A 29 year old female comes to the doctor sipping and crunching on a slushie for her yearly check up. Labs show a Hb of 8g/dL (normal 12.5-15). Further work up shows a ferritin of 2 (13–150 ng/mL) and a total iron binding capacity (TIBC) of 457 (normal 250-400). You tell her she has this kind of anemia.
What is iron deficiency anemia.
Why is she eating a slushie?
What are other common symptoms of iron deficiency anemia?
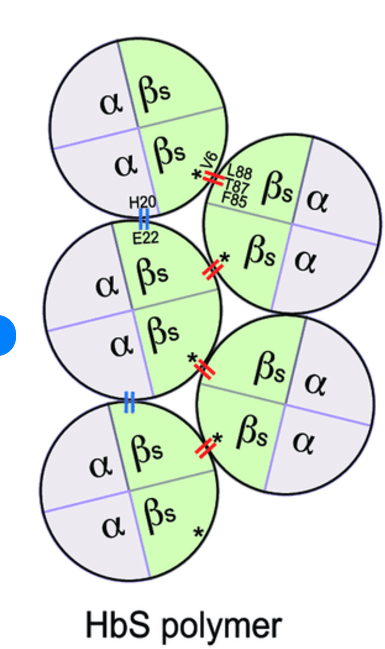
Hb S is made up of these globin chains.
2 alpha chains and 2 beta chains with a mutation in the beta chain that results in glutamine changing to valine.
What immunoglobulin is involved in warm autoimmune hemolytic anemia?
IgG
Burkitt's Lymphoma is associated with which Virus?
EBV
(HIV?)
Cmyc 8;14 translocation, classic starry sky appearance


Hemophilia A is caused by a deficiency in this coagulation factor and is characterized by what kind of bleeding ?
Factor VIII
usually bleeding into joints , soft tissue bleeding, post operative bleeding.
(platelet defects are often mucocutaneous bleeding)
What is the reversal agent of warfarin
Vitamin K
notes for next year
1. make it harder as numbers get bigger
2. plummer vinsent questoin. a harder ida question
3. if have 3 teams needs a final jeopardy
4. have an initial hard question to decide who gets to go first.
This patient has a hb if 8.7g/dL. The MCV is 104fl. See Red cells in the picture below. Name three causes of macrocytic anemia 
Macrocytosis
macrocytic anemia is seen in
1. B12 deficiency: 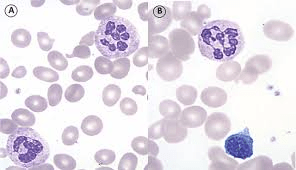
-other symptoms of +rhomberg sign / dorsal columns
2. Folate deficiency
3. Alcoholism
4.Liver disease

5. MDS
6. OTher hematologic malignancies
A 29 year old female comes to you on ferrous sulfate. She reports her primary doctor has been giving her iron to help her Hb of 9g/dL but it never seems to increase. She reports very light periods. You look at her CBC and conclude she may not be iron deficient, but she probably has thalassemia trait based on this MCV and RDW.
Thalassemia patients are microcytic.
Be able to differentiate a cbc from a thalassemia patient from a patient with IDA.
Thalassemia trait IDA
MCV <80 <80
RBC# HIGH LOW
RDW LOW HIGH
Cold Autoimmune Hemolytic anemia can be triggered by an infection from this type of bacteria.
What is mycoplasma pneumoniae
Cold Autoimmune Hemolytic Anemia : typically mediated by IgM and Complement which cause agglutination and extravascular hemolysis upon exposure to cold. Can see acrocyanosis: painful / blue fingers and toes.
A 25 year old nurse notices that he has chest pain when he is drinking alcohol last few times with his friends. Chest X ray shows a mediastinal mass which gets biopsied. What is the name of this cell seen on pathology?

What is the reed sternberg cell.
OWL eyes, stains CD15,30+, CD45 neg
Reed sternberg cell seen amongst a large inflammatory milieu.
