What does the letter of RNS HOPE acronym means when doing a health assessment.
• Rest and activity
• Nutrition, fluids, and electrolytes
• Safety and security
• Hygiene and grooming
• Oxygenation and circulation needs
• Psychosocial and learning
• Elimination
Which of these breath sounds is considered normal and not adventitious?
1) Vesicular breath sounds
2) Fine rales
3) Rhonchi
4) Wheezes
1
Vesicular breath sounds are normal breath sounds. Rales, fine and coarse, rhonchi and wheezes are all abnormal, adventitious breath sounds.
A client arrives in the emergency room with a possible fractured femur. The nurse should anticipate an order for:
A. Trendelenburg position
B. Ice to the entire extremity
C. Bucks traction
D. An abduction pillow
C. Bucks traction
The client with a fractured femur will be placed in Bucks traction to realign the leg and decrease spasms and pain.
The protrusion of an internal organ through a wound or surgical incision is referred to as:
1) Serosanguineous.
2) Dehiscence.
3) Evisceration.
4) Exuded.
3
Evisceration, or the protrusion of an organ through a wound, most often occurs in the abdominal wall. Serosanguineous describes the thin, red exudate produced by a surgical wound and dehiscence is the separation of a surgical incision. Exuded is another name for discharged in reference to the exudate.
The nurse is collecting data from a client who has had benign prostatic hyperplasia (BPH) in the past. To determine whether the client is currently experiencing exacerbation of BPH, the nurse should ask the client about the presence of which early symptom?
A) Nocturia
B) Urinary retention
C) Urge incontinence
D) Decreased force in the stream of urine
D
Rationale: Decreased force in the stream of urine is an early sign of BPH. The stream later becomes weak and dribbling. The client may then develop hematuria, frequency, urgency, urge incontinence, and nocturia. If untreated, complete obstruction and urinary retention can occur.
Test-Taking Strategy: Note the strategic word, early.
What is this? When and How would you as the nurse use it?

Need an order to give a suppository,
Constipation (what is the definition of constipation)
Can suppository be given only rectally? (remember they can be given in an ostomy also)
Left Sims is the preferred position
What is the nurse assessing for in this visual exam.
Accommodation
The nurse is caring for a client with emphysema receiving oxygen. The nurse should consult with the registered nurse if the oxygen flow rate exceeded how many L/min of oxygen?
A) 1 L/min
B) 2 L/min
C) 6 L/min
D) 10 L/min
B)
Rationale: Between 1 L/min and 3 L/min of oxygen by nasal cannula may be required to raise the PaO2 level to 60 mm Hg to 80 mm Hg. However, oxygen is used cautiously in the client with emphysema and should not exceed 2 L/min unless specifically prescribed. Because of the long-standing hypercapnia that occurs in this disorder, the respiratory drive is triggered by low oxygen levels rather than by increased carbon dioxide levels, which is the case in a normal respiratory system.
Test-Taking Strategy: Focus on the subject, oxygen administration with emphysema
A 20-year-old patient with a 6-year history of muscular dystrophy is hospitalized with a respiratory tract infection. Which nursing action will be included in the plan of care?
A. Logroll the patient every 1 to 2 hours.
B. Teach the patient about the muscle biopsy procedure.
C. Provide the patient with a pureed diet.
D. Assist the patient with active range-of-motion (ROM) exercises.
Answer: D
Rationale: The goal for the patient with muscular dystrophy is to keep the patient active for as long as possible. The patient would not be confined to bed rest and would not require logrolling. Muscle biopsies are necessary to confirm the diagnosis but would not be ordered for a patient who already had a diagnosis. There is no indication that the patient requires a pureed diet.
The wound irrigation process cleanses the wound and:
1) Reduces the potential of pain in the wound region or area.
2) Stops the spread of infection by way of magnifying the “clean” area.
3) Pushes extravasated blood from a hematoma into nearby healthy tissue.
4) Allows for the introduction of medications in solution form.
