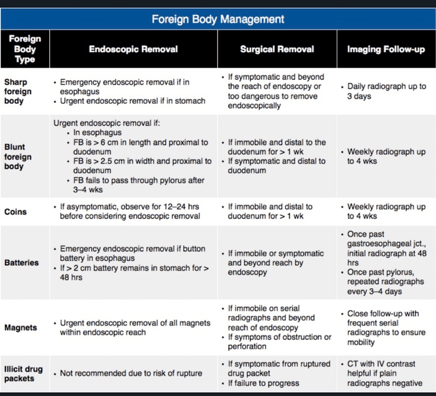
Surgical removal should be considered for objects that remain in the stomach for more than____ to ______or that remain in the same intestinal location for more than ____ .
Surgical removal should be considered for objects that remain in the stomach for more than 3 to 4 weeks or that remain in the same intestinal location for more than 1 week.
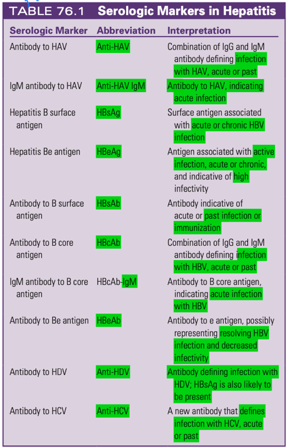
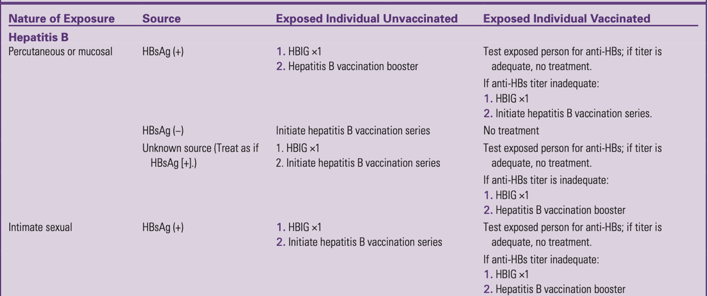
A high school student interested in nursing is observing an emergency medicine nurse at work. During the shadowing experience, she handles medical equipment without permission, and she is inadvertently exposed percutaneous from a needle used to draw blood in a patient with reported hepatitis B virus (HBV) infection. The student does not know her vaccination status, but she receives yearly medical care from a pediatrician.
Which of the following is the best next step in management of the student’s exposure?
A) Test the patient for hepatitis B surface antigen (HBsAg).
B) Administer the HBV vaccine.
C) Test the student for hepatitis B surface antibody (HBsAb).
D) Administer hepatitis B immunoglobulin (HBIG).
-(C) Vaccination is highly effective in the prevention of HBV infection.
A positive HBsAb confirms prior immunization among individuals with an unclear vaccination history
A 27-year-old woman presents to you for evaluation of sudden-onset epigastric pain radiating to the back. She has a history of symptomatic cholelithiasis, and she tells you that she has a surgical appointment scheduled in a few weeks. She felt fine until 12 hours prior to her presentation, which is when she says she developed sudden pain. She denies fevers, diarrhea, or dysuria. She is mildly nauseous and is not taking anything by mouth, but she has not vomited.
On examination, she appears uncomfortable but otherwise Vitally Stable .Her abdomen is soft, nondistended, and moderately tender to palpation in the epigastrium with voluntary guarding.
Laboratory values are notable for a lipase of 1000 U/L. Liver function test results are normal.
You plan to admit the patient for intravenous fluids, observation, and serial exams; however, her admission is delayed.
Which of the following is the most appropriate initial oral intake strategy for this patient while she is awaiting admission?
1- Clear liquids as tolerated
2- Nothing by mouth
3- Low-fat diet as tolerated
4- Nasogastric tube decompression and nothing by mouth
(3) Enteral nutrition should not be withheld in acute pancreatitis, because, in fact, newer studies show that food by mouth may be therapeutic.
Traditional management of pancreatitis included restriction of oral intake to avoid stimulation of pancreatic secretion that could worsen inflammation. However, data over the past 20 years, indicate no adverse effects from continued oral or enteral feeding in pancreatitis, and, in fact, have shown an increased risk of bacterial translocation from the gastrointestinal tract when patients are kept as "nothing by mouth” (NPO).
In this patient, who has mild pancreatitis and nausea, the most appropriate option is to offer her a low-fat diet as she can tolerate while waiting for admission
A 55year-old woman with a history of Roux-en-Y gastric bypass surgery presents with one day of worsening colicky abdominal pain and vomiting. A CT scan reveals an internal hernia. What is the most appropriate disposition?