29 year old female comes in to the hospital after finding a petechial rash on her lower extremeties. SHe also has some petehciae in her mouth. She has a normal Hb and WBC, but her platelet count is 3,000/uL (normal 150,000-400,000/uL). You suspect she has an Immune Thrombocytopenic Purpura or ITP. What would be your first line therapy in this patient?
IVIG and steroids.
WHat if this didn't work?
what is the mechanism of action of apixaban?
Factor XA inhibitor

A 25 year old man has a cellulitis that needs treatment. You give him a medication called bactrim or trimethoprim-sulfamethoxazole. Hb on day of visit with you for cellulitis is 13g/dL. He returns 2 days later feeling fatigued and repeat hb is 9g/dL. You note evidence of hemolysis in his labs with a elevated indirect bilirubin, low haptoglobin and elevated LDH. Blister cells are seen on PB smear. Coombs testing is negative. What is the inheritance pattern of the enzyme deficiency he has?
He has G6PD deficiency which is X linked recessive. (Still have to worry about it in women, but much more often severe in men.)
Sulfa drugs are contraindicated in people with significant g6pd deficiency.
Pentose phosphate pathway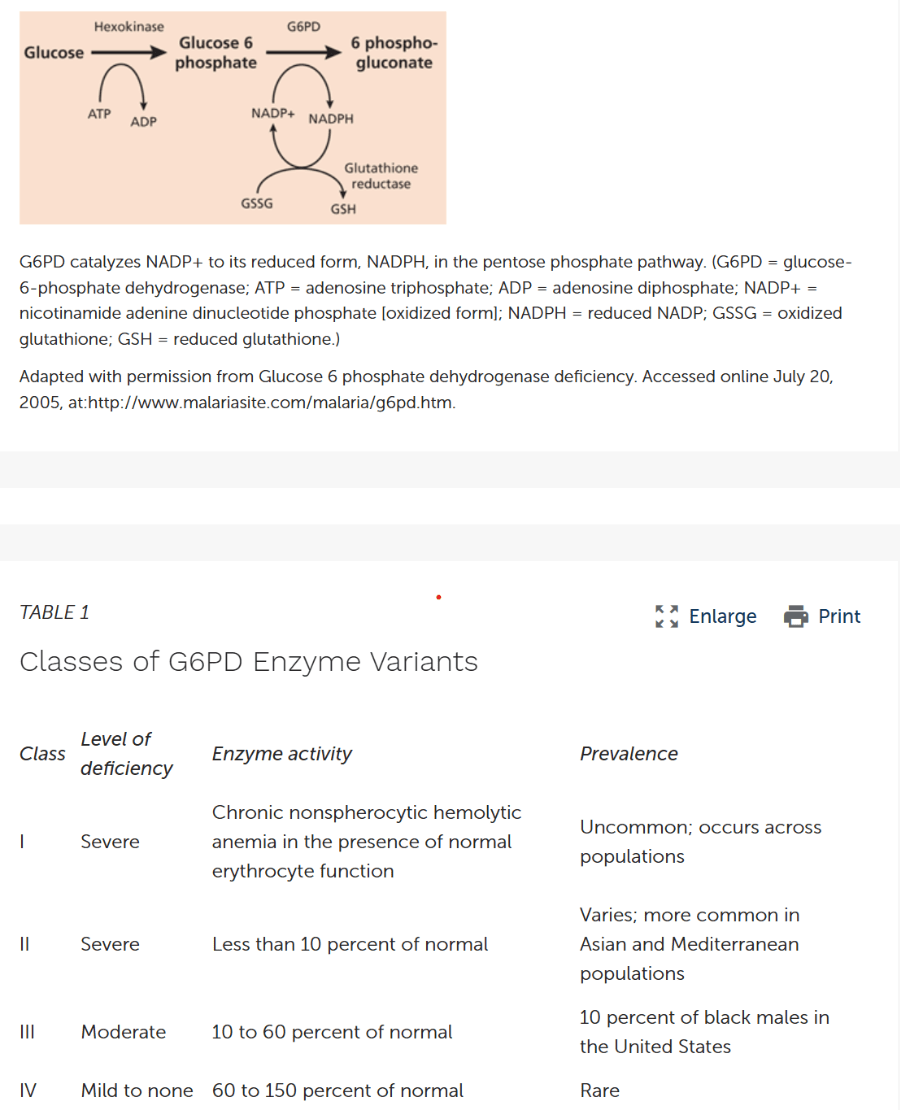
A 32 year old female with Sickle Cell disease comes in with acute aplastic crisis. Her Reticulocyte count is very low, along her her Hb which is 4g/dl, lower than her usual of 7.5g/dL (normal 12.5-15). What is the most common culprit causing aplastic crisis?
