A 62-year-old woman is seen for a preoperative evaluation before right knee arthroplasty. She has osteoarthritis of the knee and also has a history of rheumatoid arthritis. Medications are topical diclofenac, methotrexate, folic acid, and adalimumab. Other than the right knee, she reports no active joint symptoms; her rheumatoid arthritis is in remission.
On physical examination, vital signs are normal. There is chronic synovial hypertrophy of the metacarpophalangeal joints. Hand joints are not warm or swollen. There is medial joint line tenderness and crepitus in right knee.
Which of the following is the most appropriate perioperative medication management: Continue/Hold Methotrexate and Continue/Hold Adalimumab?
Continue methotrexate
Hold Adalimumab
All nonbiologic disease-modifying antirheumatic drugs should be continued throughout the perioperative period in patients with rheumatologic disease undergoing elective arthroplasty.
With the exception of patients with severe systemic lupus erythematosus, biologic agents should be withheld for one dosing cycle before arthroplasty, with surgery performed just after the next dose would have been due and resumed when the wound shows evidence of healing.
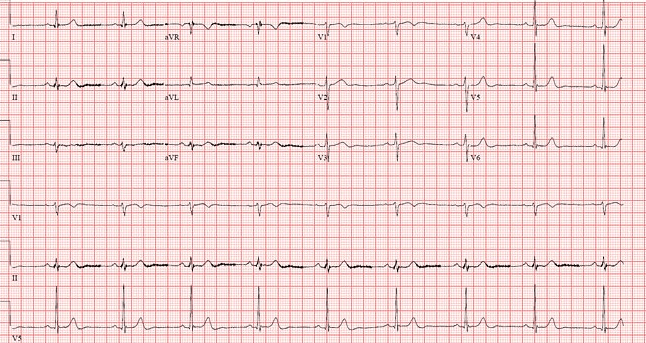
This infectious disease can sometimes lead to 3rd degree heart block.
Lyme disease, borrelia burgdorferi
B symptoms, hypercalcemia, Noncaseating granuloma on biopsy, hepatosplenomegaly

Bonus: Tell me the eponymic disease consisting of: fever, bilateral hilar lymphadenopathy, erythema nodosum, ankle arthritis.
Sarcoidosis
Lofgren syndrome
Remember, dont treat asymptomatic sarcoidosis.
The following physical exam finding is concerning for what disease.
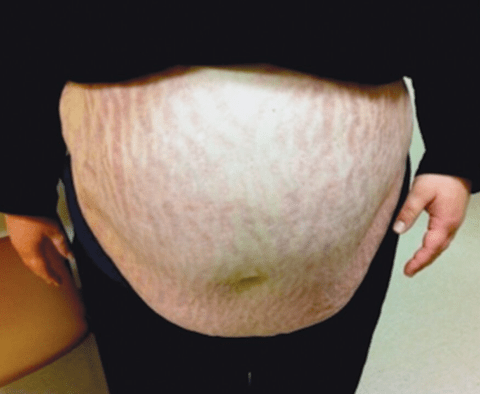
Cushings (hypercortisolism)
Which three characters did parkour all over the office?
Michael, Dwight, and Andy
A 42-year-old man is evaluated for fatigue, dyspnea, and lightheadedness. He was diagnosed with a provoked pulmonary embolism 5 months ago and has been taking apixaban since then. Initially, his dyspnea and tachycardia improved, but over the past 2 months, he has had progressive exertional dyspnea. On physical examination, vital signs are normal. BMI is 28. Cardiopulmonary examination is normal.
An echocardiogram reveals right atrial enlargement and right ventricular hypertrophy and an elevated mean pulmonary artery pressure.
Which of the following is the most appropriate diagnostic test? CTA Chest, D-Dimer, RHC and pulmonary angiography, VQ scan
VQ scan: A ventilation/perfusion scan is recommended for all patients with pulmonary hypertension to rule out chronic thromboembolic pulmonary hypertension.
For patients with suspected chronic thromboembolic pulmonary hypertension and an abnormal ventilation/perfusion scan, right heart catheterization and pulmonary angiography will confirm pulmonary hypertension, exclude competing diagnoses, and provide vital information related to potential therapy. Right heart catheterization and pulmonary angiography can be avoided in patients with a normal V/Q scan, and they should not be used as the initial tests in patients with suspected CTEPH.
CT angiography (CTA) of the chest (Option A) is capable of detecting chronic thromboembolic material within dilated central pulmonary arteries but is less sensitive than pulmonary angiography or V/Q scanning in detecting CTEPH.
