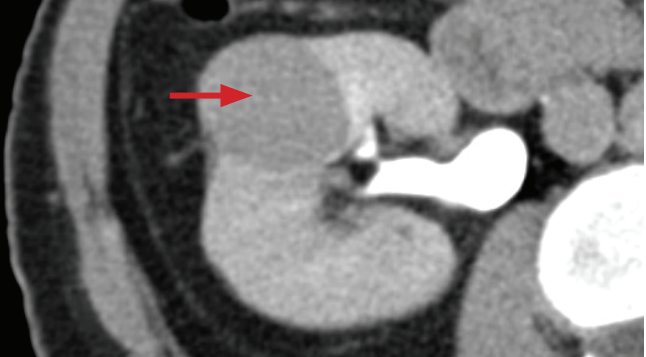
R1's it's important to know your limitations. In general, this size renal lesion is too small to characterize on cross-sectional imaging.
Less than twice the slice thickness of your study.
First years will know this is the sign the US artifact that raises suspicion for a urinary calculus.
Twinkling artifact (or twinkle artifact...I've seen people get into heated debates over this). Hyperechoic foci alone in the kidneys tend to get overcalled as stones, but if you have this artifact you can be more confident in you diagnosis.
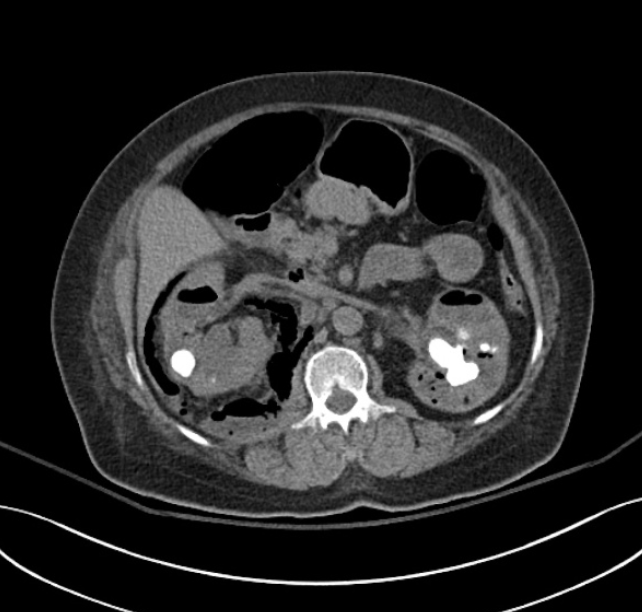
First Years know this is the term to describe the appearance of the kidneys shown here. Although nonspecific (and nonsensitive) it is classically seen in acute pyelonephritis.

Striated nephrogram.
Tip: This can be easy to miss on axials. Coronals are your friends.