Parvovirus B19
Management: supportive care. Will slowly recover over 1-2 weeks.
What is the reticulocyte count a measure of?
aplastic crisis different from aplastic anemia.
A 72 year old female comes into the hospital with urosepsis, blood cultures growing E.Coli. The hematology team is called because her blood parameters are abnormal, she is severely ill, she has anemia with a Hb of 7g/dL (normal 12-15) and a platelet count of 55,000 (normal 150,000-400,000) and there are signs of hemolysis and she also has a low platelet count. She also starts to have oozing at her IV lines. What is the name of this cell that you see on the peripheral blood smear and what does it indicate?

Schistocytes
Are seen when there is a microangiopathic hemolytic anemia: mechanical destruction of red blood cells.
In this case, schistocytes are helping confirm the presence of DIC. (severe infection, abnormal hematologic parameters, bleeding at IV sites)
44 year old female with new onset anemia over time, notices she also has bone pain, worsening renal failure and high calcium. She is losing weight. PArt of skeletal survey is shown below. What hematologic diagnosis are you worried about?
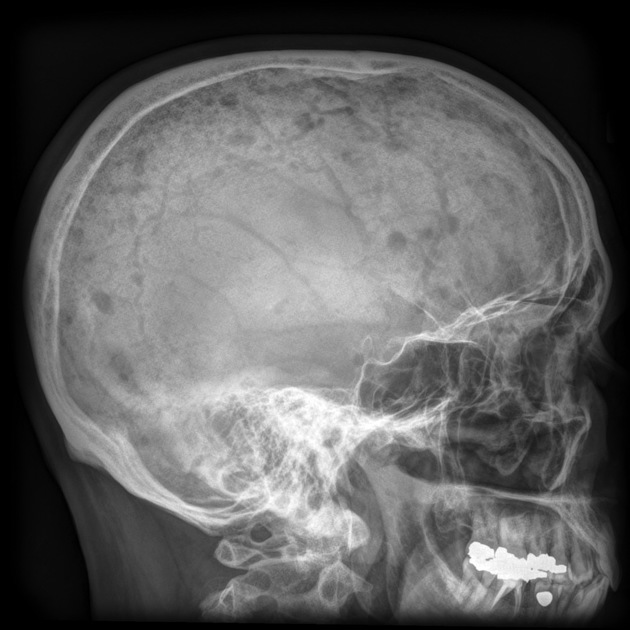
Multiple Myeloma: characterized by
Calcium high
Renal failure
Anemia
Bone lesions
After giving a patient warfarin/coumadin, these coagulation factors will be low.
Vitamin K dependent coagulation factors II, VII, IX, X
You want to give your patients with B cell lymphoma Rituximab because it is a monoclonal antibody against which cluster of differentiation (CD).
CD20.
Anemia of chronic disease is mediated by an increase in this enzyme which blocks the release of iron from macrophages as well as the absorption of iron from the gut.
What is hepcidin.