4
Of all the choices above, the only correct fact about wound irrigation is that it allows the application of medications in solution. Introducing prescribed medications in solution form can dramatically reduce infection risks and facilitating proper wound heal. Unfortunately, the irrigation process can greatly increase the pain in a wound area. Wound irrigation can reduce the spread of infection, but not by increasing the area cleaned. The complications resulting by a hematoma are reduced through wound irrigation and not by pushing into other tissue.
The nurse is monitoring an older client suspected of having a urinary tract infection (UTI) for signs of infection. Which sign/symptom is likely to present first?
A) Fever
B) Urgency
C) Confusion
D) Frequency
C
Rationale: In an older client, the only symptom of a UTI may be something as vague as increasing mental confusion or frequent unexplained falls. Frequency and urgency may commonly occur in an older client, and fever can be associated with a variety of conditions.
Test-Taking Strategy: Note the strategic word, first
The nurse is monitoring for stoma prolapse in a client with a colostomy. Which stoma observation should indicate that a prolapse has occurred?
A) Dark and bluish
B) Sunken and hidden
C) Narrowed and flattened
D) Protruding and swollen
D
Rationale: A prolapsed stoma is one in which bowel protrudes through the stoma, with an elongated and swollen appearance. A stoma retraction is characterized by sinking of the stoma. Ischemia of the stoma would be associated with dusky or bluish color. A stoma with a narrowed opening, either at the level of the skin or fascia, is said to be stenosed.
The nurse is assisting to perform a focused data collection process on a client who is complaining of symptoms of a cold, a cough, and lung congestion. Which should the nurse include for this type of data collection? Select all that apply.
1. Listening to lung sounds
2. Obtaining the client’s temperature
3. Checking the strength of peripheral pulses
4. Obtaining information about the client’s respirations
5. Performing a musculoskeletal and neurological examination
6. Asking the client about a family history of any illness or disease
- 1, 2, 4
Rationale: A focused data collection process is centered around a limited or short-term problem, such as the client’s complaint. Because the client is complaining of symptoms of a cold, a cough, and lung congestion, the nurse would focus on the respiratory system and the presence of an infection. A complete data collection includes a complete health history and physical examination and forms a baseline database. Checking the strength of peripheral pulses relates to a vascular assessment, which is not related to this client’s complaints. A musculoskeletal and neurological examination also is not related to this client’s complaints. However, strength of peripheral pulses and a musculoskeletal and neurological examination would be included in a complete data collection. Likewise, asking the client about a family history of any illness or disease would be included in a complete assessment.
The nurse is assigned to care for four clients. When planning client rounds, which client should the nurse check first?
A) A client in skeletal traction
B) A client who is dependent on a ventilator
C) A postoperative client preparing for discharge
D) A client admitted during the previous shift with a diagnosis of gastroenteritis
B
Rationale: The airway is always a priority, and the nurse first checks the client on a ventilator. The clients described in options 1, 3, and 4 have needs that would be identified as intermediate priorities.
Test-Taking Strategy: Note the strategic word, first. Use ABCs—airway, breathing, and circulation—to answer the question. Remember that the airway is always the first priority.
The nurse is checking the casted extremity of a client. The nurse should check for which sign indicative of infection?
A) Dependent edema
B) Diminished distal pulse
C) Presence of a “hot spot” on the cast
D) Coolness and pallor of the extremity
C
Rationale: Signs and symptoms of infection under a casted area include odor or purulent drainage from the cast or the presence of “hot spots,” which are areas of the cast that are warmer than others. The PHCP should be notified if any of these occur. Signs of impaired circulation in the distal limb include coolness and pallor of the skin, diminished arterial pulse, and edema.
Test-Taking Strategy: Note the subject, a sign of infection.
Which action by the novice nurse indicates need for further teaching?
A. A nurse fails to wear gloves to remove a dressing
B. The nurse applies the oxygen saturation monitor to the earlobe
C. The nurse elevates the head of the bed to check blood pressure
D. The nurse places the extremity to a dependent position to acquire a peripheral blood sample
A. A nurse fails to wear gloves to remove a dressing
The nurse who fails to wear gloves to remove a contaminated dressing needs further instruction
The nurse is inserting an indwelling urinary catheter into a male client. As the catheter is inserted into the urethra, urine begins to flow into the tubing. When should the nurse inflate the balloon?