A- Administer broad spectrum antibiotics and admit to the medicine floor.
B- Arrange for barium swallow with small bowel follow- through.
C- Insert nasogastric tube and admit to the medicine floor.
D- Prompt surgical consultation and preparation for surgery.
(D) Although rare in the general population, internal hernias are a recognized complication of bariatric surgery, especially when a Roux-en-Y type procedure has been performed. Because of the closed loop nature of an internal hernia, they are not suit able for conservative management and require surgical intervention.
72-year-old man with hypertension, hyperlipidemia, and with 1 day of dysphagia. He is accompanied by his son, who provides you with most of the history because the patient is hoarse and is having difficulty speaking. For the past 24 hours he has been unable to ingest either solid food or liquids without coughing and drooling.
Based on his history, which of the following is highest on the differential diagnosis for this patient’s dysphagia?
- Myasthenia gravis
- Stroke
- Polymyositis
- Achalasia
2-Strokes
Vertebrobasilar stroke are the most common neuromuscular cause of dysphagia, and they are highest on the differential diagnosis in this patient, because he presents with sudden symptoms accompanied by dysarthria and hoarseness concerning for additional cranial nerve deficits.
Polymyositis, dermatomyositis, and myasthenia gravis are additional neuromuscular causes, but they present with more progressive symptoms.
A 39year old man presents with a 4-day history of abdominal pain and nausea. He has no significant past history and takes no medications. Vital signs include a temperature of 37.7°C (99.9°F) oral,pulse of 98 beats/min, respiratory rate of 20 breaths/min, and a blood pressure of 119/68 mm Hg. The physical examination reveals scleral icterus, a normal cardiopulmonary examination, moderate right upper quadrant tenderness without rebound, and guaiac-negative stool. Laboratory assessment reveals the following:
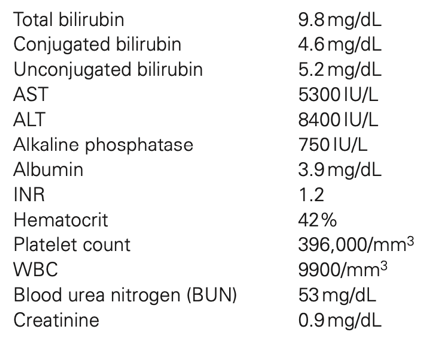
Which of the following courses of action is most appropriate?
(A)Admission for observation and GI consultation
(B)CT scan of the abdomen with contrast
(C)Gastrointestinal (GI) referral for interferon therapy
(D)Reassurance
(A) Altered sensorium and prolongation of the PT beyond 5 seconds or INR beyond 1.5 suggests fulminant hepatic failure. Similarly, an unexplained elevation of the BUN or creatinine level may portend hepatorenal syndrome, which is associated with significant
morbidity. The laboratory derangements warrant admission or transfer for hydration, close observation, and gastroenterology evaluation. Interferon has demonstrated some success in symptomatic hepatitis B patients but does not affect the early course.
A 28-year old woman presents with recurrent pancreatitis. She is otherwise healthy and takes no medications. This episode of pain was preceded by several similar episodes of intermittent epigastric pain that lasted several hours at a time. A previous (4 days) ultrasound examination of the liver, gallbladder, and pancreas was normal. She does not smoke, drink, or use over-the-counter medications. The physical examination
is remarkable for moderate epigastric tenderness without rebound. Vital signs are normal. Laboratory evaluation reveals an elevated lipase level and moderate leukocytosis. Urinalysis and urine pregnancy test
results are normal. What would be the most appropriate intervention?
(A) After stabilization, referral to a gastroenterologist for endoscopic retrograde cholangiopancreatography (ERCP)
(B)After stabilization, referral to a gastroenterologist for upper
endoscopy
(C)CT scan of the abdomen to rule out pancreatic pseudocyst
(D)Repeated ultrasound examination of the liver, gallbladder, and pancreas
(A) Many cases of presumed idiopathic pancreatitis may be due to small stones or sludge that cannot be seen by ultrasound examination but may be seen by ERCP. Pancreatic pseudocyst is more likely in alcoholic pancreatitis and typically occurs gradually, several months after a severe episode.
What predisposing factor increases the risk for adenocarcinoma of the small bowel?
(A)History of Crohn disease
(B)History of ulcerative colitis
(C)Lactose intolerance
(D)Tobacco use
(A) Adenocarcinoma of the small bowel is a rare disease.