AOCD is seen in Chronic infections neoplastic disorders, SLE, RA, ckd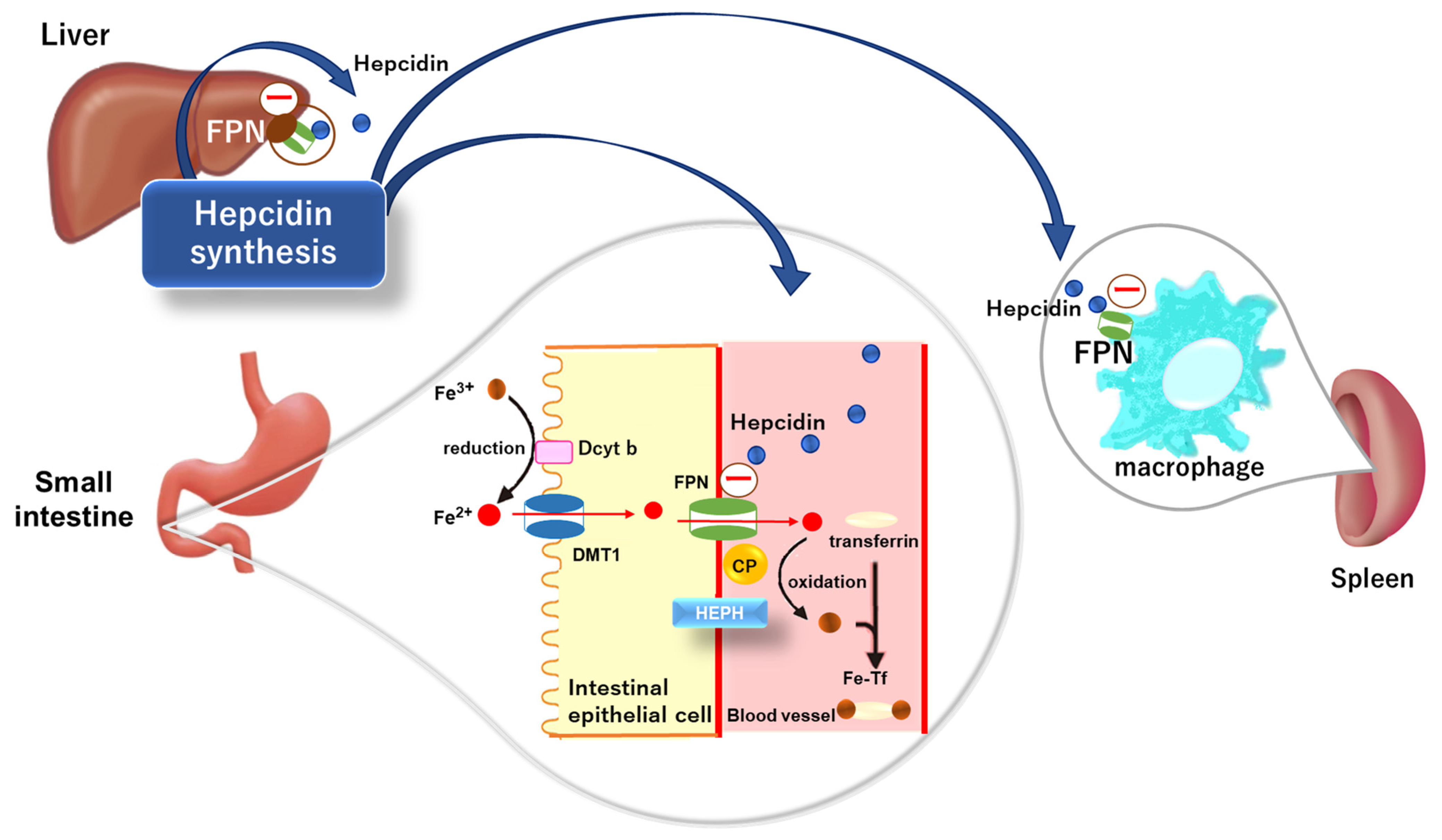
Hydroxyurea increases this type of Hb in patients with sickle cell disease.
What is Hemoglobin F
What else does Hydroxyurea do that might be useful in sickle cell disease?
A 42 year old female comes to the hospital reporting tea colored urine after waking up this morning and is found to be anemic. Coombs testing is negative but she has an elevated indirect bilirubin, high lactic dehydrogenase and a low haptoglobin. She also has mild pancytopenia (hb of 10.4 g/dL, plt of 75K, WBC of 2.5 with a neutrophil count of 1200), and is found to have a LLE deep venous thrombosis. Flow cytometry shows CD55 and CD59 negative Red blood cells. You diagnose her with this disease.
