The two fundamental approaches to manage atrial fibrillation
What are
a. rhythm control
b. rate control
What group of pathogens causes croup?
How do we treat croup?
What is viral?
Steriods
for inspiratory stridor we give racemic inhaled epinephrine
steroid
eye lubricant
The primary cause of death from a pelvic fracture is
A. Associated injuries
B. Blood loss
C. Ruptured diaphragm
D. Sepsis
What is
B. blood loss
How do I determine BP goals in a stroke patient?
1. Ischemia or bleed?
-Bleed: <140mmHg systolic
-Ischemia ->
-Using TPA?: goal <180mmHg systolic
-No TPA?: Don't do anything unless >220mmHg
I should do this if I think my patient is hemodynamically unstable BECAUSE OF their rapid afib.
What is electrically Cardiovert?
I recommend a small dose of etomidate if you can.
Then SYNCHRONIZE.
Then 200J. -> 300J if that doesn't work.
60M PMH ESRD on nightly peritoneal dialysis presents with fever and abdominal pain. What is the likely dx and what do you do?
What is SBP?
Sample the dialysate fluid.
Go ahead and treat with ABx through PD catheter.
Usually ceftazidime +/- vancomycin
ARDS is associated most strongly with...
A. Aspiration
B. Trauma
C. Sepsis
D. Massive blood transfusion
What is
C. Sepsis
...can happen in severe trauma as well
Your patient's dad calls because he has scant bleeding, coughed up a small dime sized area of blood. He's POD8 from outpatient T&A. What do you do?
What is the classic triad of lab findings in a patient was adrenal insufficiency (adrenal crisis)?
1. hyponatremia
2. hyperkalemia
3. hypoglycemia* most important clue, characteristic
These medications help provide RATE control for afib.
(Exception would be WPW but we are keeping it simple.)
What are
-calcium channel blockers (dilt & verapamil)
-beta blockers (metoprolol, esmolol, carvedilol)
-Dig
-Amio (might cardiovert though!)
-Don't forget Magnesium!
True or False
For a pregnant asthmatic patient in an exacerbation, great caution should be used when giving steroids.
False
The risk of not treating the asthma is more dangerous for mom & baby. Give the steroids unless the exacerbation is very mild.
These patients get vaccinated for pneumococcal PNA.
Who are...
Alcoholics, cigarette smokers, COPD, HF, DM, immunocompromised, asplenic, >65 years old
Name 10 causes of pancreatitis. What are the top 2?
2. ETOH
3. viral
4. medication- antibiotics & diuretics
5. malignancy
6. hypertriglyceridemia
7. post ERCP
8. trauma
9. autoimmune
10. scorpions
Which of the following does not correspond to DIC.
A. Increased fibrinogen level
B. Decreased platelets
C. Schisotocytes
D. Anemia
E. Increased ddimer
What is
A. Increased fibrinogen level- this would actually be low
These medications provide RHYTHM control.
What is
-Amio (go to)
-propafenone (rhythmol)
-sotalol
-flecainide
-procainamide
-dofetilide (tikosyn)
What INCIDENTAL BP reading warrants ED referral?
<90mmHg systolic
>140mmHg systolic for pregnant patient over 20 weeks that's never had high BP before (but really call OB first for that)
Variables considered when classifying severity of a patient's asthma.
What are
-daily symptoms
-nocturnal awakenings
-frequency of using short acting beta agonist
-activity limitations
-lung capacity volumes
Which joint is the most commonly affected by septic arthritis in the following populations:
-IV drug users
-Kids
-Everyone else (most cases)
What is...
IVDU: sacroiliac, sternoclavicular, intervertebral
Peds: knee and hip
Everyone else: knee
Name 3 complications of diverticulitis.
1. abscess
2. perforation
3. obstruction
The usual treatment for incidentally found asymptomatic PVC's
What is nothing?
(Lyte derangements & hypoxia can cause PVC's & those should be addressed if the patient is sick. Context matters)
What is the most common cause of hypertensive encephalopathy?
A.DM
B. Hypertensive encephalopathy
C. prior ischemic stroke
D. ruptured berry aneurysm
Hypertensive encephalopathy
Most true about TB Skin Test:
A. It is positive in 100% of patients w/ TB meningitis.
B. Positive TBST = infection with Mycobacterium tuberculosis but not necessarily active disease
C. It is positive in 100% of patients infected w/ Mycobacterium tuberculosis
D. Criteria for interpreting a test as positive are universal for patients regardless of background/PMH
What is...
B. Positive TBST = infection with Mycobacterium tuberculosis but not necessarily active disease
How do we diagnose septic arthritis?
What is
Arthrocentesis
WBC 5K- 50K (Usually >40K, 75% PMNs)
A 44-year-old man presents to the ED with non-traumatic, unrelenting mid back pain for two days. He denies recent weight loss, history of cancer or IV drug use. He completed treatment for pneumonia one week ago. He notes that he cannot find a comfortable position and has been experiencing profuse night sweats. There is no radiation of the pain, bowel or bladder dysfunction, or neurological symptoms in the lower extremities. Vitals are: HR 118, BP 128/85, RR 18, T 39.0 C (102.2 F), SpO2 100%. On exam, he is diaphoretic and tender to palpation over the lower thoracic vertebrae. He has 5/5 strength and normal sensation in both lower extremities. What is the most appropriate next step in management?
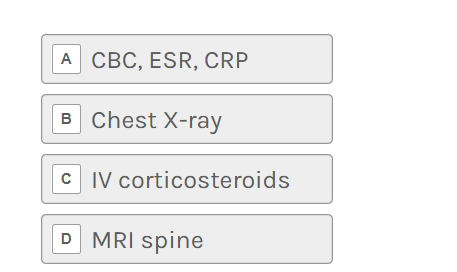
D. MRI of the spine
Management includes blood cultures for organism identification, long-term IV antibiotics, surgical drainage of any abscesses, and, in some cases, open debridement and decompression followed by spinal stabilization. WBC count is insensitive and non-specific. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are sensitive and can be used as a screening test in some patients with a low likelihood of having a serious infection, but these are likely to be positive in this case.
from EMRAP