List as many risk factors for the need to hospitalize someone with pericarditis
Bonus: give me the treatment of choice
Fever, subacute onset, large pericardial effusion, tamponade physiology/presentation, on oral AC, lack of response to typical therapy.
Bonus: High dose NSAID and cholchicine
Daytime Hypercapnea as defined by PCO2 greater than 45 mm Hg
This trial states that optimal blood sugar control in the ICU setting ranges from 140-180 (lower mortality as opposed to strict control of sugars)
NICE-SUGAR
What is the first prank Jim is seen pulling on Dwight?
He puts his stapler in Jell-O.
A 63-year-old man is evaluated during a follow-up visit for gastroesophageal reflux disease and heartburn. His symptoms are worse after large meals and when lying down and have significantly decreased the quality of his life and disrupted his sleep. He also has stage G4 chronic kidney disease, obesity, and hypertension. Medications are atenolol, lisinopril, and nifedipine. Laboratory studies show an estimated glomerular filtration rate of 29 mL/min/1.73 m2. Weight loss and other lifestyle management modifications for gastroesophageal reflux disease are discussed.
Which of the following is the most appropriate additional therapy? Famotidine, Omeprazole, Oral calcium and magnesium hydroxide, sucralfate
Famotidine: H2 blocker therapy can be considered for patients with advanced chronic kidney disease provided appropriate dosing is used.
Proton pump inhibitors may contribute to the development and progression of chronic kidney disease and should be avoided.
Patients with advanced CKD are at risk for magnesium toxicity with the use of these antacids and therefore should be avoided.
Sucralfate has no role in the treatment of GERD due to its short duration of action and reduced effectiveness compared with other therapies, including PPIs and H2 blockers.
In peripartum cardiomyopathy, which 3 classes of medications should be avoided?
ACEi
ARB
MRA
How long after radiation therapy does radiation pneumonitis occur (a range)?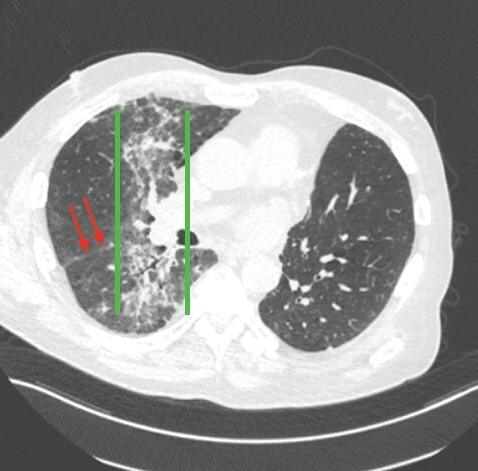
4-12 weeks
What is the biggest risk factor for the development of thyroid cancer?
History of ionizing radiation such as an adolescent who was treated for unrelated cancer with radiation.
What was the disease that the staff participated in a race to help cure?
Bonus: tell me the post exposure treatment for someone who has not been vaccinated who was bit by a dog suspected to have this disease.
Bonus 2: Tell Me the full name of the race
Rabies
Bonus: rabies vaccine (active) and rabies immune globulin (passive) ASAP.
Bonus 2: Michael Scott's Dunder Mifflin Scranton Meredith Palmer Memorial Celebrity Rabies Awareness Pro-Am Fun Run Race for the Cure
A 60-year-old man is evaluated for a 1-year history of lower extremity edema. He has a 30-year history of poorly controlled ankylosing spondylitis. He also has intermittent uveitis. His only medication is naproxen; he has been reluctant to initiate biologic agents.
On physical examination, blood pressure is 158/90 mm Hg. Other vital signs are normal. He has kyphosis with immobility of the cervical, thoracic, and lumbar spine. There is decreased range of motion of the shoulders and hips with 30-degree flexion contractures at both hips. There is 2+ bilateral swelling of the lower extremities.
Albumin 2.5 g/dL, C-reactive protein 6.3 mg/dL, Creatinine 1.8 mg/dL, Protein-creatinine ratio 5200 mg/g.
Urinalysis 3+ protein; no erythrocytes, leukocytes, casts, or eosinophils
What is the most likely diagnosis?
Renal Amyloidosis: Patients with long-standing, poorly controlled ankylosing spondylitis can develop renal (AA) amyloidosis, the major cause of kidney disease in these patients. AA amyloidosis most commonly affects the kidneys, manifesting as proteinuria and, eventually, renal insufficiency.
Analgesic nephropathy may develop after years of NSAID use and typically presents with abnormalities on routine urinalysis, including pyuria, proteinuria, and hematuria. Chronic kidney disease and end-stage kidney disease can develop in some patients. This patient's urine findings are not compatible with analgesic nephropathy.
