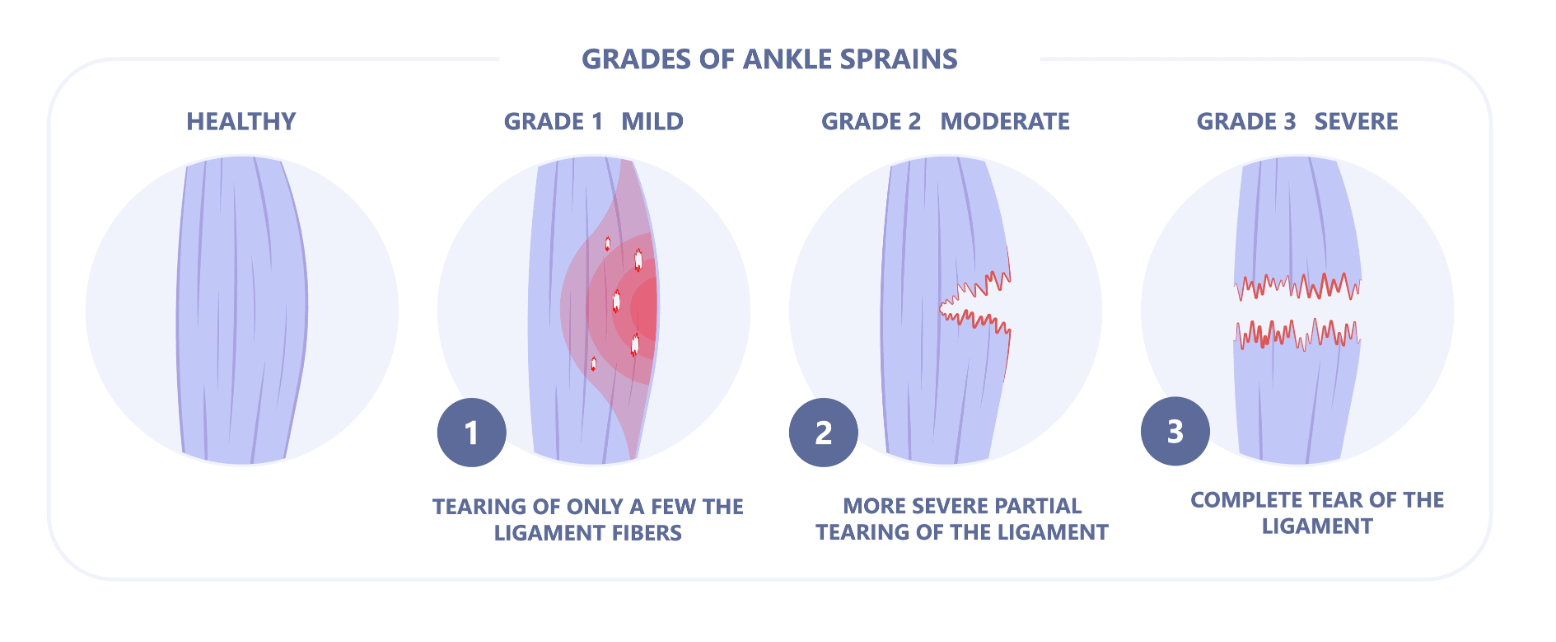
What is the name of an injury to the ligaments that surrounds the joints?
SPRAIN- wrenching or twisting motion that occurs at the ankle, wrist, and knee joints. Three degrees of damage
FIRST- mild tenderness and minimal swelling
SECOND- moderate partial disruption involving the tissue more swelling and tenderness
THIRD- severe complete tear of the ligament severe swelling
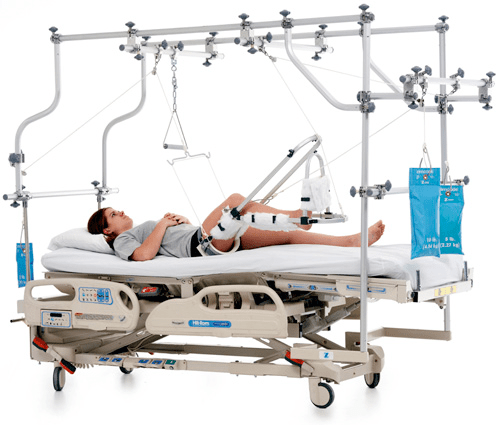
What is the application of a pulling force to an injured or diseased body part?
TRACTION- 1 used to prevent or reduce pain and muscle spasms (Whiplash, unrepaired hip fracture) 2 immobilize a joint or part of the body 3 reduce a fracture or dislocation 4 treat a pathologic joint condition
Traction can also (1) provide immobilization to prevent soft tissue damage, (2) promote active and passive exercise, (3) expand a joint space during arthroscopic procedures, and (4) expand a joint space before major joint reconstruction.
