Name this exam finding?
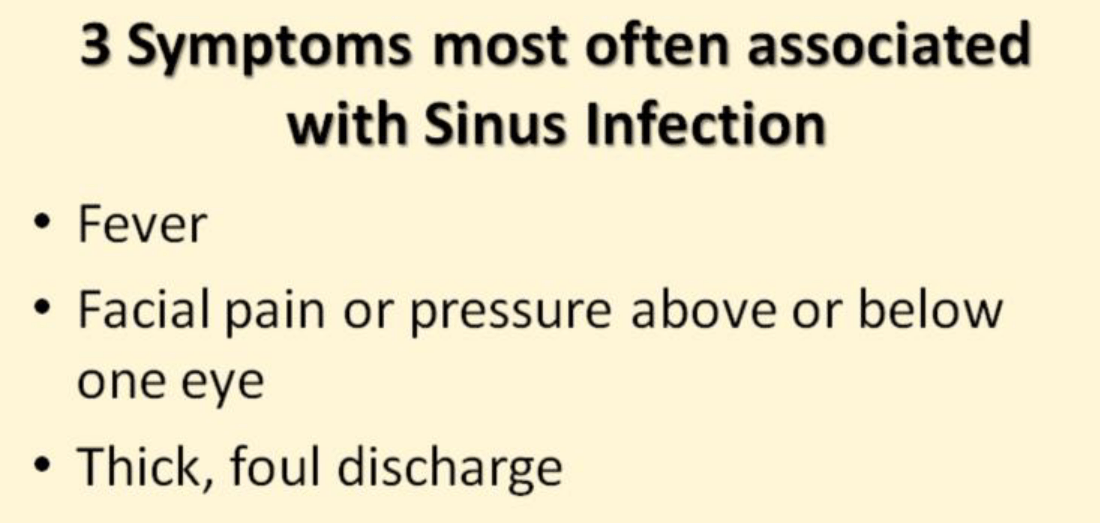
According to our lecture what are 3 symptoms most associated with sinus infection?
32-year-old female presents for evaluation of sore throat, fever. Rapid strep was negative. According to your reading name 3 supportive measures used for pain relief.
Acetaminophen, NSAIDs, opioids if needed for severe cases, viscous lidocaine, salt water gargles, single dose dexamethasone.
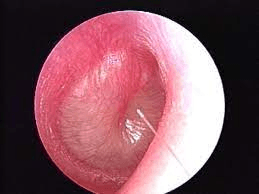
How would you document this finding?
Injected, erythematous, mild to moderate bulging with opaque appearance and white colored fluid
A 7-month-old male who attends daycare is brought in by his mother with 4-day history of fever, upper respiratory symptoms. Mom states she has been treating with over-the-counter medications including Tylenol with the last dose 3 hours ago earlier. She states today when the child woke up he was extremely fussy, and pulling on both of his ears. On examination you find a double ear infection. Patient does not have any known allergies. What medication would you prescribed? And how which dose this medication?
Amoxicillin 80 mg/kg/day divided twice a day for 5 to 10 days
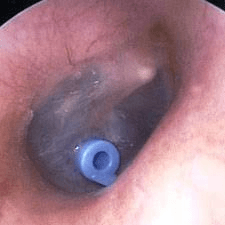
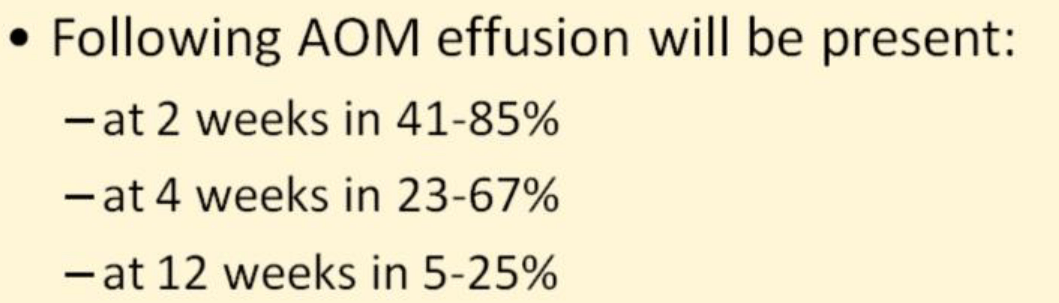
32-year-old female presents for evaluation of right ear pain. On examination you see this. Patient denies any additional URI symptoms. No fever. Has not had any medication for symptom. What would you diagnose this finding for?