A) Immediately inflate the balloon.
B) Insert the catheter 2.5 cm to 5 cm and inflate the balloon.
C) Advance the catheter an additional 1 to 2 inches
D) Insert the catheter until resistance is met and inflate the balloon.
C
(see skills pg. 561)
Rationale: Urinary catheterization is a sterile procedure. When inserting an indwelling catheter, the nurse should ensure the balloon is in the bladder before inflating it. If the balloon is inflated in the urethra of the male client, trauma may occur. When catheterizing a male client, the nurse observes the tubing for the flow of urine and then continues to advance the catheter an additional 1 to 2 inches then inflates the balloon. The nurse then pulls the catheter back until slight resistance is felt and applies a tube holder onto the thigh to hold the catheter in place. The balloon should not be inflated when urine is first observed, after advancing several more centimeters or when resistance is felt.
Test-Taking Strategy: Focus on the subject when to inflate the balloon when inserting an indwelling urinary catheter in a male client.
As the nurse prepares to assist Mrs. P with her newly created Ileostomy, She is aware of which of the following?
A) An appliance will not be required on the continual basis
B) The size of the stoma stabilizes within two weeks
C) Irrigation is necessary for regulation
D) Fecal drainage will be liquid
D) Fecal drainage will be liquid
Bowel appliance is usually required on a continual basis because the fecal drainage is liquid.
Stomas size usually stabilizes within 4 to 6 weeks,
Ileostomy Irrigation is not necessary because fecal matter is liquid
During which phase of the nursing process does data get collected and validated with the patient and/or family members by the nurse?
1) The implementation phase
2) The assessment phase
3) The evaluation phase
4) The planning phase
2
Subjective, objective, primary and secondary data is collected and validated with the patient and/or family members by the nurse during the assessment phase of the nursing process. The implementation phase is the actual care of the patient; the evaluation phase includes the comparison of current data to expected outcomes to determine if the patient has achieved the pre-established goals and the planning phase consists of priority setting and care planning.
A nurse is caring for a male client immediately after removal of the endotracheal tube. The nurse reports which of the following signs immediately if experienced by the client?
a. Stridor
b. Occasional pink-tinged sputum
c. A few basilar lung crackles on the right
d. Respiratory rate of 24 breaths/min
A.
The nurse reports stridor to the physician immediately. This is a high-pitched, coarse sound that is heard with the stethoscope over the trachea.
Stridor indicates airway edema and places the client at risk for airway obstruction
The nurse has provided instructions regarding specific leg exercises for the client immobilized in right skeletal lower leg traction. The nurse determines that the client needs further teaching if the nurse observes the client doing which activity?
A) Pulling up on the trapeze
B) Flexing and extending the feet
C) Doing quadriceps-setting and gluteal-setting exercises
D) Performing active range of motion (ROM) to the right ankle and knee
D
Rationale: Exercise is indicated within therapeutic limits for the client in skeletal traction to maintain muscle strength and ROM. The client may pull up on the trapeze, perform active ROM with uninvolved joints, and do isometric muscle-setting exercises (e.g., quadriceps- and gluteal-setting exercises). The client may also flex and extend his or her feet. Performing active ROM to the affected leg can be harmful.
Test-Taking Strategy: Note the strategic words, needs further teaching.
138. The nurse is caring for a postoperative client who has a Jackson-Pratt drain inserted into the surgical wound. Which actions should the nurse take in the care of the drain? Select all that apply.