What is paroxysmal nocturnal hemoglobinuria?
Deficient of the pi-linked antigen that keeps CD55 and CD59 on red cells, these CDs protect the cell from complement mediated hemolysis. Without those CDs there, the body attacks the red cells.
A 55 year old male patient comes to see you for yearly follow up. He is generally feeling well. He notes occasional LUQ abdominal pain, upon further questioning he realizes that sometimes he has started to feel full soon after eating (early satiety). His Hb is 15g/dL, platelets are 400,000/uL and his WBC is 90x10 9/L, mostly neutrophils in the peripheral smear. You send a test looking for which translocation to confirm the diagnosis of chronic myelogenous Leukemia.
What is BCR-ABL translocation or the philidelphia chromosome.
MPN:
CML- high wbc
BCR-ABL negative MPN:
PV (high Hb, Jak2+nearly all pts)
ET (high platelets) can see Jak2 50%
Myelofibrosis usually anemia, splenomegaly, tear drops, Can be jak2 50%
You are seeing a 24 year old female for a history of thrombocytopenia. She states she has had mild thrombocytopenia her entire life. Her current platelet count is 70,000/uL. She reports she has easy bruising. You send for testing: Ristocetin induced platelet aggregation is decreased. Smear is below. What does she have?

What is Bernard-Soulier Syndrome.
(AR inheritance)
This is a side effect of high dose cyclophosphamide that can be prevented by giving mesna.
What is hemorrhagic cystitis.
40 yo M comes to doctors office because he has been feeling fatigued lately. Cbc shows a Hb of 6g/dL (12-15), WBC of 1.2x109/L (nl 4.5-10.5) and neutrophil count of 200/uL (0.2x109/L) (nl2.5-10.5), platelets of 11,000/uL (nl150-400). Reticulocyte count is very low. HE is sent emergently to the hospital. Bone marrow biopsy shows a hypocellular marrow with fatty infiltration. What is the diagnosis?

Aplastic Anemia
-can be induced by medications (carbemazepine, benzene, nsaids, methimazole),viral, idiopathic
A 23 year old male with HbSS disease comes to the hospital with shortness of breath and chest pain. He has a temperature of 102F. O2 sat is 82% on Room air. With O2 he is at 88%. He looks uncomfortable when breathing. Chest Xray shows bilateral infiltrates at the bases. His Hb is 8g/dL (normal 12-15), his usual baseline is 9g/dL. The MICU is called and they are considering intubation given his respiratory distress. In addition to antibiotics and respiratory management, what is the best management for this patient with sickle cell disease?
He has acute chest syndrome. Best management is exchange transfusion.
38 year old female comes to the hospital with headaches and generalized malaise over last 1 week. Hb is 9g/dL ( normal 12.5-15), platelets of 52,000 plt /uL (normal 150-400). They were normal 2 months ago at her PCP office. Schistocytes are identified on peripheral blood smear and you think this could be thrombotic thrombocytopenia purpura and decide to look for this deficiency:
What is AdamTS13
What does AdamTS do?
A 60 year old man has had CLL(chronic lymphocytic leukemia) for many years. He has had mild lymphadenopathy in the neck for 5 years now. Over the last 3 months, he notices increasing fevers, night sweats, weight loss and fatigue. He also notes that the lymph nodes in his neck and axilla are growing. PET scan shows significant progression of lymphadenopathy since last scan and newly active lesions and biopsy of the lymph nodes show aggressive disease. His doctor notes the change in his diagnosis and tells him he will need systemic chemotherapy for his now aggressive B cell lymphoma called this.
What is Richters Transformation (when CLL transforms to DLBCL).
What coagulation factor is low in Von Willebrands disease and why?
Factor VIII because von willebrand keeps VIII in circulation. without it , it is degraded.
Imatinib massively changed the prognosis of which hematologic disease?
CML
Imatinib is a tyrosine Kinase inhibitor against BCR-ABL