Myringitis is a bacterial or viral infection of the eardrum. Myringitis is a form of acute otitis media. Acute otitis media often occurs in people with a cold or allergies. The infected ear is painful.
Patient presents to the clinic with chief complaint of sore throat what information is important to obtain when you are gathering your history.
Exposures, ability to tolerate liquids-inability to tolerate liquids is a red flag, this may indicate a more serious infection such as epiglottitis, the presence of esophageal foreign body, or abscess., immunization history-haemophilus influenza type B vaccine makes epiglottitis likely slightly, prior history of Epstein-Barr virus-makes acute mononucleosis less likely.
Key symptoms constitutional symptoms such as cough, sneezing make strep throat less likely, trismus or difficulty opening the jaw this symptom may represent abscess formation, stiff neck may be a sign of retropharyngeal abscess, history of sexual activity may indicate a risk of gonococcal pharyngitis.
Child age 8 months.
Treated with antibiotics 3 weeks ago for AOM. fussing with pulling on ears, restless sleep, poor appetite, URI symptoms. Temperature 102.9.
Left ear:

What would your diagnosis be and how would you treat this patient?
Otitis Media with Effusion (OME) is the condition of fluid present in the middle ear. Inflammation may be associated with OME. The spectrum of tympanic membrane findings can be challenging for one to appreciate the subtle differences in the progression from MEE and OME to AOM. Visualization of the tympanic membrane is critical to differentiate between AOM and OME. “A middle ear effusion may be present after resolution of an episode of AOM, or it may develop because of a viral upper respiratory tract infection that produces eustachian tube dysfunction. In both of these settings, the middle ear effusion is not an infectious process and will not benefit from antibiotic therapy.”
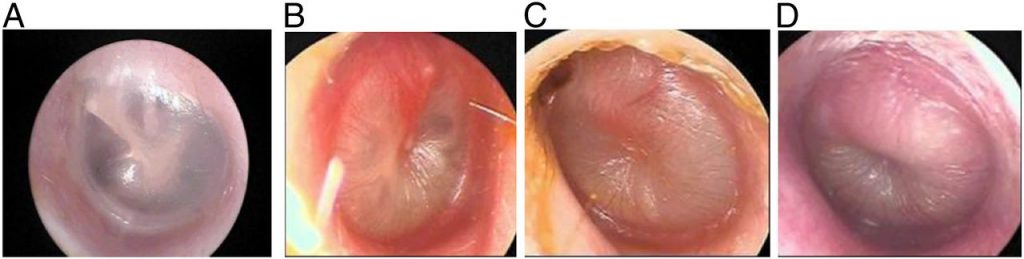
A, Normal TM. B, TM with mild bulging. C, TM with moderate bulging. D, TM with severe bulging.