1. Check the drain for patency.
2. Check that the drain is decompressed.
3. Observe for bright red, bloody drainage.
4. Maintain aseptic technique when emptying.
5. Empty the drain when it is half full and every 8 to 12 hours.
6. Secure the drain by curling or folding it and taping it firmly to the body.
1, 2, 3, 4, 5
Rationale: A drain is a tube that is placed to drain out fluid and blood near the surgical site and could lead to infection. The tube is connected to a bulb, which is compressed to create a vacuum and pull out the fluid. The nurse should check for patency and that fluid is being pulled out. The bulb should be, and look, decompressed in order to create the vacuum. The drainage usually is dark red as a result of blood content, but may be pale yellow with serous fluid. Aseptic technique must be used when emptying the drainage container to avoid contamination of the wound. The bulb of the drain should be emptied when it is half full and at least every 8 to 12 hours. The amount of drainage is documented in the client medical record under intake and output. Curling or folding the drain prevents the flow of the drainage.
Test-Taking Strategy: Focus on the subject, caring for a surgical drain.
The nurse is teaching an older female patient how to manage stress incontinence at home. She instructs her to contract her pelvic floor muscles for at least 10 seconds followed by a brief period of relaxation. What is this intervention called?
A) Prompted voiding
B) Crede technique
C) Valsalva maneuver
D) Kegel exercises
D Kegel exercises
Rationale:
Kegel exercises strengthen the pelvic floor muscles that support the uterus, bladder, and bowel. Doing Kegel exercises regularly can reduce urinary incontinence. These exercises involve tightening and relaxing the muscles around the vaginal area.
Prompted voiding is a part of a bladder-training program in which the person learns to void based on a schedule, rather than to empty the bladder.
The Crede technique is applying manual pressure with your hands to the top portion of the bladder to initiate a urine flow.
The Valsalva is the maneuver in which a person tries to exhale forcibly with a closed glottis (the windpipe) so that no air exits through the mouth or nose, for example, in strenuous coughing, straining during a bowel movement, or lifting a heavy weight.
Your patient complains of an excessive flatulence. When reviewing your patients dietary intake, which foods, if eaten regularly, would you identify as possibly responsible?
A) Meat
B) Cauliflower
C) Potatoes
D) Ice cream
B
Cauliflower is a gas producing food that relates in flatulence
What is the name of this assessment procedure
Auscultation
Can you also name the other three assessment processes
Inspection
Palpation
Percussion
A nurse is suctioning fluids from a female client through an endotracheal tube. During the suctioning procedure, the nurse notes on the monitor that the heart rate is decreasing. Which of the following is the appropriate nursing intervention?
a. Continue to suction.
b. Notify the physician immediately.
c. Stop the procedure and reoxygenate the client.
d. Ensure that the suction is limited to 15 seconds.
C.
During suctioning, the nurse should monitor the client closely for side effects, including hypoxemia, cardiac irregularities such as a decrease in heart rate resulting from vagal stimulation, mucosal trauma, hypotension, and paroxysmal coughing. If side effects develop, especially cardiac irregularities, the procedure is stopped and the client is reoxygenated.
The nurse is preparing a list of cast care instructions for a client who just had a plaster cast applied to his right forearm. Which instructions should the nurse include on the list? Select all that apply.
1. Keep the cast and extremity elevated.
2. The cast needs to be kept clean and dry.
3. Allow the wet cast 24 to 72 hours to dry.
4. Expect tingling and numbness in the extremity.
5. Use a hair dryer set on a warm to hot setting to dry the cast.
6. Use a soft-padded object that will fit under the cast to scratch the skin under the cast.
1,2,3
Rationale: A plaster cast takes 24 to 72 hours to dry (synthetic casts dry in 20 minutes). The cast and extremity may be elevated to reduce edema. A wet cast is handled with the palms of the hands until it is dry, and the extremity is turned (unless contraindicated) so that all sides of the wet cast will dry. A cool setting on the hair dryer can be used to dry a plaster cast (heat cannot be used because the cast heats up and burns the skin). The cast needs to be kept clean and dry, and the client is instructed not to stick anything under the cast because of the risk of breaking skin integrity. The client is instructed to monitor the extremity for circulatory impairment such as pain, swelling, discoloration, tingling, numbness, coolness, or diminished pulse. The PHCP is notified immediately if circulatory impairment occurs.
Test-Taking Strategy: Focus on the subject, a plaster cast.