First years know this is the housnfield unit threshold to call a hyperdense cyst on non-con CT.
>70 HU.
This implies benign hemorrhagic or proteinaceous cyst. (Bosniak category II)
This is the most common subtype of RCC.
Clear Cell RCC
Expect to see avid enhancment.
Associated with VHL
R1's will know, that if you see papillary renal cell carcinomas that are hereditary you likely have this condition (don't overthink it).
Hereditary papillary RCC (HPRCC)
Its an autosomal dominant disease associated with MET mutations.
Topic
This morning's assigned lecture
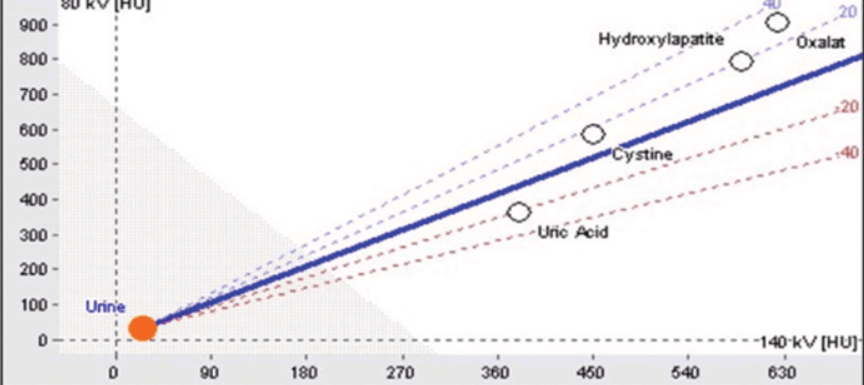
These are how absolute (definite) enhancement is defined for a lesion on a dedicated renal protocol CT and MRI.
20 or greater increase in HU on CT, or 20% greater signal intensity on MRI.
Most renal stones are radiopaque on CT with the exception of matrix stones, and this stone that is classically seen in this patient population (need two answers).
Indinavir stones are seen HIV patients undergoing antiretroviral therapy.
This is the diagnosis that explains what's going on here.
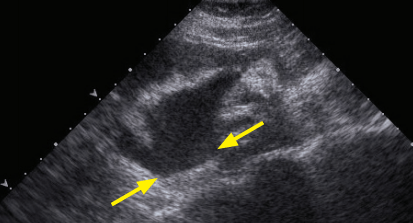
Pyonephrosis
Essentially pus under pressure. This is an emergency that needs to be acted on rapidly with either nephrostomy or stent.
US findings: nonshadowing echogenic material in a dilated collecting system. Fluid-fluid level may or may not be present
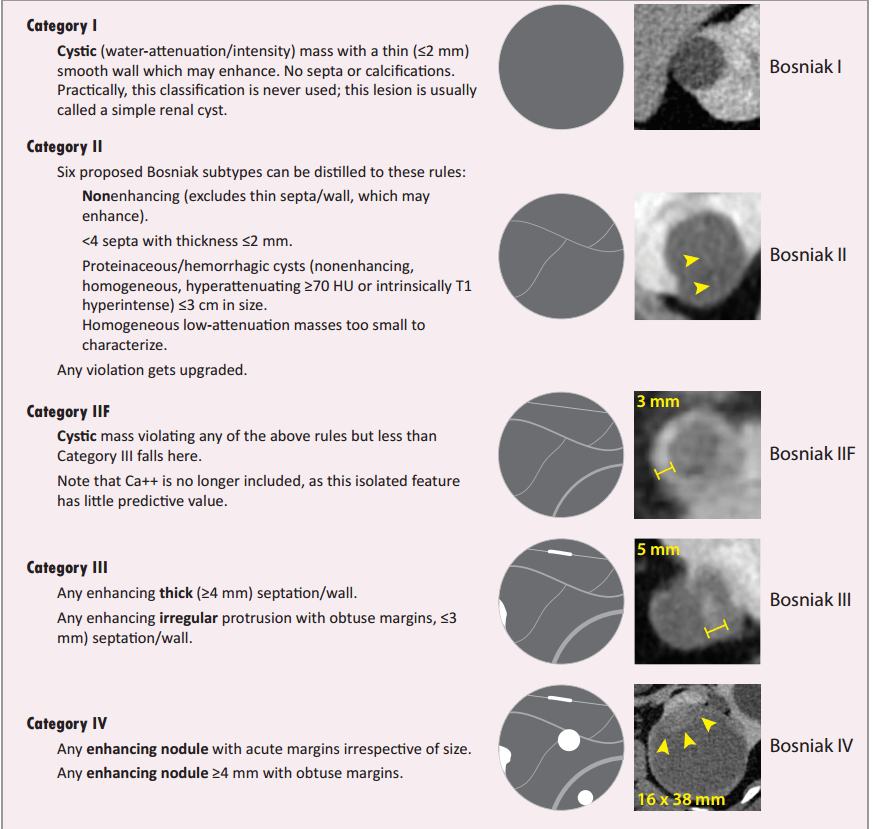
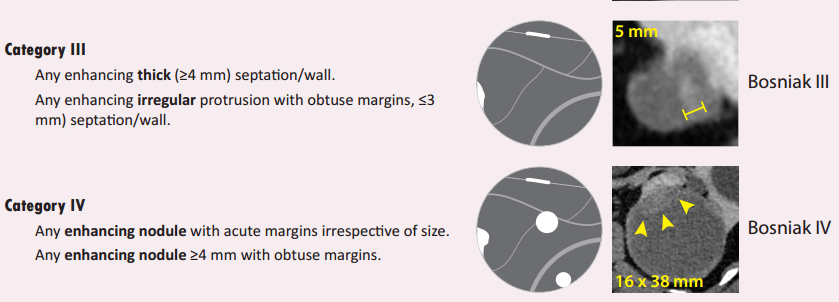
This is the Bosniak Category that describes the renal finding shown here:

Bosniak Category III
(Thick enhancing thick septation)
This RCC subtype has the best prognosis.
Chromophobe

Best prognosis with a 90% 5-year survival.
Least common subtype.
Associated with Birt-Hogg-Dube
Similar pathologic origin to oncocytomas
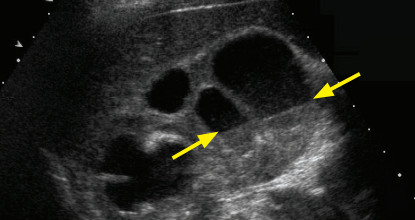
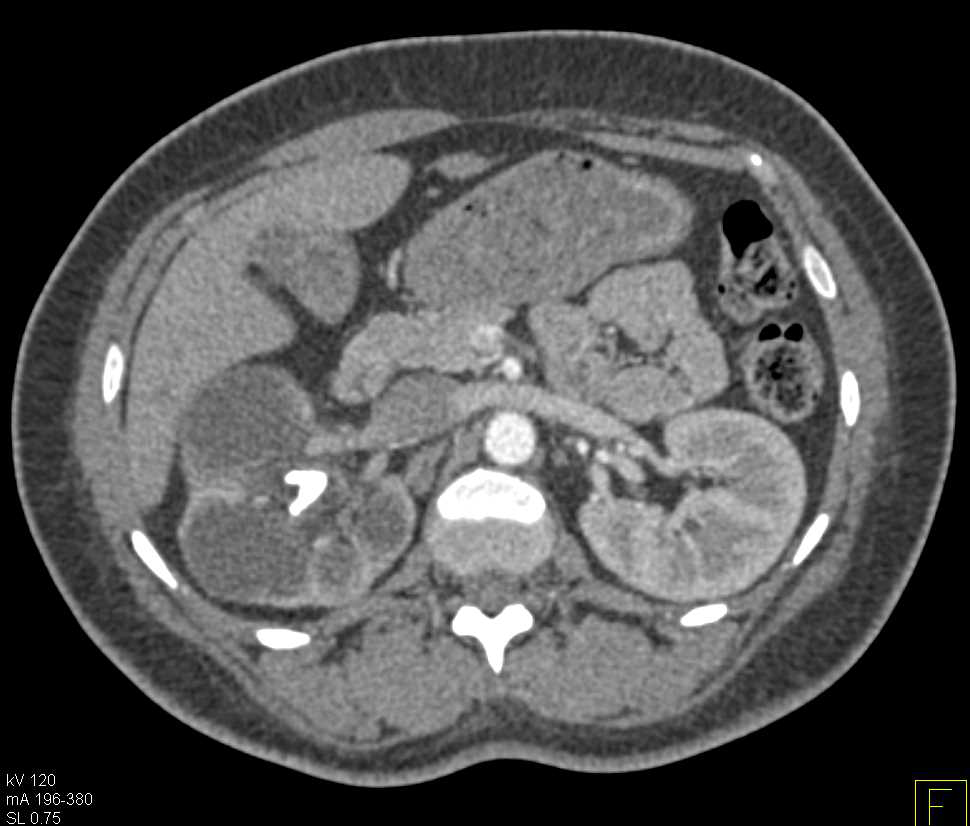
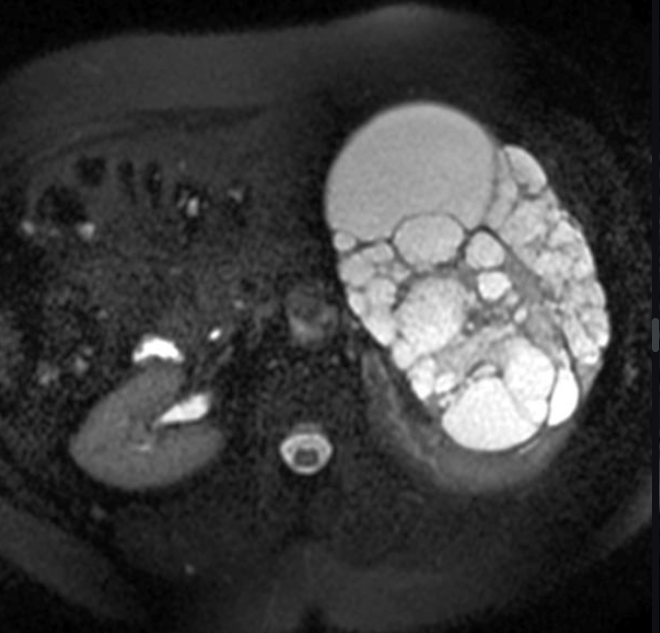
This syndrome is shown here:



Tuberous Sclerosis
Bilateral AML's should be enough on boards for you to pull the trigger on TS.
Tuberous sclerosis (TS) is an autosomal dominant neurocutaneous disease caused by a tumor suppressor gene mutation. It manifests clinically with seizures, developmental delay, and (mostly) benign tumors in multiple organ systems.
Look for cortical tubers and SEGA's in the brain, LAM in the lungs, rhabdomyomas in the heart, AMLs and renal cancer in the kidneys
Named for a doctor who wrapped animal kidneys in cellophane (seriously), this condition shown here is a rare cause of secondary hypertension, usually following trauma.

Page kidney
It's what you get when a subcapsular fluid collection (usually a hematoma) compresses the renal parenchyma and decreases blood flow. This leads to increased renin and so on and so forth until you get HTN, usually several months after.
Tx is percutaneous drainage.
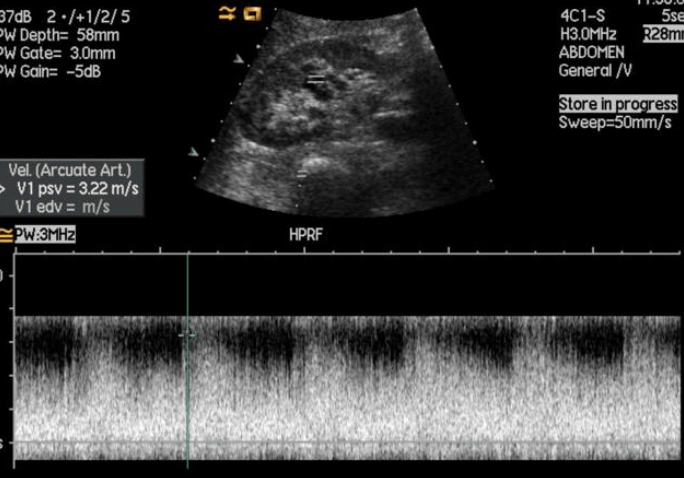
This is the sonographic resistive index values that suggest acute obstruction.
A RI of >0.7 on the affected side, or a difference between >0.1 between kidneys suggest acute obstruction.
RI is not used for diagnosis of chronic obstruction.
For review, RI =(PSV-EDV)/PSV.
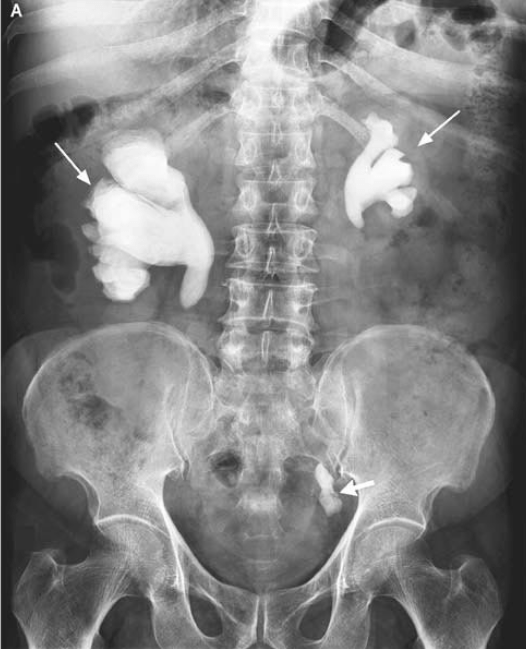
This is the diagnosis present:
Xanthogranulomatous pylonephritis
It's a chronic renal infection due to obstructing staghorn calculi. The majority present diffusely, but you can have a localized (tumefactive XGP) which can mimic a renal mass.
Classic T finding shows fibrofatty replacement creating a "Bear paw appearance"
Treatment is nephrectomy due to abscess and fistula formation.
Chart review of the patient with the following image will reveal this classic history:

Lithium use (also would accept nephrogenic diabetes insipidus or psychiatric history)
Classic appearance of lithium nephropathy is numerous scattered uniform microcysts in normal-sized kidneys.
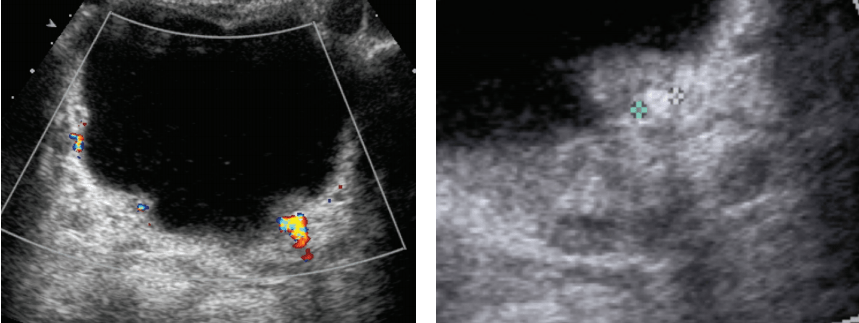
It's the entity seen here that can mimic a hypervascular renal mass:
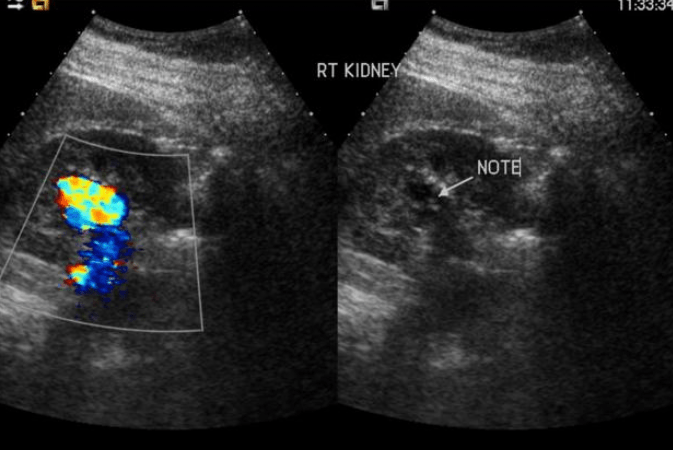
Renal AVM
The keys here are a very High Velocity Low Resistance spectral waveform associated with the renal lesion on US (know your waveforms for common pathologies back and forth for the test), and on CT you have a tangled vascular structure with early filling of the R. Renal Vein
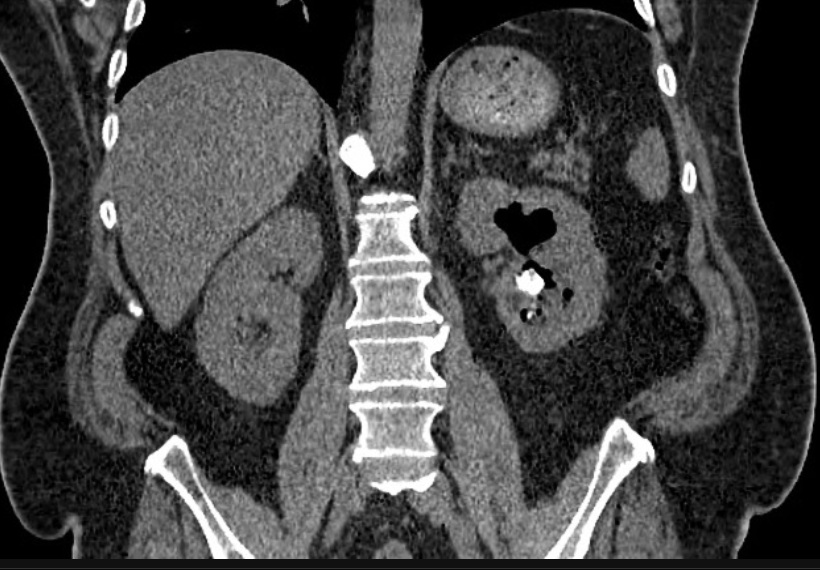
It's the syndrome shown here:


von Hippel-Lindau
AD mutation of the VHL tumor suppressor on chromosome 3 which leads to cystic neoplasm in multiple organ systems
In GU: multiple bilateral RCC's (clear cell); pheochromocytoma, renal cysts
In CNS: hemangioblastomas of the brain and spinal cord
Pancreas: neuroendocrine tumors, pancreatic serous cystadenoma, pancreatic/hepatic cyts
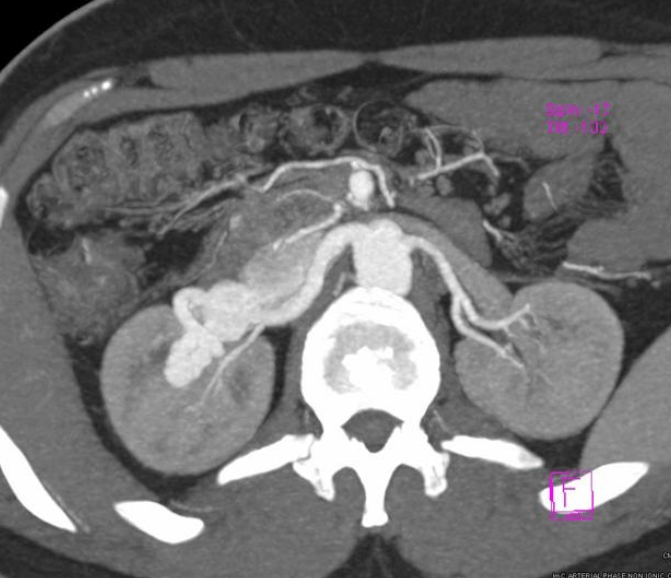
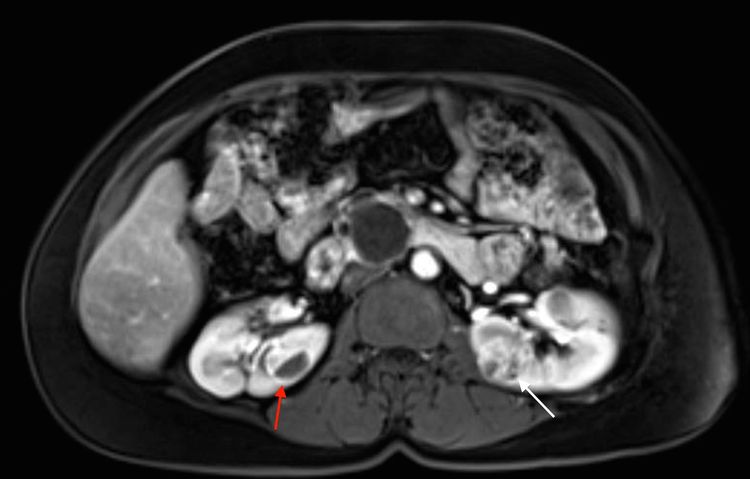
Involvement of what renal anatomy differentiates Grade III injury (typically treated conservatively) from Grade IV (requires intervention)
Extension into the collecting system (causing urinary extravasation)
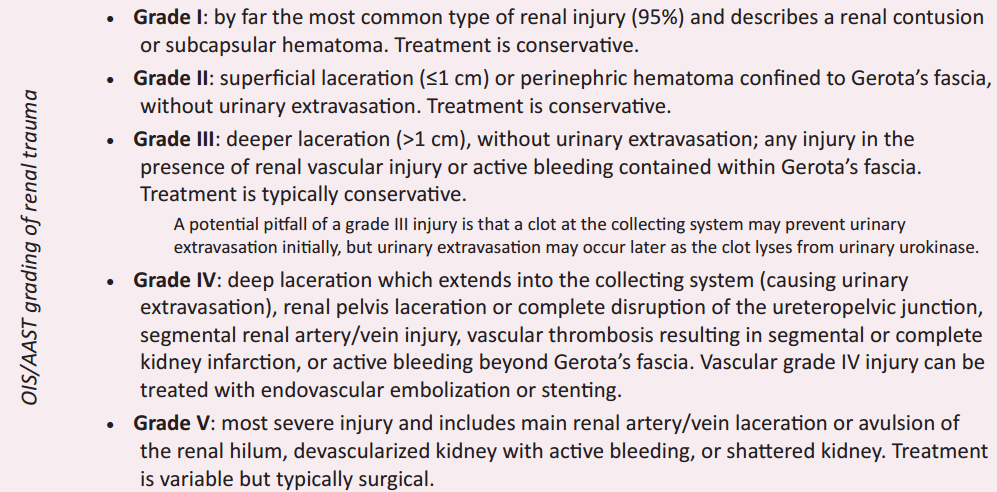