This medication should be added to patients with HFrEF on maximally titrated GDMT in normal sinus rhythm with a pulse >70
Bonus: if you can tell me its mechanism of action
Ivabradine, a sinoatrial node modulator that selectively inhibits the If current in the sinoatrial node, causing a reduction in heart rate. It has no negative inotropic effects.
What are the 3 most common causes of pleural effusions in the USA.
HF, Pneumonia, Malignancy.
Give me the expected lab values for someone with primary adrenal insufficiency (AM cortisol, ACTH, Na, K).
Bonus: Tell me the most common cause of primary adrenal insufficiency.
AM cortisol low, ACTH High, Na low, K high
Bonus: autoimmune adrenalitis leading to the progressive destruction of all cortical layers
How many minutes did Michael Scott work at the office?
9,986,000 minutes.
A 50-year-old man is evaluated for newly developed ascites. He has cirrhosis due to nonalcoholic steatohepatitis. Paracentesis confirms cirrhosis as a cause of the ascites and excludes infection, and a low-sodium diet is implemented. Medical history includes type 2 diabetes mellitus, hypertension, and dyslipidemia. Current medications are metformin, lisinopril, and atorvastatin.
On physical examination, vital signs are normal. The abdomen is nontender and mildly distended, with normal bowel sounds.Serum creatinine level is 1.1 mg/dL. Random urine protein-creatinine ratio is 16 mg/g.
Which of the following is the most appropriate additional treatment? d/c atorvastatin, d/c lisinopril, start lactulose, start a low protein diet.
Discontinue Lisinopril: Medications that decrease renal perfusion pressures, such as ACE inhibitors, can worsen ascites in patients with portal hypertension.
β-Blockers and NSAIDs should be used with caution or discontinued in patients with portal hypertension and ascites.
Cirrhotics need a HIGH protein diet
Statins for the treatment of dyslipidemia may increase hepatic aminotransferase levels. However, the overall benefits of these medications typically outweigh the potential harms, especially in patients with risk factors for coronary artery disease, such as in this patient with nonalcoholic steatohepatitis, type 2 diabetes, dyslipidemia, and hypertension. Therefore, discontinuation of atorvastatin is not appropriate.
Nonabsorbed disaccharides, such as lactulose (Option C), are initiated for the management of hepatic encephalopathy. This manifestation of cirrhosis can develop in the same population as patients with ascites. However, this cathartic is poorly tolerated and should not be initiated in a patient without symptoms referable to hepatic encephalopathy.
An 84-year-old man is evaluated during a routine physical examination. His only concern is a gradual loss of stamina and low energy. He can no longer complete his routine 2-mile run without stopping to rest with a prolonged recovery time. He has hypertension, for which he takes lisinopril.
On physical examination, blood pressure is 125/78 mm Hg and pulse rate is 52/min. Heart rate is regular. The remainder of the examination is unremarkable.
Laboratory studies are within normal limits, including a recent thyroid-stimulating hormone measurement.
Ambulatory 48-hour ECG monitoring shows a maximum heart rate of 72/min during vigorous aerobic activity. An echocardiogram and exercise stress test performed 1 year ago for chest pain revealed normal left ventricular function and no ischemia, with appropriate augmentation of heart rate.
Pacemaker Implantation
A 72-year-old man is evaluated in the emergency department for decreasing responsiveness after he spent the day at the zoo. The outside temperature was 38.9 °C (102.0 °F). He also has hypertension. Medications are hydrochlorothiazide and lisinopril.
On physical examination, temperature is 40.5 °C (104.9 °F), blood pressure is 97/54 mm Hg, pulse rate is 117/min, respiration rate is 22/min, and oxygen saturation is 96% with the patient breathing ambient air. He is somnolent. His skin is flushed, warm, and dry. Other than tachycardia, cardiac and pulmonary examinations are normal.
Evaporative Cooling
Dont do immersion in ice water in the elderly, there is an increased mortality risk.
List 5 symptoms of hypocalcemia
Bonus: give me the 2 eponymic physical exam findings associated with hypocalcemia and tell me how to perform
laryngospasm, seizure, myocardial dysfunction, QT prolongation, paresthesia, perioral numbness, carpopedal spasm and muscle cramps, facial nerve hyperirritability.
Bonus: Trousseau' Sign, carpopedal spasm with characteristic hand posture (flexion at metacarpophalangeal joints and extension at interphalangeal joints) may be spontaneous or triggered by transient distal limb ischemia during blood pressure assessment. Chvostek's Sign, facial nerve hyperirritability and muscle spasm can be demonstrated by percussion of the facial nerve just anterior to the ear.
How much money did Jim spend on his outfit to imitate Dwight?

$11