True or False
All wounds should be closed and bandaged to promote healing.
False
Some wounds should be left open to heal instead of bringing the edges together. These include some animal bites and large wounds that are contaminated. Leaving these wounds open helps prevent infection. A bandage usually is not necessary unless the wound is in an area that will get dirty or rub on clothing.
A client has just voided 50 mL, but reports that his bladder still feels full. The nurse's next actions should include: (Select all that apply.)
1) palpating the bladder height.
2) obtaining a clean-catch urine specimen.
3) performing a bladder scan.
4) asking the patient about his recent voiding history.
5) encouraging the patient to consume cranberry juice daily.
6) inserting a straight catheter to measure residual urine.
1) Palpating the bladder height.
3) Performing a bladder scan.
4) Asking the patient about his recent voiding history.
Rationale:
The nurse should palpate the bladder for distention.
A bladder scan will yield a more accurate measurement of the postvoid residual urine. A detailed history of the client's recent voiding patterns will assist the nurse in determining the appropriate nursing diagnosis and developing a plan of care.
A clean-catch urine specimen may be necessary if further assessment shows the potential of a urinary tract infection.
Cranberry juice is sometimes used to in an effort to prevent urinary tract infection, although there is conflicting research to support this action.
Inserting a straight catheter to measure residual urine is an invasive procedure with the risk of introducing microorganisms into the bladder and is usually unnecessary if the nurse has access to a portable bladder scanner.
The nurse is assessing a patient who underwent bowel resection 2 days ago. As she auscultates the patient's abdomen, she notes low-pitched, infrequent bowel sounds. How should she document this finding?
1) Hyperactive bowel sounds
2) Abdominal bruit sounds
3) Normal bowel sounds
4) Hypoactive bowel sounds
4) Hypoactive bowel sounds
Rationale:
Hypoactive bowel sounds are low pitched, infrequent, and quiet. An abdominal bruit is a hollow, blowing sound found over an artery, such as the iliac artery. Normal bowel sounds are high pitched, with approximately 5 to 35 gurgles occurring every minute. Hyperactive bowel sounds are very high pitched and more frequent than normal bowel sounds.
The mnemonic “PERRLA” is useful for the assessment of the eyes. What does PERRLA stand for?
1) Pupils equal, round, reactive to light and accommodation
2) Patient eyes are equal, round, recessed and responsive to light and acuity
3) Patient eyes are equal, reactive,responsive to light and acuity
4) Pupils equal, round, reactive to light and acuity
The mnemonic “PERRLA” stands for
1) pupils equal round, reactive to light and accommodation,
not acuity. Visual acuity is tested with the Snellen Chart among adult patients.
Name the 44th, 43rd, 42nd, 41st, and 40th President of the United States
Obama 44
W Bush 43
Clinton 42
HW Bush 41
Reagan 40
Just random knowledge for Trivia game night
During the physical assessment of a young adult, the nurse notes a lateral, S-shaped curve of the spine. What should the nurse suspect is occurring w this pt?
a. lordosis
b. scoliosis
c. kyphosis
d. musculosis
B
reference the book
Which of the following are functions of dressings? (select all that apply)
A. promote hemostasis
B. keep wound bed dry
C. wound debridement
D. prevent contamination
E. increase circulation
A. promote hemostasis
C. wound debridement
D. prevent contamination
We don't want to keep the wound bed dry and dressings don't increase circulation
Which urinary system structure is largely responsible for storing urine?
1) Kidney
2) Bladder
3) Ureters
4) Nephrons
2) Bladder
Rationale:
The urinary bladder is a sac-like organ that receives urine from the ureters and stores it until discharged from the body.
The kidneys filter metabolic wastes, toxins, excess ions, and water from the bloodstream and excrete them as urine.
The ureters transport urine.
The nephrons form urine.
KiKi (KeKe) Doesn't love Drake (why)
Because Drake only loves his bed and his mom
Which of the following assessment tools is used to determine the patients’ level of consciousness?