Traction devices apply a pulling force on a fractured extremity to attain realignment, while countertraction pulls in the opposite direction.

Traction weights are usually 5 to 10 lb (2.3 to 4.5 kg). Buck’s traction is a type of skin traction sometimes used for the patient with a hip, knee, or femur fracture
Skeletal traction is used to align injured bones and joints or to treat joint contractures and congenital hip dysplasia. It provides a long-term pull that keeps the injured bones and joints aligned. To apply skeletal traction, the HCP inserts a pin or wire into the bone, and weights are attached to align and immobilize the injured body part. Weight for skeletal traction ranges from 5 to 45 lb (2.3 to 20.4 kg). Too much weight can result in delayed union or nonunion. The major complications of skeletal traction are infection at the pin insertion site and the effects of prolonged immobility.
Acute Care SPRAINS & STRAINS
RICE- (Rest, Ice, Compression, Elevation) this will decrease local inflammation and pain for most musculoskeletal trauma injuries. Movement should be restricted and the extremity should be rested once pain is felt
Traction Care
WEIGHTS CANNOT TOUCH THE FLOOR
Perform neurovascular assessments
Assess for compartment syndrome- swelling with increased pressure within a limited space treated with fasciotomy
Determine the patient's correct body alignment to enhance the traction
Teach patient ROM exercises
Assess for complications associated with immobility
Pain Management
infection, constipation, VTE, atelectasis, renal calculi
Which discharge instruction would the emergency department nurse include for a patient with a sprained ankle?
- Keep the ankle loosely wrapped with gauze.
- Apply a heating pad to reduce muscle spasms.
- Use pillows to elevate the ankle above the heart.
- Gently move the ankle through the range of motion.
Excessive stretching of a muscle?
STRAIN- Excessive stretching of a muscle and its fascial sheath, often involving the tendon
occurs in large muscle groups, lower back, calf, and hamstrings
classified as (1st degree, 2nd degree, and 3rd degree)
symptoms includes pain, edema, deceased in function, and bruising
Mild strains takes 3-6 weeks to heal
Severe strains may need surgical repair
Amputation
The removal of a body extremity by trauma or surgery
About 185,000 amputations occur each year in the United States. Just over half are due to PVD and diabetes. These patients often have peripheral neuropathy that progresses to deep ulcers and gangrene. Trauma is the other major cause. Injuries have affected over 1700 military veterans since 2003, with several losing more than 1 limb.16 Other reasons for amputation include thermal injuries, tumors, osteomyelitis, and congenital limb disorders.

Forms of Nursing care Sprain/Strain
Cryotherapy- cold causes vasoconstriction and reduces the transmission and perception of nerve pain impulses
Cold is applied immediately after an injury has occurred used for 24-28 hours, apply ice no more than 20-30 mins at a time DO NOT APPLY ICE DIRECTLY TO THE SKIN
Compression will decrease edema and pain and elastic compression bandage is usually utilized and wrapped around the injured part. If the bandage is wrapped too tight there may be numbness and tingling below the compressed area. Leave the bandage in place for 30 mins and then remove it for 25 mins
Elevate the injured part above heart level even during sleeping for 24-48 hours. This helps to mobilize excessive fluid from the area and prevents further edema NSAIDs may also be used to manage pain and discomfort
Amputation care (Lower extremity)
Inspect the residual limb daily for signs of skin irritation, especially redness, abrasion, and odor. Especially evaluate areas prone to pressure.
2. Stop using the prosthesis if irritation develops. Have the area checked before resuming use of the prosthesis.
3. Wash the residual limb thoroughly each night with warm water and bacteriostatic soap. Rinse thoroughly and dry gently. Expose the residual limb to air for 20 min.
4. Do not use lotions, alcohol, powders, or oil on residual limb unless prescribed by the HCP.
5. Wear only a residual limb sock in good condition and supplied by the prosthetist.
6. Change residual limb sock daily. Launder in mild soap, squeeze, lay flat to dry.
7. Use prescribed pain management techniques.
8. Perform ROM to all joints daily. Perform general strength exercises (including for upper extremities) daily.
9. Do not elevate residual limb on a pillow.
10. Lay prone with hip in extension for 30 min, 3 or 4 times daily.
The nurse is caring for a patient who has a pelvic fracture and an external fixation device. Which method would the nurse use to assess pressure areas and provide skin care to the patient’s back and sacrum?
- Ask the patient to turn to the side independently.
- Defer back assessment until the patient is ambulatory.
- Have the patient lift the back and buttocks using a trapeze bar.
- Roll the patient over to the side by pushing on the patient’s hips.