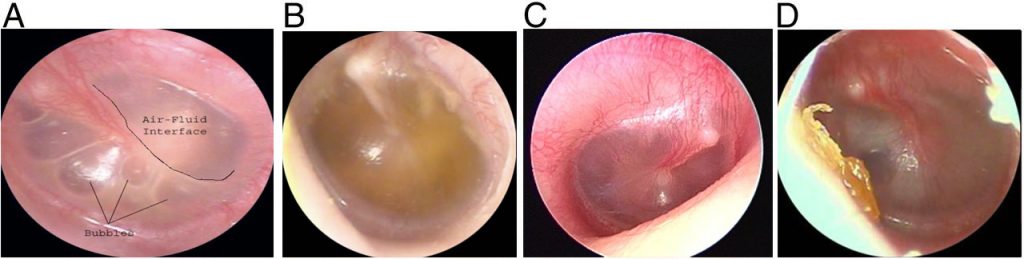
A, OME with air-fluid levels and bubbles. B, OME with prominent malleus and amber colored fluid. C, OME with prominent malleus and minimal erythema (injection). D, OME with opaque appearance and white colored fluid.
The name of the scoring system may help identify patients who are more likely to be infected with group A Streptococcus. What are the criteria?
Centor Criteria. Age, presence of exudates on tonsils, tender swollen anterior cervical nodes, fever, absence of cough
You diagnosed the patient with otitis externa, history includes, see picture below: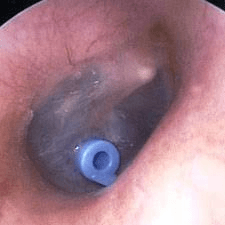
How would you treat this patient?
While we generally prefer topical fluoroquinolones over other options for the treatment of otitis externa because of their antimicrobial spectrum, lack of potential ototoxicity, and lower risk of allergic reactions, they are more costly than other options and in the United States, insurance coverage is variable.
This will present with swelling superior to the tonsil and will have palpable fluctuance and often displace the uvula to the other side, what is this exam finding increase suspicion for?
Peritonsillar abscess.
The mother brings in her 2-year-old child with complaints of fever, sore throat. Patient does attend daycare. Exam reveals the following image below, this increases your suspicion for what diagnosis?

Coxsackievirus, Which Can Cause an Combination of Fever, Sore Throat, Lesions of the Mouth, Hands, or Feet. These Characteristic Ulcerations in the Posterior Pharynx Are Diagnostic and a Rapid Strep Test or Culture Is Not Required.
What is the maximum dose of amoxicillin for a child diagnosed with strep pharyngitis.
500 mg.
There are several rashes and skin findings associated with streptococcal infection, name 2 of them.
scarlatiniform "sandpaper" "strawberry tongue"
"strawberry tongue"

Erythema marginatum May be associated with other features such as subcutaneous nodules and chorea and presents if there is rheumatic fever a possible complication of untreated strep pharyngitis.  Impetigo and erysipelas Are also caused by Streptococcus infections and present with rash is better not associated with pharyngitis
Impetigo and erysipelas Are also caused by Streptococcus infections and present with rash is better not associated with pharyngitis

How would you describe this finding? The presence of this finding in addition to anterior cervical lymphadenopathy makes this a more likely causative organism, what is it?
palatal petechiae, group a strep, Remember The presence of or the amount of exudate does not determine severity of infection or help distinguish bacterial from viral causes.
A 12 yo boy, Denies PMH, KNA, presents to clinic accompanied by dad with complaints of right ear pain. Dad states symptoms began about 3 days ago after they returned home from a water park. Denies any fever, cough, or additional URI symptoms. Has been treating with Motrin. Last dose was 3 hours ago. On exam you look into the right ear and see this... What is your diagnosis? What is your plan?
What is your diagnosis? What is your plan?
Otitis externa:
The ideal antibiotic regimen should have coverage against the most common pathogens, S. aureus and P. aeruginosa:
●The topical fluoroquinolones ofloxacin and ciprofloxacin provide coverage against both pathogens. In two clinical trials, topical ofloxacin appeared to be as effective as topical neomycin-polymyxin B-hydrocortisone. Another trial found that topical ciprofloxacin-dexamethasone was superior to topical neomycin-polymyxin B-hydrocortisone in decreasing inflammation, edema, and achieving pain control.