Adenocarcinoma of the small bowel is generally a disease of older people. Several factors have been evaluated to determine an increased risk for adenocarcinoma of the small bowel. There is some increased risk in patients who drink alcohol, ingest refined sugar, or consume large amounts of red meat or smoked foods.
However, the most significant associations have been with underlying cystic fibrosis or Crohn disease. The most common presenting symptoms of a small bowel tumor include abdominal pain, nausea and vomiting, weight loss, gastrointestinal bleeding, and intestinal obstruction. Diagnosis is made with computed tomography imaging or endoscopy. Treatment is surgical resection.
A 50-year-old man with a history of hiatal hernia presents complaining of sudden-onset, severe epigastric pain radiating to the left chest and back. He has had multiple episodes of nonbilious, non-bloody emesis followed by nonproductive retching. He also complains of new dyspnea at rest.
At today's visit,his vital signs are: Temp 36.7 °C , HR 110 beats/minute; BP149/90 mm Hg; RR 24 breaths/minute; and O2 sat 95% on room air.
Physical examination is notable for decreased breath sounds over the left chest. Abdominal examination is unremarkable. Findings on electrocardiography are normal.
Upright posteroanterior x ray( Show below).
lateral radiographs of the chest reveal a large, gas-filled loop of hollow viscus in the chest.
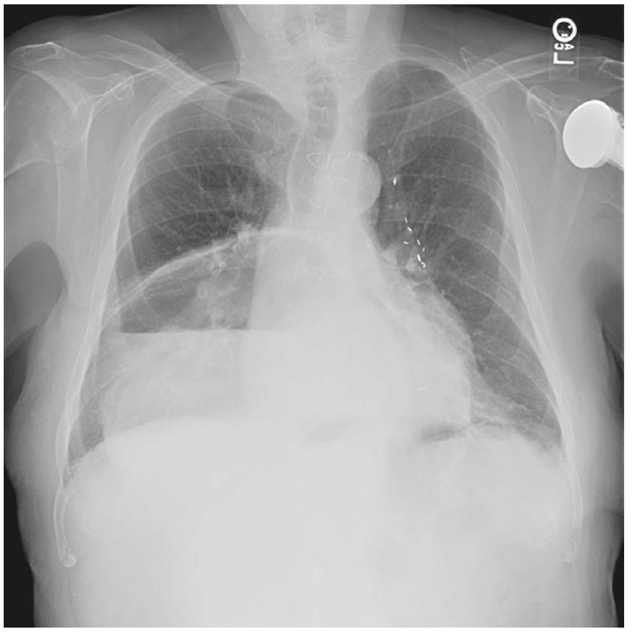
Which of the following is correct regarding this patient’s condition?
- Tube thoracostomy is indicated
- Inability to pass a nasogastric (NG) tube confirm the diagnosis
- Standard of care is nasogastric (NG) tube decompression and serial examinations
- Mortality rate from this diagnosis is low
3- Standard of care is nasogastric (NG) tube decompression and serial examinations
If no signs of gastric infraction pt may underwent Endoscopic reduction with Surgical repair to diaphragmatic deficits
This patient’s history of a diaphragmatic hernia, combined with symptoms of upper abdominal pain radiation to the chest and back, vomiting, and retching, as well as the radiographic findings revealing a loop of bowel in the chest, are concerning for gastric volvulus. then the mortality rate can be as high as 50%. Treatment is surgical, with emergent operative reduction of the volvulus and diaphragmatic hernia repair.
Chest tubes are contraindicated when abdominal contents have herniated above the diaphragm.
A 67-year-old man with poorly controlled, insulin-dependent diabetes presents with 3 days of fever, nausea, and abdominal pain. He reports the pain as constant and localized in the right upper quadrant. Vital signs are: temperature 38.9° C (102 °F), heart rate 110 beats/minute, blood pressure 110/70 mm Hg, respiratory rate 22/minute, and oxygen saturation 95% on room air. His abdomen is soft, but tender to palpation in the right upper quadrant, with a positive Murphy sign.
Laboratory results are notable for a white blood cell count of 22,000/µL and a blood glucose level of 320 mg/dL.
Which of the following statements is true regarding this patient’s diagnosis?
(A)A history of diabetes is noncontributory.
(B)It carries a high risk of gallbladder perforation.
(C)The Murphy sign is always present.
(D)This case, like the majority of cases, is due to gallstones
(B) Emphysematous cholecystitis occurs predominantly in patients with diabetes, often in the absence of gallstones. Due to gas producing bacteria (E.coli) Emphysematous cholecystitis is associated with a high risk of gallbladder gangrene and perforation and usually requires urgent cholecystectomy and covers with cef-mitro.