1) The Snellen Scale
2) The Norton Scale
3) The Morse Scale
4) The Glasgow Scale
4
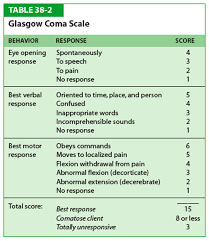
The Glasgow Scale assesses for altered levels of consciousness. The Snellen chart, not scale, is used to assess and measure visual acuity; the Norton Scale assesses patients’ risk for skin breakdown; the Morse Scale assesses patients’ risk for falls.
A male client is admitted to the health care facility for treatment of chronic obstructive pulmonary disease. Which nursing diagnosis is most important for this client?
a. Activity intolerance related to fatigue
b. Anxiety related to actual threat to health status
c. Risk for infection related to retained secretions
d. Impaired gas exchange related to airflow obstruction
D
A patent airway and an adequate breathing pattern are the top priority for any client, making impaired gas exchange related to airflow obstruction the most important nursing diagnosis. The other options also may apply to this client but are less important.
Who was the better TV family
The Brady Bunch
Different Strokes
Facts of Life
The Simpsons
It all depends so hey any answer is correct
What term refers to pale, red and watery drainage from a wound?
A. serous
B. sanguineous
C. serosanguineous
D. purulent
C. serosanguineous
serous - clear, watery, plasma
sanguineous - bright red, active bleeding
purulent - thick, yellow, green, tan or brown (pus)
Data must be collected to evaluate the effectiveness of a plan to reduce urinary incontinence for a older adult patient. Of the information below, which is the least important for the evaluation process?
A) The incontinence pattern
B) State of physical mobility
C) Medications being taken
D) Age of patient
D) Age of patient
Incontinence is not a natural consequence of the aging process. All the other factors are necessary information for the plan of care.
A patient starts to experience pain while receiving an enema. The nurse notes blood in the return fluid and rectal bleeding. What action does the nurse take first?
a. Administers pain medication
b. Slows down the rate of instillation
c. Tells the patient to breathe slowly and relax
d. Stops the instillation and obtains vital signs
D
Tell us why D is correct
Which technique or method is used to determine whether or not the patient has an irregular pulse?
1) Apical pulse
2) Inspection
3) Auscultation
4) Percussion
3
Auscultation is listening to the sounds of the body, particularly the apical pulse for rate and irregularity, using a stethoscope. Inspection is the purposeful and systematic visual inspection and examination of the client. The palpation technique employs the nurse’s sense of touch. Percussion is performed by striking the client’s body in order to determine what sounds and vibrations their body will produce.
The nurse is caring for a male client who recently underwent a tracheostomy. The first priority when caring for a client with a tracheostomy is:
a. helping him communicate.
b. keeping his airway patent.
c. encouraging him to perform activities of daily living.
d. preventing him from developing an infection.
B.
Maintaining a patent airway is the most basic and critical human need. All other interventions are important to the client's well-being but not as important as having sufficient oxygen to breathe.
What Chapter of your NCLEX-PN should be read for test taking tips.
Chp 4
This form of wound debridement is the removal of devitalized tissue by using a scalpel, scissors, or other sharp instruments.
A) Chemical
B) Mechanical
C) Sharp
D) Autolytic
C
Sharp
(see pg. 768 in the book for detail Oh yeah)

The client is scheduled for a pericentesis. Which instruction should be given to the client before the exam?
A. "You will need to lay flat during the exam."
B. "You need to empty your bladder before the procedure."
C. "You will be alseep during the procedure."
D. "The doctor will injuect a medication to treat your illness during the procedure."
B. "You need to empty your bladder before the procedure."
The client scheduled for a pericentesis should be told to empty the bladder, to prevent the risk of puncturing the bladder when the needle is inserted. A pericentesis is done to remove fluid from the peritoneal cavity.
The nurse is assessing a patient 2 hours after a colonoscopy. Based on the procedure done, what focused assessment will the nurse include?
a. Bowel sounds
b. Presence of flatulence
c. Bowel movements
d. Nausea
A
Explain why