●Polymyxin B (a polypeptide antimicrobial) and neomycin (an aminoglycoside) are antibiotics that are combined in many frequently used ototopical medications. Polymyxin B is effective against P. aeruginosa, while neomycin is effective against S. aureus.
●Topical aminoglycosides (eg, tobramycin and gentamicin) are also effective against both S. aureus and P. aeruginosa.
A mother brings her 3-year-old child in with complaints of 2-day history of right ear pain. Child is noted to have a fever. Mom has been treating with over-the-counter medications with last dose of Tylenol 45 minutes ago. What additional information is important to obtain when gathering your past medical history?
Participation in daycare, bottlefeeding, exposure to tobacco smoke and air pollution, pacifier use
Fever, this may possibly be the only indicator medical history for infants, date of last episode or episodes of acute otitis media, antibiotic use specially amoxicillin the last 3 to 6 months, history of resistance, immunizations especially pneumococcus, influenza, Hib
A 32-year-old female presents to the urgent care clinic with complaints of upper respiratory symptoms. States that she has been taking over-the-counter medications for the last week with no improvement. Feels like symptoms have been worsening for the last 48 hours. Believes she may have a low-grade fever but has been treating with medications so is unsure if she actually has a fever or she is just feeling warm. What would you diagnose for this patient how would you treat this patient? Patient does not have any known allergies.
Indications for antibiotics include typical sinus symptoms that are persistent or do not decrease after more than 10 days, severe symptoms lasting greater to or equal to 4 days, worsening or double sickening greater than 3 days. Treatment would include treatment for 7 days of Augmentin. Adults can be given 2 g twice a day, children 90 mg/kg divided twice daily. Doxycycline for patient's allergic to penicillin, Bactrim–there is high resistance to this commendation drugs will prescribe cautiously, cephalosporins there is also high resistant to this drug so prescribed cautiously, macrolides again high resistant rate due to over prescribing so proceed cautiously.
You diagnosed the patient with otitis media, what additional documentation is important think medicolegal pearls. State 3.
Documentation should include the lack of meningeal signs, document lack of worst headache in life as appropriate, document 9 tenderness to palpation over the mastoid area, document the lack of tympanic perforation
You just diagnosed a 12yo with otitis externa. You did not need to place an ear wick. You are prescribing topical ear suspension drops. Please share what you would include in your discharge of this patient...
Installation of topical preparations — Correct application of topical agents to the site of infection is a key element in the effective treatment of external otitis, regardless of severity. A common cause of failure for topical treatment is underdosing.
Proper installation of ear drops entails tilting the head toward the opposite shoulder, pulling the superior aspect of the auricle upward, and filling the ear canal with drops. Patients should ensure that sufficient medication is used to adequately fill the entire ear canal, typically 4 to 6 drops for an adult ear canal. In young children, the earlobe should be pulled downward in order to adequately fill the canal.
Patients should lie on their (opposite) side for three to five minutes following instillation or place a cotton ball in the ear canal for 20 minutes following instillation to maximize medicine exposure.
Ear hygiene during acute episode — The ear should be protected from water during treatment for external otitis. During bathing or showering, patients can place a cotton ball coated with petroleum jelly in the ear canal. Patients with active external otitis should not swim and ideally should refrain from water sports for 7 to 10 days. Competitive swimmers may consider return to swimming at two to three days if pain has resolved and they wear well-fitting ear plugs.
Hearing aids, “ear-buds,” and other similar devices should not be worn until pain and discharge have subsided [5,22]. In addition, these devices should be disinfected prior to re-use.
Prevention of recurrence — Preventive interventions may be appropriate for patients with recurrent external otitis, immunocompromised hosts, and patients with a dermatologic condition affecting the ear(s).
To prevent recurrence, patient education regarding proper ear hygiene is essential. Patients should be advised that the ear canal is self-cleaning, and that fingers, towels, cotton swabs, or other foreign objects should not be inserted into the canal.
