Describe three options for mechanical loading, other than strengthening activities.
Functional activities
Weight bearing
Gravity
Describe how immobilization affects joint structures.
For joint structures, immobilization means no loading, and therefore they won’t secrete or go through deformation.
Describe Wolff’s Law in the context of tissue structure and function.
“The more stress you place, the more the tissue will respond by growing/remodeling.”
Cartilage has a small cellular component and a large ECM/interfibrillar component. Describe how this relates to cartilage function.
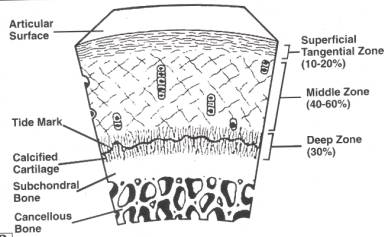
Large ECM is full of PG and GAG, which the cartilage needs to maintain rigid structure. This rigid structure provides a lot of support for weight-bearing and distribution of compressive loads. Cell count is low with no alignment, so cartilage has a limited ability to repair itself.
___ bone is stronger/stiffer and gives the skeleton its strength to withstand load. (Ultimate strength = threshold)
___ bone reduces load/impact and is found around joints that needs protection. Higher % of deformation
Cortical, trabecular
In ligaments, describe how the ratio of collagen to elastin accounts for different functions at a specific joint.
Ratio of collagen/elastin accounts for the relative abilities to provide stability (collagen) and allow for mobility (elastin) at a joint.
What function does the structure of collagen’s tropocollagen triple helix molecule serve? What is the term for the wavy arrangement of these fibers?
The tropocollagen “braid” resists tensile forces more. In most relaxed tissues, the fibers have a wavy composition called crimp.
Why do we need mechanical load for collagen production?
Mediates how much degradation vs. production in the tissue
Mechanical force mediates the collagen degradation rate, which then initiates and alters the remodeling and repairing process of collagen-based materials.
Why do certain tissues like cartilage have increased concentration of PGs?
PGs are increased in tissues subjected to alternating cycles of compression!
What component of bone tissue gives it structure (inorganic or organic)? How does this differ from the other tissues’ structures?
Inorganic component → crystallized matrix → crystals of hydroxyapatite
Other tissues maintain structure through organic components (osmotic pressure, PGs)
What are the two types of enthesis and where are each located? What is the function of entheses?
Fibrous enthesis: cemented into mostly cortical bone via Sharpey's fibers (Collagen bundles that extend from the tendon/ligaments into the bone)
Fibrocartilaginous enthesis: short bones, transitional tissue
Anchor to the bone with high role in stress dissipation
What will happen if there is too much mechanical loading to one joint area?
If too much loading, too many cells will go to the area and therefore cause too much degradation. This will delay the building of tissue because of inflammation.
How do structure and function determine a tissue’s material properties/ vice versa?
Form determines overall structure, but the characteristics of the tissue are affected by functional use. Type of collagen/crosslinks/PG type and amount are affected by the type and amount of stress applied to tissue. The size of tissue will determine the types of loads the tissue can bear.
Where is the tidemark located in cartilage, and what is its role in endochondral ossification?
The tidemark is located between the calcified and noncalcified cartilage. It is the point for healing, aging, and growth.
True or false: bones and tendons are both avascular.
False: bones are very vascular (periosteum). And some tendons are considered vascular if they have a paratenon like the Achilles tendon. A bone grows AND remodels in response to the forces that act upon it. Therefore, bone adapts its mechanical properties according to the needed mechanical function.
While tendons and ligaments have similar structures, what are the main structural differences between the two? (3)
Tendons have mostly Type I collagen for strength, and have more Type I than ligaments.
Tendons have less Type III (tendon sheath)
Tendon fibers follow the direction of muscle contraction while ligament fibers align parallel to ALL the imposed forces.
How do the PGs in the ECM (interfibrillar matrix) affect hydration?
The PGs in the ECM affect hydration through attached GAGs. GAG chain attracts water into interfibrillar matrix/ECM, creating tensile stress on surrounding collagen network. Collagen fibers resist and contain the swelling, thus increasing the rigidity of the ECM.
Explain creep and how it affects joint structure and function.
Creep - CT gradually elongates after an initial elastic response to a constant tensile load. Then, it gradually returns to original length after load is removed.
Example: when you hang a weight on the end of an elastic band, you get immediate elastic deformation
It will also gradually elongate further over time
Take us through the deformation over time curve. (picture)
Goal - equilibrium of hydrostatic pressure. Curve represents deformation over time.
Lots of fluid/ground substance
Black arrows = water/ground substance moving out through semipermeable membrane bc of compressive force.
At equilibrium there is no exudation (white bar equals creep, or change that occurs when you apply load)
What negatively affects the integrity of a bone? What increases it?
Disuse, inactivity, weightlessness, age
To increase: Mechanical and non- mechanical factors
How do the fascicles of the tendons interact with motor units?
Each fascicle of the tendon is associated with a discrete group of muscle fibers or motor units at the muscle-tendonjunction.
Several fascicles may form a larger bundle that also is enclosed in the endotenon
Concept map: How does ECM play a key role in force transmission and tissue structure maintenance?
ECM turnover influenced by mechanical loading → quantity of PG/GAGs affects tissue hydration → tissue’s tensile and compressive strength → rigidity of the tissue
Describe viscoelasticity.
Viscoelasticity is the material’s ability to deform under tensile/compressive loads and return back to its original state once the force is removed. The viscous qualities (resistance to flow) make the deformation and return time-dependent.
Describes the steps of stress loading/area on cartilage, starting with the initial compressive load.
Aggregating PGs attract a large volume of water, which increases osmotic swelling pressure in the cartilage. PGs stiffen into the surrounding collagen network and ECM expands, creating tension. This creates an opposing force that keeps PGs and water contained. Equilibrium is reached between swelling pressure and the load on the joint. Deformation stops.
What does cancellous bone form in response to stress/load? (structure and function)
-form trabeculae or "spongy tunnels" (trabecular, spongy bone)
-Found at the surfaces to distribute loading forces
-cancellous bone is covered by a layer of dense, compact cortical bone, which is laid down in concentric layers.