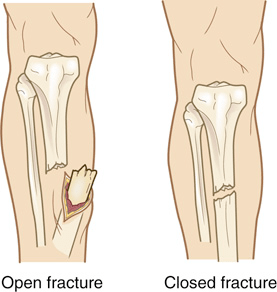
A disruption or break in the bone
FRACTURE- described as open or closed
open- skin is broken and bone is exposed
closed skin is intact over the site
complete- break goes through the bone or incomplete- occurs partly across the bone shaft but the bone is still intact
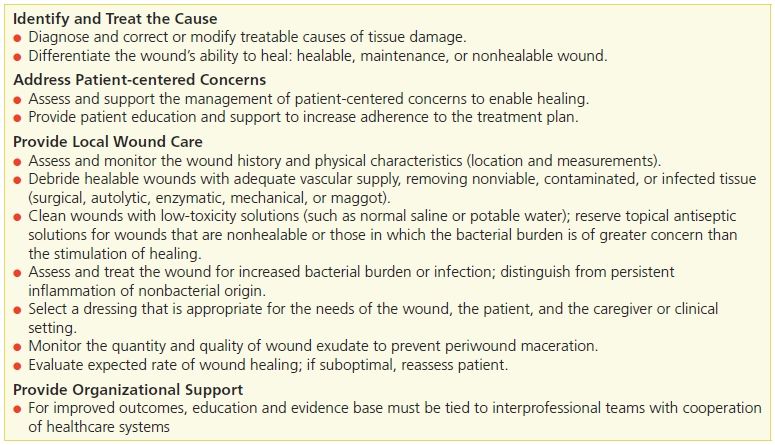
Debridement
Debridement is the removal of debris, such as pieces of bone or cartilage (loose bodies) or osteophytes, from a joint using a fiberoptic arthroscope. This procedure is usually done on an outpatient basis on the knee or shoulder. A compression dressing is applied after surgery. Weight bearing is permitted after knee arthroscopy. Patient teaching includes monitoring for signs of infection, managing pain, and restricting activity for 24 to 48 hours.
Closed- Fracture
CLOSED REDUCTION- is the nonsurgical, manual realignment of bone fragments to their anatomic position. Traction and countertraction are manually applied to the bone fragments to restore position, length, and alignment. Closed reduction is usually done while the patient is under local or general anesthesia.
Traction, casting, splints, or orthoses (braces) may be used after reduction to maintain alignment and immobilize the injured part until healing occurs.
Debridement
A patient who is to have no weight bearing on the left leg is learning to use crutches. Which observation by the nurse indicates the patient can safely ambulate independently?
- The patient moves the right crutch with the right leg and then the left crutch with the left leg.
- The patient advances the left leg and both crutches together and then advances the right leg.
- The patient uses the bedside chair to assist in balance as needed when ambulating in the room.
- The patient keeps the padded area of the crutch firmly in the axillary area when ambulating.
Description of fractures
Displaced- 2 ends of the broken bone is separated from each other and out of their normal position (Comminuted, Oblique)
Nondisplaced- bone fragments stay in alignment (Transverse, Spiral, Greenstick)
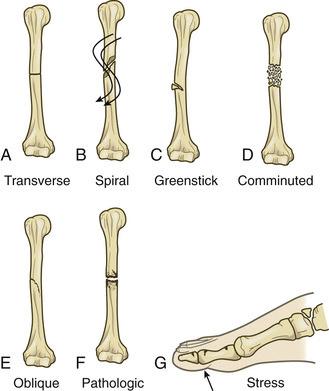
Types of fractures. (A) Transverse fracture: the line of the fracture extends across the bone shaft at a right angle to the longitudinal axis. (B) Spiral fracture: the line of the fracture extends in a spiral direction along the bone shaft. (C) Greenstick fracture: an incomplete fracture with 1 side splintered and the other side bent. (D) Comminuted fracture: a fracture with more than 2 fragments. The smaller fragments appear to be floating. (E) Oblique fracture: the line of the fracture extends across and down the bone. (F) Pathologic fracture: a spontaneous fracture at the site of a diseased bone. (G) Stress fracture: occurs in bone that is subject to repeated stress, such as from jogging or running.
Fat embolism syndrome (FES) is characterized by fat globules entering the circulatory system from fractures. FES contributes to mortality from fractures. The fractures most often associated with FES are those of the long bones, ribs, tibia, and pelvis. They collect in areas with abundant blood vessels, especially the lungs and brain.
These include chest pain, tachypnea, cyanosis, dyspnea, apprehension, tachycardia, and hypoxemia. These symptoms are caused by poor O2 exchange.
Rhabdomyolysis is a syndrome caused by the breakdown of damaged skeletal muscle cells. This breakdown causes the release of myoglobin into the bloodstream. Myoglobin precipitates and causes obstruction in renal tubules. This results in acute tubular necrosis and acute kidney injury (AKI). Because of possible muscle damage, assess urine output. Common signs are dark reddish-brown urine and symptoms of AKI
Phantom limb
Tell the patient that the amputated limb may feel like it is still present after surgery. This phenomenon, termed phantom limb sensation, occurs in many amputees.