That's how dual energy CT differentiates between mineral composition of different stones.
Modify the kVP of the exam to target different K-edges (voltage where contrast is maximized--a classic physics question)
It would be a good idea to check the patient's EMR to confirm that they had this medical condition which resulted in the ultrasound seen here.. (Hint: the liver is normal. Kidney measures 144 mm).
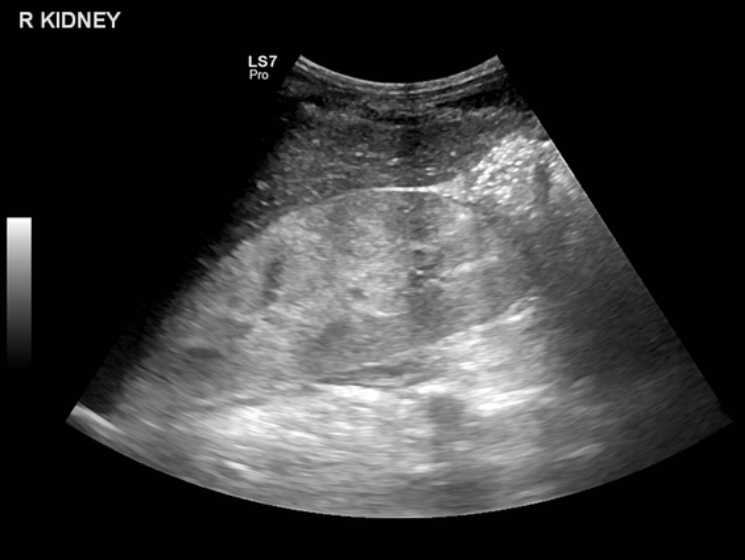
HIV.
HIV associated nephropathy. Renal imaging on US is characteristic with enlarged, echogenic kidneys with decreased renal sinus fat. This is a boards favorite.
This is what's up in this 55 year old lady's kidney (T2 coronal, axial, T1 parenchymal phase post con:


Cystic nephroma, aka the artist-formerly-known-as-and-still-likely-to-be-tested-as multilocular cystic nephroma.
These used to be lumped together with pediatric cystic nephromas (Michael Jackson Lesion), now pediatric cystic nephromas are considered distinct based off a the DICER1 gene mutation.
These are classified under the mixed epithelial and stromal tumor (MEST family).
CT findings: multilocular cystic mass (often herniating into the pelvis causing obstructive calycectasis). No nodular or solid enhancement...if there is enhancement think multilocular cystic renal neoplasm of low malignant potential aka the artist-formerly-known-as multilocular cystic RCC
Renal Medullary Carcinoma is most strongly associated with this demographic.

Young adult male with sickle cell trait.
It's an extremely aggressive and infiltrative neoplasm.
Prognosis is dismal with mean survival of 15 months. Chemotherapy is not effective.
This is the most common subtype of RCC associated with the pictured syndrome:


Chromophobe
This is Birt-Hogg-Dube, an AD syndrome of dermatologic lesions, cystic lung disease, and multiple renal tumors (oncocytomas, and chromophobe RCC's and chromophobe-oncocytoma hybrids)
This is the term for the pathology seen here:

Hint: Here's an old chest radiograph:
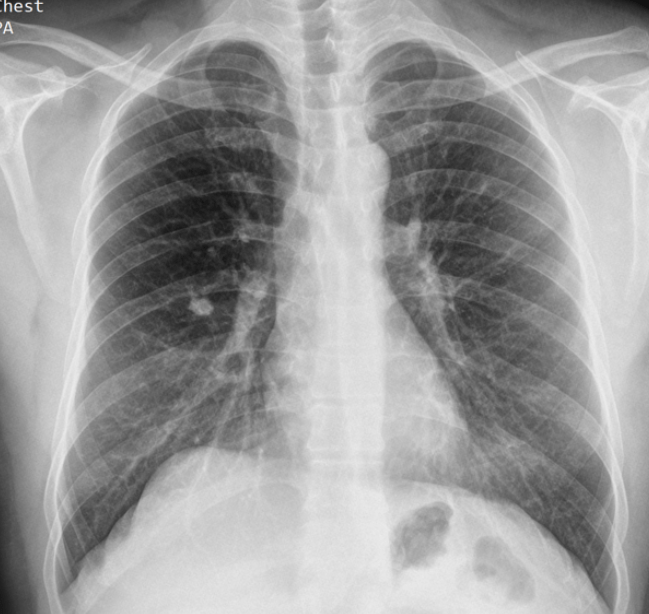
Putty Kidney
An autonephrectomy in end-stage renal tuberculosis patients. Presents with atrophic, calcified kidney
(The chest xray is a Ghon Lesion)
That's the name of the organism typically responsible for struvite (staghorn) calculi.
Proteus mirabilis
A urease producing bacteria. Classic step question and sadly fair game for the core exam too.

This is the condition shown here (We'll spot you the stone):
Emphysematous pyelitis.
Gas within the renal collecting system without features of pyelonephritis. It caries a good prognosis and responds well to IV abx.
Contrast this with emphysematous pyelonphritis (tricksy jerks gave a relatively mild condition and an emergent condition similar sounding names). That's a morbid infection with gas formation within the renal parenchyma that can rapidly lead to necrosis and sepsis. That's also typically seen in diabetics or immunocompromised.
In addition to hepatic cysts, autosomal dominant polycystic kidney disease (ADPKD), is known for this uncommon but highly testable extrarenal manifestation.

Saccular cerebral aneurysms (seen in 15%) of patients.
Some more ADPKD trivia to know for boards:
It's the one that affects adults (aRpkd is in kiddos and gives you hepatic fibrosis rather than cysts, and is more likely to be fatal)
ADPKD is why 10% of HD patients exist.
ADPKD and cancer risk is controversial, won't likely to be tested
This is the entity seen here.

Oncocytoma (I'd also accept chromophobe RCC if you appropriately justify it)
It's a benign tumor of tubular cells. Oncocytomas typically have a central scar plus/minus spokewheel septations. A flip flop sign is when the hyperdense central scar becomes hypodense relative to enhancing parenchyma on the post-con.
All these features suggest it's an Oncocytoma, however, you can't fully exclude RCC because of imaging overlap. Biopsy can usually exclude Clear cell and papillary subtypes, but chromophobe RCC can yield oncocytic cells. So most oncocytomas will still get the knife.


Hereditary leiomyomatosis and RCC (HLRCC)
HLRCC is an autosomal hereditary syndrome characterized by the development of multiple RCCs, uterine and cutaneous leiomyomas, and adrenal hyperplasia. The most commonly seen renal cancer subtype is papillary RCC.
This was this morning's lecture topic. I am sure you all watched it.
Radiologic anatomy of the cerebral cortex...made easy.