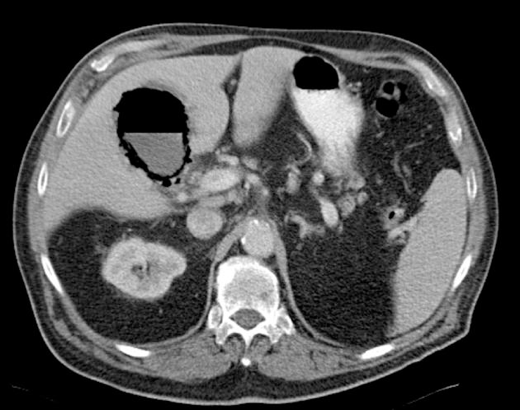
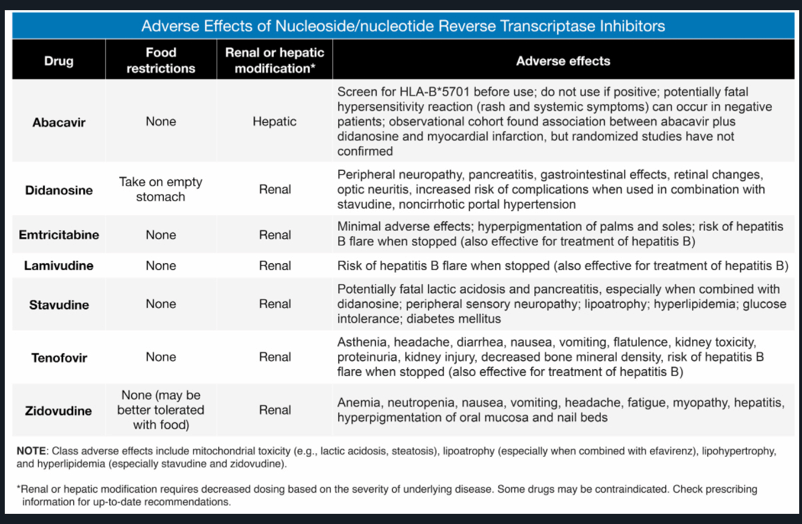
A 48-year-old man with a history of human immunodeficiency virus infection presents with abdominal pain for four days. The pain is epigastric, radiates to the back, and is associated with nonbloody, nonbilious vomiting. He has tenderness in the epigastrium but a negative Murphy sign. There is no guarding or rebound tenderness. His laboratory studies are significant for a WBC count of 19,000/ML, hemoglobin of 14 g/dL, lipase of 650 U/L, aspartate aminotransferase of 30 U/L, and alanine aminotransferase of 40 U/L. Which of the following medications is most likely responsible for his condition?
(A) Didanosine
(B) Indinavir
(C) Isonizied
(D) Pentamidine
(A) Currently, antiretroviral therapy for the treatment of human immunodeficiency virus (HIV) infection utilizes a three-drug protocol. The recommendation includes the use of two nucleoside reverse transcriptase inhibitors (e.g., abacavir, didanosine, emtricitabine, tenofovir, zidovudine) plus one of the following: a protease inhibitor (e.g., indinavir, ritonavir), an integrase inhibitor (raltegravir, dolutegravir), or a nonnucleoside reverse transcriptase inhibitor (e.g., efavirenz, nevirapine, rilpivirine).
Didanosine causes peripheral neuropathy, lactic acidosis, pancreatitis, and insulin resistance.
A 32-year-old woman presents with abdominal pain, Medically free and her only medication is a OCP. She reports that she felt well until 3 days ago, which is when she noticed the gradual onset of constant, poorly localized abdominal pain. She explains that the pain has worsened over time. She has had nausea, and today she has experienced several episodes of diarrhea.
On examination, she appears uncomfortable. Vitally stable. Her abdomen is soft and mildly tender to palpation diffusely, without rebound, guarding, or masses. Her stool is heme positive.
Laboratory values are notable for: White blood cell count: 16,000/µL, Metabolic acidosis: Positive, Bicarbonate: 19 mEq/L, Lactic acid: 2.3 mmol
1-What is your next step?
2-What is most likely the diagnosis?
3-How to manage it?
1-Computed tomography of the abdomen and pelvis with intravenous contrast reveals a thrombus in her superior mesenteric vein.
2-Mesenteric venous thrombosis
3-Intravenous heparin and serial examinations