Open- fracture
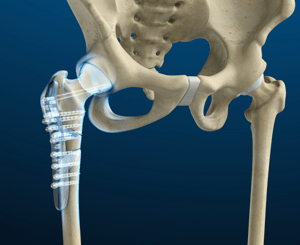
OPEN REDUCTION (ORIF)- is the correction of bone alignment through surgery. It usually includes internal fixation of the fracture with wires, screws, pins, plates, intramedullary rods, or nails. The type and location of the fracture, patient age, and concurrent disease influence the decision to use open reduction.
Phantom Limb
To meet the patient’s educational needs, know the level of amputation, type of dressings to be applied, and type of prosthesis to be used. Teach the patient to perform upper extremity exercises, such as push-ups in bed or the wheelchair, to promote arm strength for crutch walking and gait training. Discuss general postoperative nursing care. Review positioning, support, and residual limb care. If a compression bandage will be used after surgery, teach the patient about its purpose and how it will be applied
Mirror therapy, VR reality treatment give visual information to the brain, replace sensory feedback expectations about the missing limb
 Based on the information in the accompanying figure obtained for a patient in the emergency room, which action would the nurse take first?
Based on the information in the accompanying figure obtained for a patient in the emergency room, which action would the nurse take first?
- Administer the prescribed morphine 4 mg IV.
- Contact the operating room to schedule surgery.
- Check the patient’s O2 saturation using pulse oximetry.
- Ask the patient the date of the last tetanus immunization
Fracture healing phases
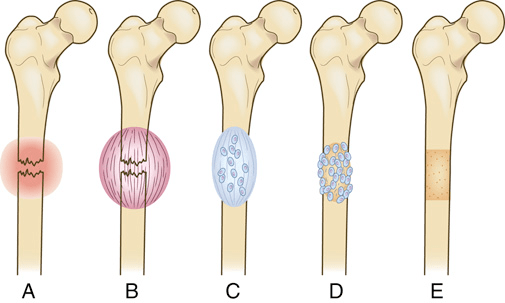
FIG. 67.8 Bone healing (schematic representation). (A) Bleeding at fractured ends of the bone with hematoma formation. (B) Organization of hematoma into fibrous network. (C) Invasion of osteoblasts, lengthening of collagen strands, and deposition of calcium. (D) Callus formation: new bone is built up as osteoclasts destroy dead bone. (E) Remodeling is accomplished as excess callus is resorbed and trabecular bone is laid down.
Fractures involving the shaft of the humerus are common among young and middle-aged adults. The most common symptoms are obvious displacement of the humeral shaft, shortened extremity, abnormal mobility, and pain. Complications include radial nerve injury and injury to the brachial artery due to laceration, transection, or muscle spasm. Nonoperative treatment may include a hanging arm cast, shoulder immobilizer, sling and swathe (a type of immobilizer that prevents shoulder movement)
The clavicle is a frequently broken bone in children and young adults. Midshaft fractures account for 85% of all clavicle fractures. Injury is usually the result of a fall. Less often it happens from direct trauma to the bone.
Pelvic fractures range from relatively minor to life threatening, depending on the mechanism of injury and associated vascular damage. They account for only 3% of adult fractures. Pelvic fractures have a high mortality rate. They may cause serious intraabdominal injury, including laceration and hemorrhage of the urethra, bladder, or colon. They can cause acute pelvic compartment syndrome. Paralytic ileus may occur after pelvic fracture. Patients may survive the pelvic injury, only to die from sepsis, FES, or VTE.
Hip fractures are common in older adults. 95% of hip fractures result from a fall.14 Many falls occur when getting in or out of a chair or bed. Falls to the side are the most common type seen in frail older adults.
Immediate surgery is the standard of care. Initially we may immobilize the affected extremity with Buck’s traction
Infection
Infection is a serious complication of joint surgery, especially joint replacement surgery. The most common causative organisms are streptococci and staphylococci. Infection may lead to pain and loosening of the prosthesis, often requiring further surgery.
Open Fracture Risks
The main risks of open reduction are infection, complications of anesthesia, and effects of preexisting medical conditions (e.g., diabetes). However, open reduction internal fixation (ORIF) facilitates early ambulation, decreasing the risk for complications related to prolonged immobility.
Infection
Measures to reduce infection include the use of specially designed self-contained operating suites, operating rooms with laminar airflow, and prophylactic antibiotic administration.
When a patient arrives in the emergency department with a facial fracture, which action would the nurse take first?
- Assess for nasal bleeding and pain.
- Apply ice to the face to reduce swelling.
- Use a cervical collar to stabilize the spine.
- Check the patient’s alertness and orientation.