External otitis is a frequent occurrence in individuals who are habitually in the water [23]. Specific measures for those who engage in water sports include use of ear plugs, shaking the ear dry after swimming, and blow drying the ear after water exposure (placing the blow dryer on low speed and heat settings at least 12 inches away from the ears) [24].
Drops containing alcohol and/or acetic acid help to dry the ear, prevent skin maceration, and re-acidify the ear canal may be used, but it is unclear if this prevents recurrence of external otitis.
Hearing aids should be removed nightly and cleaned regularly.
This exam finding may demonstrate an anterior bulge in the posterior pharynx. Obtaining A soft tissue lateral neck x-ray will reveal an increase in the prevertebral soft tissue and may also demonstrate air within the soft tissue. Name of the diagnosis.
Retropharyngeal abscess.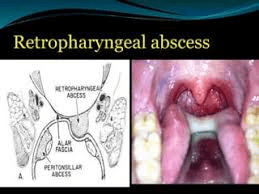

When obtaining a history for patient presenting with upper respiratory symptoms what information is important to gather from the patient?
Asked the patient for details about having a history of any of the following, discolored nasal discharge such as yellow, green, blood-streaked. Cold symptoms getting worse or not decreasing after more than 14 days, pain behind the eyes or cheeks, headache, upper tooth pain, ear congestion and/or pain, symptoms with decreasing but are now worsening again i.e. double sickening, facial redness cellulitis overlying maxillary sinuses periorbital cellulitis, sore throat, postnasal drip, cough, and fever may be present but their presence is not required for making a diagnosis.
26-year-old male presents for evaluation of upper respiratory symptoms. Symptoms began 2 days ago. Has been complaining of sinus congestion, sore throat, and cough. Symptoms tend to worsen at night. Denies any fever but states he feels some chills. Has not had any medication for symptom management. How would you treat and educate this patient?
Steroid Neillsville sprays will help reduce nasal inflammation, oral steroids can help reduce nasal inflammation, decongestions may or may not be of benefit, pseudoephedrine can be given if the patient is not allergic or if there are no contraindications, mucolytic's may or may not be of benefit, antihistamines only if allergic component is suspected, nasal saline sprays or rinses can help clear nasal secretions. Topical decongestions and antihistamines are not recommended because of the risk of dependency and rebound symptoms. Increase fluid intake, coolmist humidifier, Vicks vapor rub. This is a viral illness and does not require antibiotic therapy.
When diagnosing a patient for acute sinusitis what information is important from a medical legal standpoint?
Documented lack of signs consistent with cavernous vein or sinus thrombosis, (severe headache, visual changes)
Documented lack of meningeal signs. Document normal mental status.
8-year-old patient presents to clinic accompanied by dad with complaints of left ear pain. Dad states patient has had fever last night. Has been treating with Motrin. Last dose 2 hours ago. Patient is up-to-date with routine vaccines. Name 3 additional differential diagnoses and associated symptoms for ruling in these diagnoses.
Acute otitis media:
Middle ear effusion with moderate to severe bulging, moderate severe ear pain, fever of greater than 39 °C, symptoms lasting greater than 48 hours, fluid in the ear canal is not associated with acute otitis media (rupture of tympanic membrane)
Potential diagnosis of acute otitis media with the following:
Mild bulging of tympanic membrane, ear pain less than 48 hours, intense erythema
Otitis media with effusion (not infectious):
Middle ear effusion present, little to no discomfort, no redness, no fever or evidence of toxicity, possible decreased hearing
Mastoiditis:
Acute otitis media present, post auricle tenderness, redness and swelling, fluctuance and a mass or draining fistula, displacement of auricle downward and upward in children less than 2 and upward and outward in children greater than 2.
Bacteremia in infants:
Age 3 to 36 months, rectal temperature greater than 39 °C or higher that may be relieved with acetaminophen or ibuprofen, WBC count greater than 15,000