What wound qualifications are needed for foam dressings?
Medicare advantage plans only need moderate/heavy exudate and depth (at this time)
What identifier do all Medicare policy numbers share?
Prefixes are MEB
What Humana plan type needs called at least once per plan year? What are we checking for?
HMO policies. If a PCP referral is required.
How do we determine our network status and guidelines for BCBS plans?
Refer to the state the patient lives in and contact card.
Which Tricare plan type does deductible not apply?
POS plans
We have an invalid policy number for a patient. What other pieces of information can we use to search for eligibility using the UHC portal?
First name, last name, group number, date of birth
In which circumstance we are we considered OON provider?
On certain EPO/Employer Sponsored plans.
What is a PCP Referral?
A PCP Referral is an authorization the PCP doctor/office must submit for Prism to provide services to the patient. The PCP office coordinates care.
Which policies require modifiers?
Policy ID's with A, AN, or M outside of the 3 letter alpha prefix; if Medicare is secondary; or if compressions are being shipped.
DOUBLE JEOPARDY - What guidelines do Tricare policies follow?
Physician's orders
In what situation are compressions are covered with UHC Medicare policies?
Open venous stasis ulcer (I codes), Stocking below knee, Compression greater than 30mmHg,less than 50mmHg
Why do we call on commercial policies?
Supplies are sometime considered disposable and OTC.
What is the line item limit for all Humana policies?
$750
DOUBLE JEOPARDY - Name 4 BCBS plans utilize Integra Partners?
BCBSNY, BCBSCT, BCBSME, and BCBSNH
If we see Tricare for Life while verifying coverage, what insurance should be primary?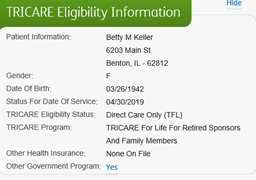
Medicare
What Noble insurance ID should this insurance have?

UHC Community of Florida
Which portals can be used to verify coverage?
Availity and Navinet
What item is non-covered under insurance no matter the circumstance?
Compressions – wraps or stockings.
What BCBSSC plans do we send to processing?
Plans that use to Blue Essentials network, Ostomy and Urology orders, BCBSSC MDCD, and BCBSSC Medicare policies.
Medicare is primary. Tricare is secondary. The physician has ordered daily use of Simpurity foam dressings. How many foam are we able to send?
30. Tricare will pay for the additional foam outside of Medicare guidelines IF deductible is met.
DOUBLE JEOPARDY - Which 3 community plans do we ship without submitting authorization due to payment history?
UHCCOMMFL, UHCCOMMTN, UHCCOMMVA
True/False: Compressions are non-covered and pricing must be offered?
False. There are certain criteria in which compressions are deemed as covered items. Please see contact card for this information.
What state typically requires a PCP referral?
Florida
True or False: We offer pricing for both Medicare and Commercial plans for BCBSMI?
False. Commercial policies do not cover supplies. Pricing needs offered.
Medicare is primary. Tricare for Life is secondary. The physician has ordered daily use of Tegaderm Film. How many film can we send?
12. Tricare for Life is a supplemental policy and does NOT pay for additional supplies.